A Rare Presentation of Gall Bladder (GB) Mass in the Form of Mixed Adenoneuroendocrine Carcinoma (MANEC): A Case Report
Rishikant Sinha1, Pranav Kumar Santhalia2, Prem Kumar3, Punam Prasad Bhadani4
1 Senior Resident, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
2 Assistant Professor, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
3 Professor, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
4 Professor, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Rishikant Sinha, Flat Number 201, Basudev Bihar Apartment, Nageshwar Colony, Parmanand Path, Patna, Bihar, India.
E-mail: drrishikantsinha@gmail.com
Primary Neuroendocrine Carcinoma (NEC) of gall bladder is extremely rare. The diagnosis is incidental in most cases. Here, we present a case of Mixed Adenoneuroendocrine tumour (MANEC) in a 48-year-old female who presented with pain in abdomen, nausea and loss of appetite and diffuse non-tender lump in right hypochondrium. CECT abdomen showed distended Gall Bladder (GB) with intraluminal polypoidal mass, with multiple liver and retroperitoneal metastasis. Histopathological and immunohistochemistry study revealed MANEC in GB with NEC metastasis in liver. This case highlights the rarity of the disorder and role of immunohistochemical studies and therefore MANEC should be considered as a differential to GB carcinoma.
Gall bladder, Immunohistochemistry, Malignant
Case Report
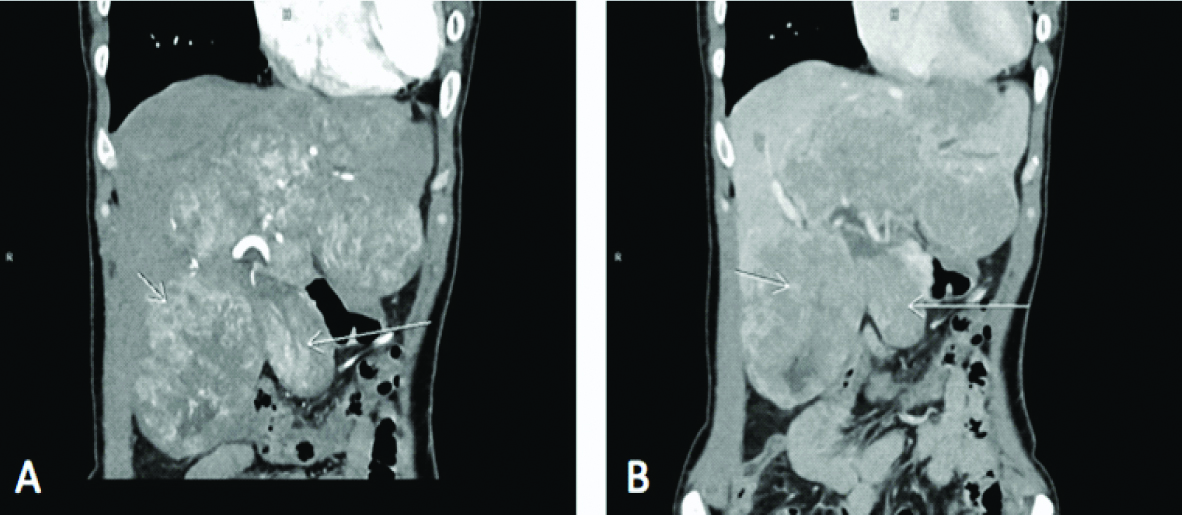
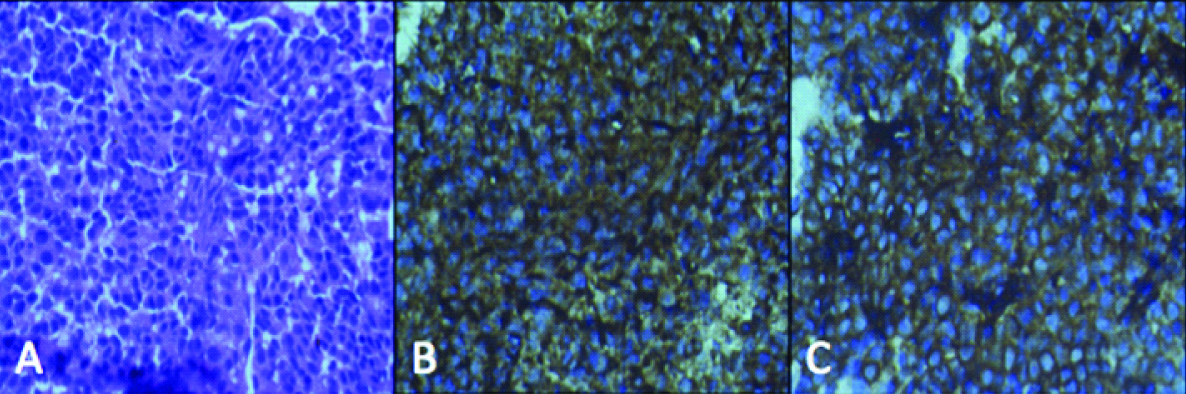
A 48-year-old female with complaints of pain in abdomen, on and off nausea and loss of appetite since one month presented to the department. Laboratory investigation revealed elevated SGOT (511 U/L), SGPT (93 U/L), ALP (1350 U/L), direct serum bilirubin (2.11 mg/dL), total serum bilirubin (2.91 md/dL) with normal HbsAg and Anti HCV. On clinical examination an approximately 11×10 cm, diffuse non-tender lump was noted in right hypochondrium, which extended to the epigastrium and umbilical region and was moving with respiration. Chest X-Ray was normal. Ultrasound (USG) showed multiple hypoechoic lesions in liver. Triple phase CECT abdomen was done which showed distended GB with intraluminal polypoidal mass, with multiple liver Space Occupying Lesions (SOL) and retroperitoneal enlarged nodes [Table/Fig-1]. Patient was admitted with provisional diagnosis as carcinoma GB with liver and nodal metastasis. Guided TRU cut biopsy from liver lesions and FNAC from polypoidal mass of GB lumen was done. Histopathological examination of liver biopsy showed tumour arranged in sheets, perivascular rosseting and focal organoid pattern. The individual tumour cells showed hyperchromatic nuclei, increased nucleus to cytoplasmic ratio (N:C) and moderate amount of eosinophilic cytoplasm. IHC study showed diffuse strong positive in tumour cells for cytokeratin, synaptophysin, chromogranin A, CD56 and CDX-2, 65% for Ki-67 and negative for CK7 and CK20 suggesting neuroendocrine carcinoma [Table/Fig-2]. FNAC from GB mass showed atypical cells arranged in papillaroid clusters sheets, gland formation and singly scattered. The cells showed moderate nuclear pleomorphism, high N:C ratio, suggestive of adenocarcinoma with focal neuroendocrine features.
CECT of abdomen, Coronal sections, (a) shows distended GB with intraluminal polypoidal mass (large arrow) and multiple well-defined lobulated intrahepatic masses (small arrow) of varying sizes with moderate heterogeneous enhancement on arterial phase and washout on venous phase (b).
Tumour cells stain positive for cytokeratin (a), chromogranin (b) and synaptophysin (c).
Discussion
Neuroendocrine Tumours (NETs) previously known as carcinoid tumours are neoplasm of enterochromaffin/neuroendocrine cell origin, with neurosecretory capacity [1,2]. Neuroendocrine neoplasms are classified according to the WHO Classification of Tumours of the Digestive System in 2010 as well-differentiated, low-grade (G1); well-differentiated, intermediate-grade (G2); and poorly differentiated, high-grade (G3) [3]. Carcinoid tumours are quite unusual endocrine tumours arising mainly in the gastrointestinal tract. The site for primary carcinoid is appendix, jejunum and rectum in most of the cases. Primary GB carcinoid are extremely rare, till date only 278 cases of GB NETS are reported in the Surveillance, Epidemiology, and End Results (SEER) database. The age of presentation ranges from 38 to 81 years with marked higher incidence in women and it corroborates with our case [4]. NETs of GB probably originate from a multipotent stem cell or from endocrine cells induced by intestinal metaplasia of the body and fundus as well as from pre-existing endocrine cells in the neck of the GB, which occurs following cholelithiasis and/or chronic inflammation [1].
Neuroendocrine carcinoma is frequently combined with other tumours such as adenocarcinoma or squamous cell carcinoma. MANEC is diagnosed only when both tumour types are more than 30% in the pathological examination [5].
The imaging modalities like USG, CT and MRI, cannot distinguish GB-NEC from other gall bladder carcinomas. The radiological findings are similar to presentations of any other GB tumour. MRI is the modality of choice in staging GB tumours and when combined with MRCP, gives full overview of biliary radicles invasion. Sensitivities are as high as 100% and 92% for direct hepatic invasion and lymph nodes invasion on MRI respectively [6]. Diagnosis is generally made on pathological and immune histochemical examinations.
NEC also invades the adjacent liver parenchyma and cause biliary obstruction, thus making it difficult to diagnose at an early stage. Due to the nature of NECs, patients are often diagnosed at an advanced stage with lymph node metastasis or liver infiltration, and have a poor prognosis [3,7]. Since there is no characteristic imaging finding to suspect this tumour and it is almost impossible to differentiate it from other subtypes of gall bladder tumour, only postoperative diagnosis was done previously. But now-a-days, TRU cut biopsy from lesion is rampantly done under ultrasound guidance and preoperative diagnosis is possible and it helps in better management of the cases. GB NETs treatment comprises of multidisciplinary approach including surgery, chemotherapy and radiotherapy. In patients in advanced stages without distal metastasis, radical cholecystectomy and lymphadenectomy combined with hepatic resection are done [3]. Systemic chemotherapy is the treatment of choice in case of unresectable tumours.
Conclusion
The findings of NEC are similar to presentations of any other GB tumour. So its specific diagnosis on imaging is difficult. USG is the initial modality of choice in diagnosis GB tumours. Multiphasic CECT, MRI, and PET-CT are imaging which helps in further characterising and staging of tumours. Radical surgery with adjuvant chemotherapy is the main line of treatment in patients without metastatic disease. This case highlights the rarity of the disorder and role of preoperative USG guided TRU cut biopsy and immunohistochemical studies in diagnosis of MANEC.
[1]. Eltawil KM, Gustafsson BI, Kidd M, Modlin IM, Neuroendocrine tumours of the gallbladder: an evaluation and reassessment of management strategyJ Clin Gastroenterol 2010 44:687-95.10.1097/MCG.0b013e3181d7a6d420375728 [Google Scholar] [CrossRef] [PubMed]
[2]. Zuetenhorst JM, Taal BG, Metastatic carcinoid tumours: a clinical reviewOncologist 2005 10::123-31.doi: 10.1634/theoncologist.10-2-12310.1634/theoncologist.10-2-12315709214 [Google Scholar] [CrossRef] [PubMed]
[3]. Bosman FTCF, Hruban RH, Theise ND, World Health Organization (WHO) Classification of Tumours of the Digestive System 2010 Geneva, SwitzerlandWHO Press [Google Scholar]
[4]. Modlin IM, Shapiro MD, Kidd M, An analysis of rare carcinoid tumours: clarifying these clinical conundrumsWorld J Surg 2005 29:92-101.10.1007/s00268-004-7443-z15599742 [Google Scholar] [CrossRef] [PubMed]
[5]. Deehan DJ, Heys SD, Kernohan N, Eremin O, Carcinoid tumour of the gall bladder: two case reports and a review of published worksGut 1993 34:1274-76.10.1136/gut.34.9.12748406168 [Google Scholar] [CrossRef] [PubMed]
[6]. Gallbladder , In: Edge SB, Byrd DR, Compton CC, et al. (eds.): AJCC Cancer Staging Manual 2010 7thedNew York, NYSpringer:211-17.10.1007/978-0-387-88441-7_20 [Google Scholar] [CrossRef]
[7]. Albores-Saavedra J, Batich K, Hossain S, Henson DE, Schwartz AM, Carcinoid tumours and small-cell carcinomas of the gallbladder and extrahepatic bile ducts: a comparative study based on 221 cases from the Surveillance, Epidemiology, and End Results ProgramAnn Diagn Pathol 2009 13:378-83.10.1016/j.anndiagpath.2009.08.00219917473 [Google Scholar] [CrossRef] [PubMed]