The intimate anatomical relationship between the Inferior Alveolar Nerve (IAN) and the IMTM is a major concern for planning of surgical removal of the tooth as the nerve has a high potential to be injured following the procedure. Injury to this nerve will lead to sensory disturbance to all mandibular teeth of the affected quadrant and other adjacent structures innervated by the nerve. These include the ipsilateral side of the lower lip and chin, as well as, the gingivae that surrounds the buccal surface of the premolars and the labial surface of the anterior teeth. The frequency of IAN paraesthesia ranges between 0.4% and 8.4% [1] while the permanent numbness is shown to be less than 1% [2].
Understanding the risk of MC exposure would help the clinician in providing appropriate informed consent, justification of further radiographic investigation, as well as treatment decision for the patient.
The risk of MC exposure by IMTM may be assessed using various radiographic methods. To date, CBCT has been proven to be the most accurate modality in the prediction of the presence or absence of MC exposure in IMTM cases [3] although panoramic radiograph still remains as the imaging modality of choice. In CBCT image evaluation, the presentation of MC exposure may be marked by loss of radiopaque cortex of the canal by the IMTM’s root [4].
It is important to understand the risk of MC exposure by IMTM from the panoramic radiograph since it is more commonly used as the first line radiographic approach due to its availability, lower radiation dose and effective cost.
Seven radiological markers from the panoramic radiograph which suggest close proximity of IMTM to the MC have been described since the early study by Rood JP et al., [5]. These markers are interruption of white line(s), deviation of MC, narrowing of MC, narrowing of the root, deflection of the root, darkening of the root, as well as, dark and bifid root. Interruption of white line(s) indicates the disruption of the cortical lining the MC by the IMTM. This marker is significantly associated with high risk of MC exposure [3-7]. It is questionable whether the finding remains similar when the interruption regions of the white line is taken into consideration in the risk assessment of MC exposure by IMTM.
Darkening of the root implies the reduction in the root density as a result of impingement of MC to the root of IMTM. Meanwhile, dark and bifid root implies impingement of MC to the bifid root apex of IMTM. Narrowing of the root signifies deep grooving of the IMTM root where the MC crosses it. Deflected root implies deviation of the root when it reaches the MC. When panoramic radiograph demonstrates changes in the IMTM root appearance, only darkening of the root commonly demonstrates significant association with high risk of MC exposure [3-7]. It is questionable whether the rest of the markers still demonstrate insignificant finding if there is involvement of more than one root. Thus, there is a need to explore the type of markers based on the interruption regions of white line and number of root (s) involve and investigate their significance in relation to the risk of MC exposure.
Deviation of MC implies the change in the direction of MC when it crosses the IMTM. Whereas, narrowing of MC implies decrease of MC diameter when it crosses the tooth. While deviation of MC commonly demonstrates significant association with high risk of MC exposure [3,4,6,7], narrowing of the canal was considered to indicate MC exposure when appear with interruption of the white line [5]. This finding suggested that the number of marker may affect the risk assessment of MC exposure by IMTM. Therefore, apart of the type of markers originally described by Rood JP et al., that need to be further explored, the number of markers present also requires attention in the risk assessment of MC exposure by IMTM [5]. Studies were performed to predict MC exposure based on the type and number of panoramic radiological markers [3,4,6,7]. All of these studies followed Rood and Shehab in the classification of panoramic markers. The expansion of the type of panoramic markers described by Rood and Shehab into 15 categories is the first ever study which possibly entails new insight in the risk assessment of MC exposure by IMTM from panoramic radiograph. The aim of this study was to investigate each of the 15 type of panoramic radiological markers and number of markers in relation to the risk of the MC exposure by IMTM.
Materials and Methods
Study Design
This retrospective cross-sectional study was conducted at Faculty of Dentistry, Universiti Kebangsaan Malaysia from February 2015 until February 2018 following approval by the Research Ethics Committee, Universiti Kebangsaan Malaysia (UKM 1.5.3.5/244/DD/2015/02). Determination of the sample size was performed using the Open Epi software [8]. We made an assumption based on our annual patient’s attendance in the Oral and Maxillofacial Surgery Clinic, Faculty of Dentistry, UKM that stood approximately 300 cases per year. By using 56.7% prevalence of mandibular third molar impaction [9], hence at 95% confidence interval, the estimated number that needed to be sampled with 10% drop out rate was 185 patients.
In this study, the sample composed of paired panoramic radiographs and CBCT images of 188 IMTMs which were obtained between 2012 to 2016. Panoramic radiographs were acquired as primary radiographic investigation of the IMTM. When ever there was suspicion of MC exposure by an IMTM from panoramic radiograph, further assessment with CBCT image was performed for better insight of the relationship between the IMTM and MC. These were gathered from the image archives in the Radiology Unit, Faculty of Dentistry, Universiti Kebangsaan Malaysia. The CBCT images were selected first from the archives, followed by the digital panoramic radiographs of the same subjects. The inclusion criteria for this study were patients 18-year-old and above, panoramic radiograph which showed two roots-IMTMs, and presence of fully visible IMTMs as well as visible MC. Radiographic records of IMTM with more or less than two roots, incomplete root formation, or with pathological evidence were excluded from this study.
Radiographic Evaluation
A calibration phase between the oral and maxillofacial radiologist and the oral and maxillofacial surgeon in the image evaluation was performed using 30 panoramic radiographs and 30 CBCT images of the IMTMs. Once adequate inter-observer agreement was achieved, the subsequent image evaluation was performed by the oral and maxillofacial radiologist alone. Cohen’s kappa coefficient value was used to determine the inter-observer agreement. Value of Cohen’s kappa ranges from -1 to 1. Values less than 0 indicate no agreement. Value within the range of 0.01-0.2 is indicated as slight agreement, 0.24-0.4 as fair, 0.41-0.6 as moderate, 0.61-0.8 as substantial and 0.81-1 as excellent agreement.
All images were evaluated on a standardised computer monitor (22’’ Barco MDRC-2122BL clinical display). Assessment of the IMTM and MC of each panoramic radiograph was made using the image displayed on the computer monitor. Assessment of the CBCT images was performed using the reconstructed panoramic views as well as cross-sectional views on the computer monitor. The relationship between the IMTM and MC was assessed in all the reconstruction planes on all the slices.
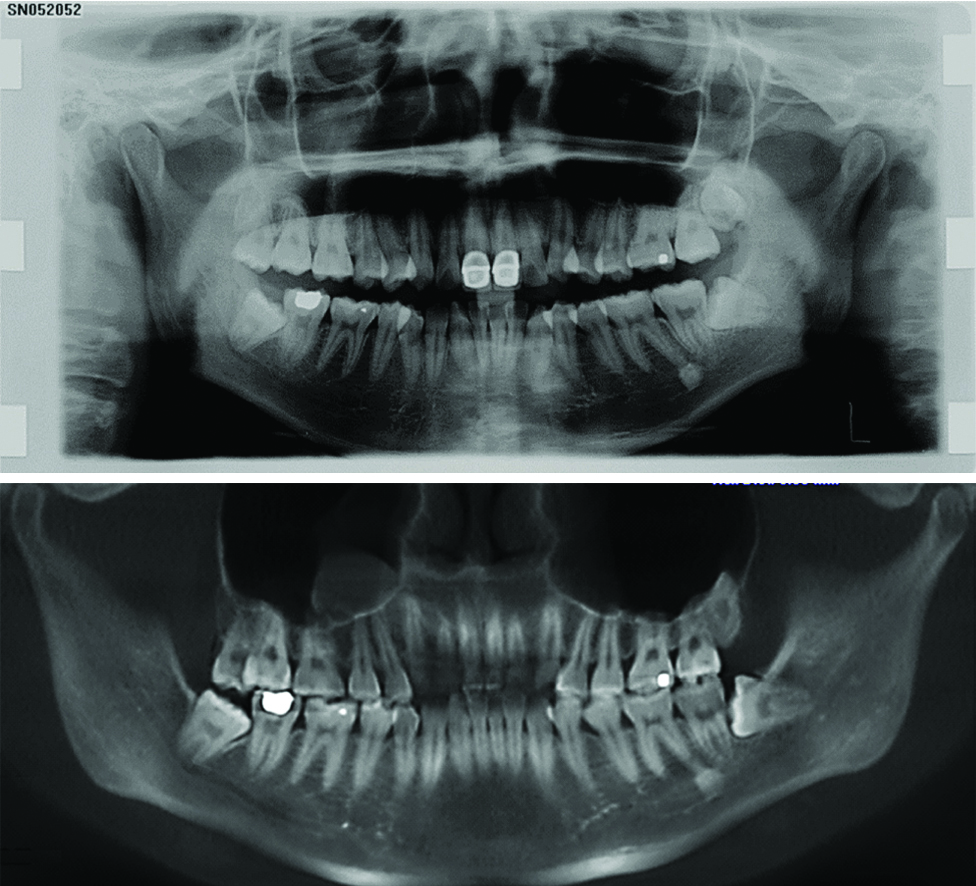
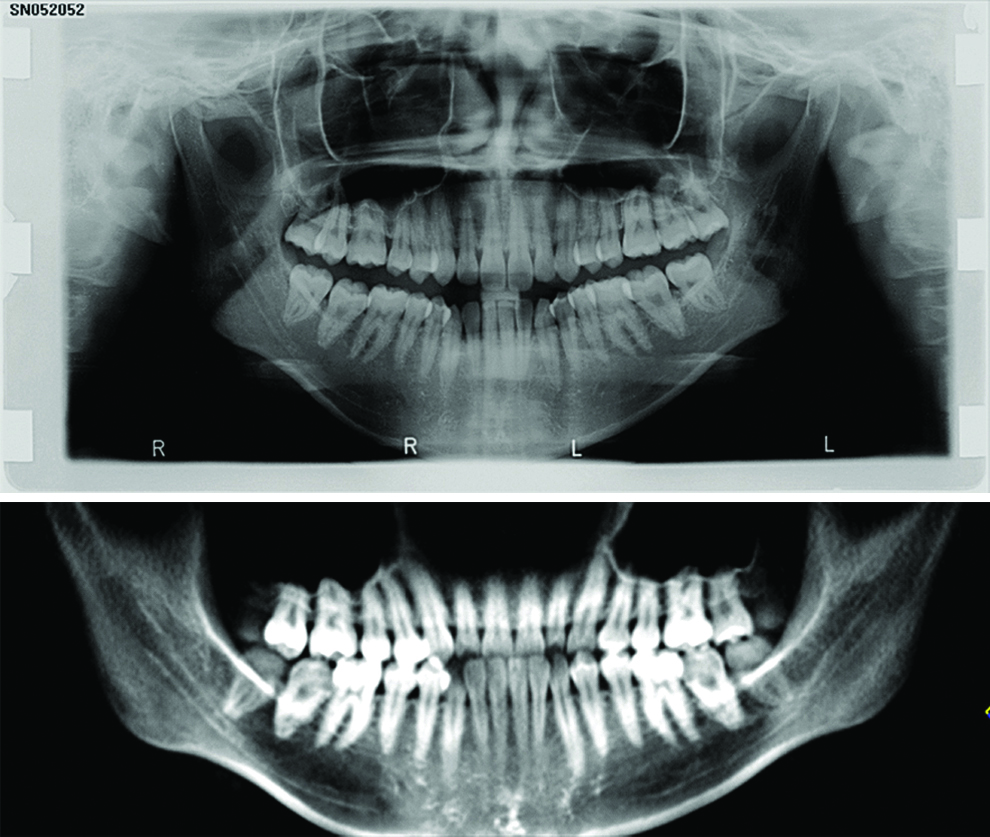
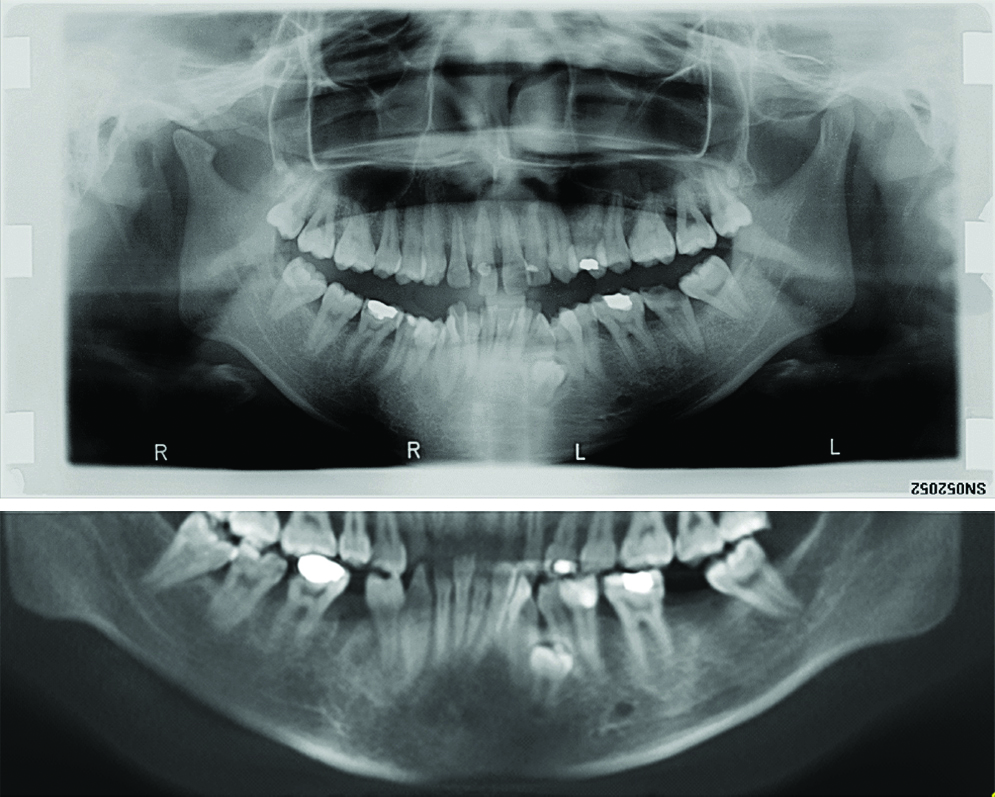
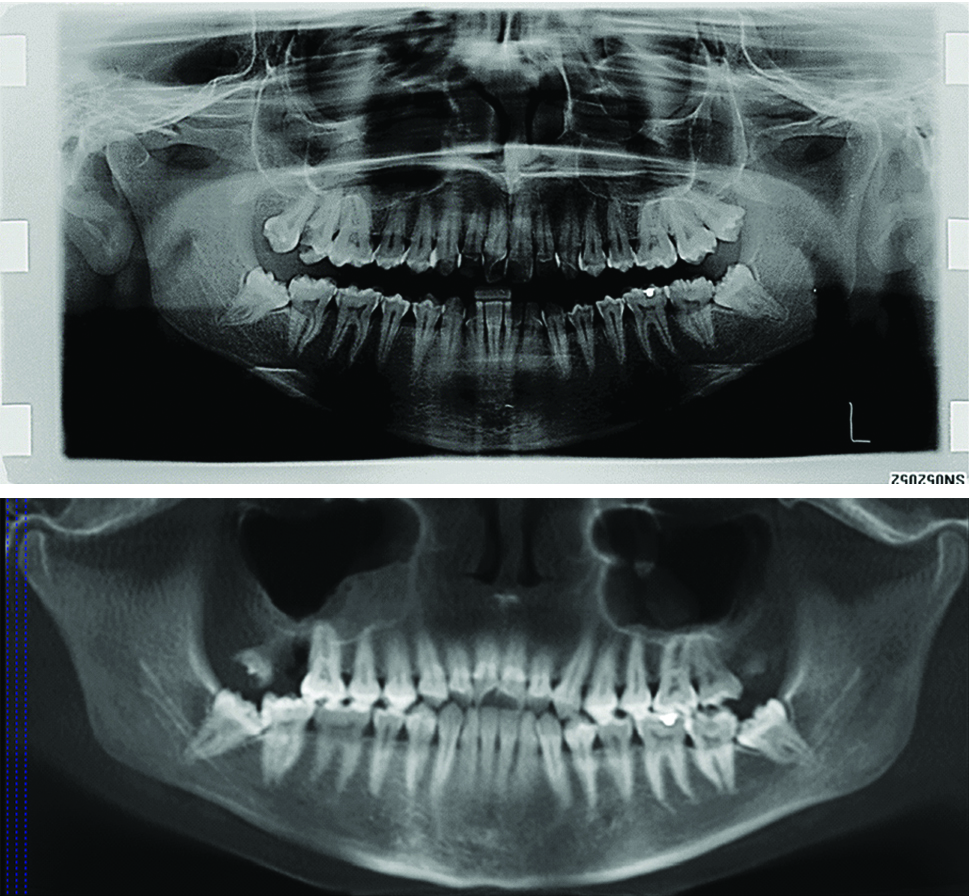
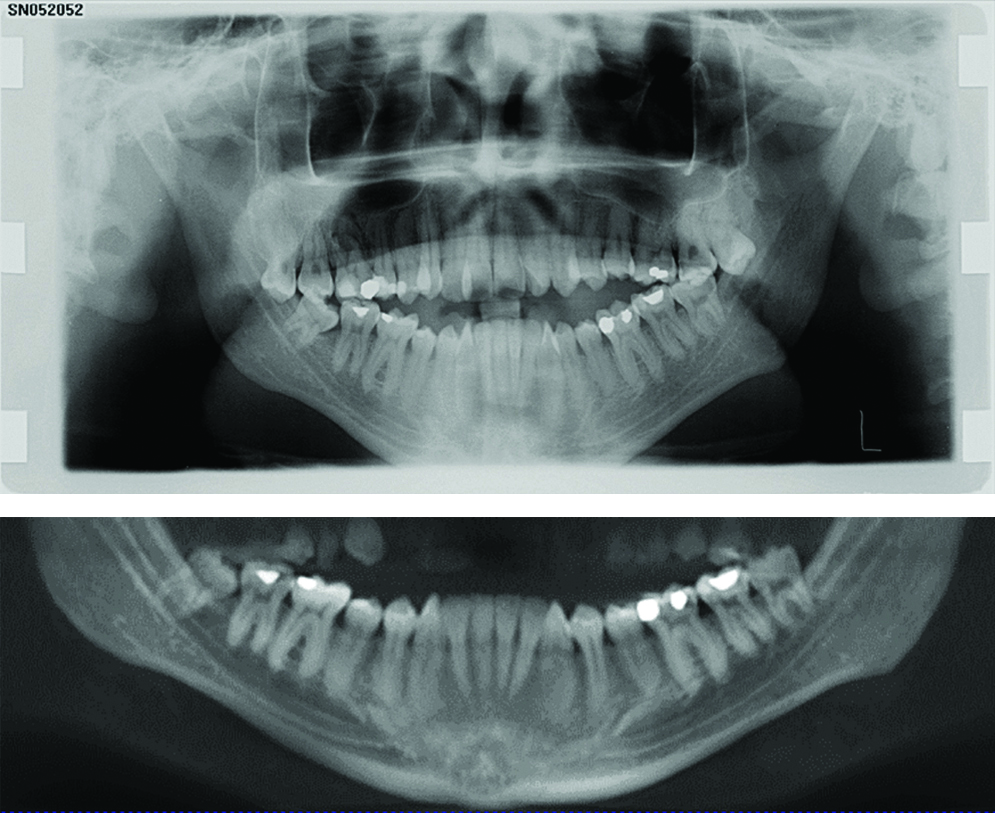
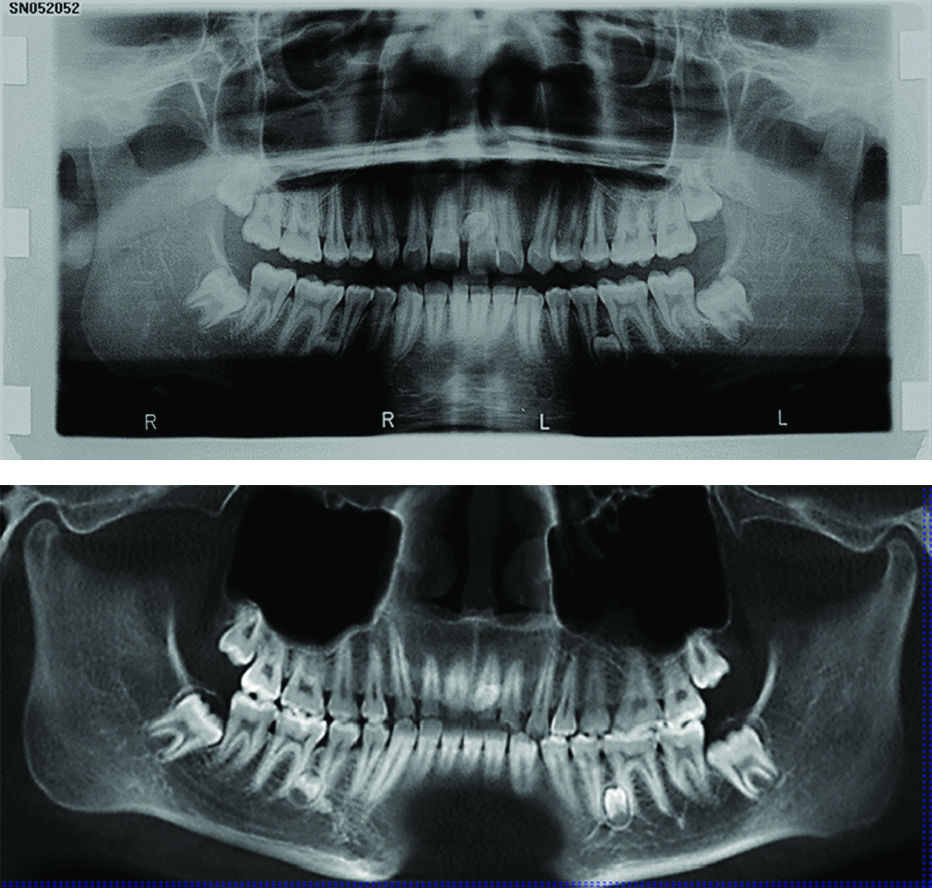
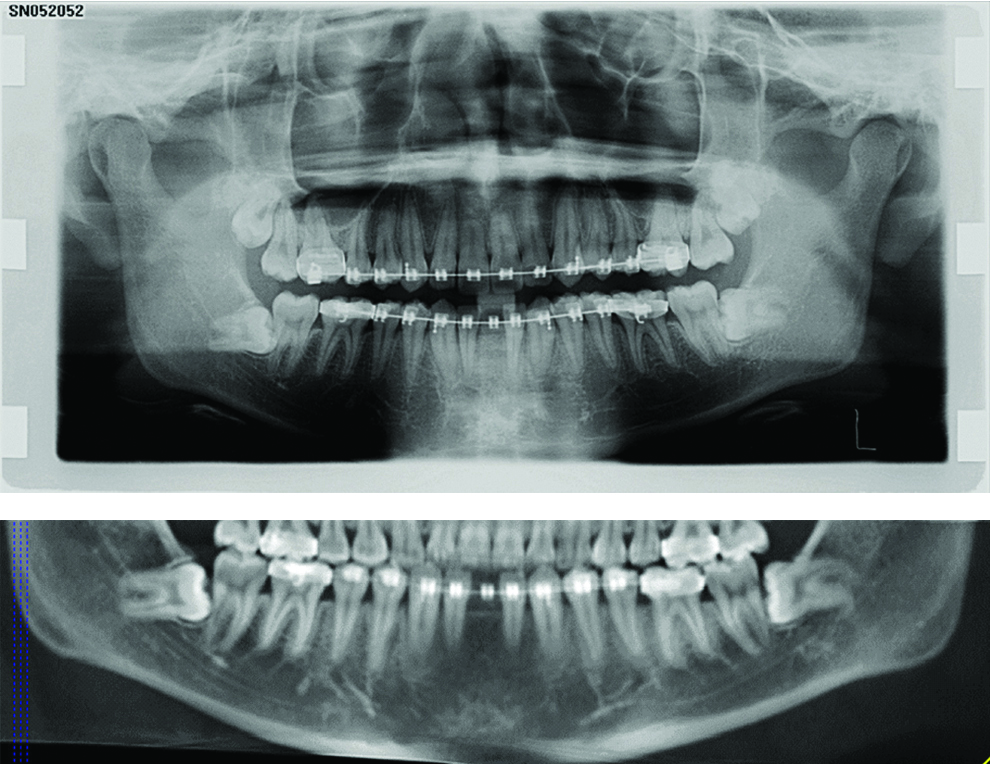
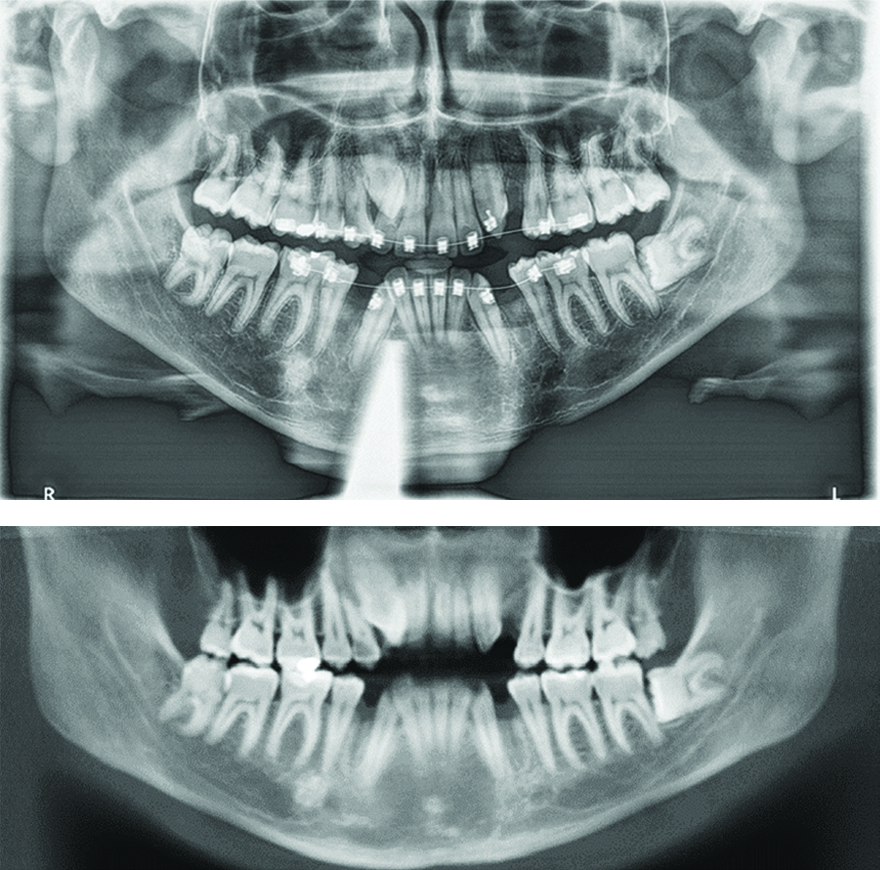
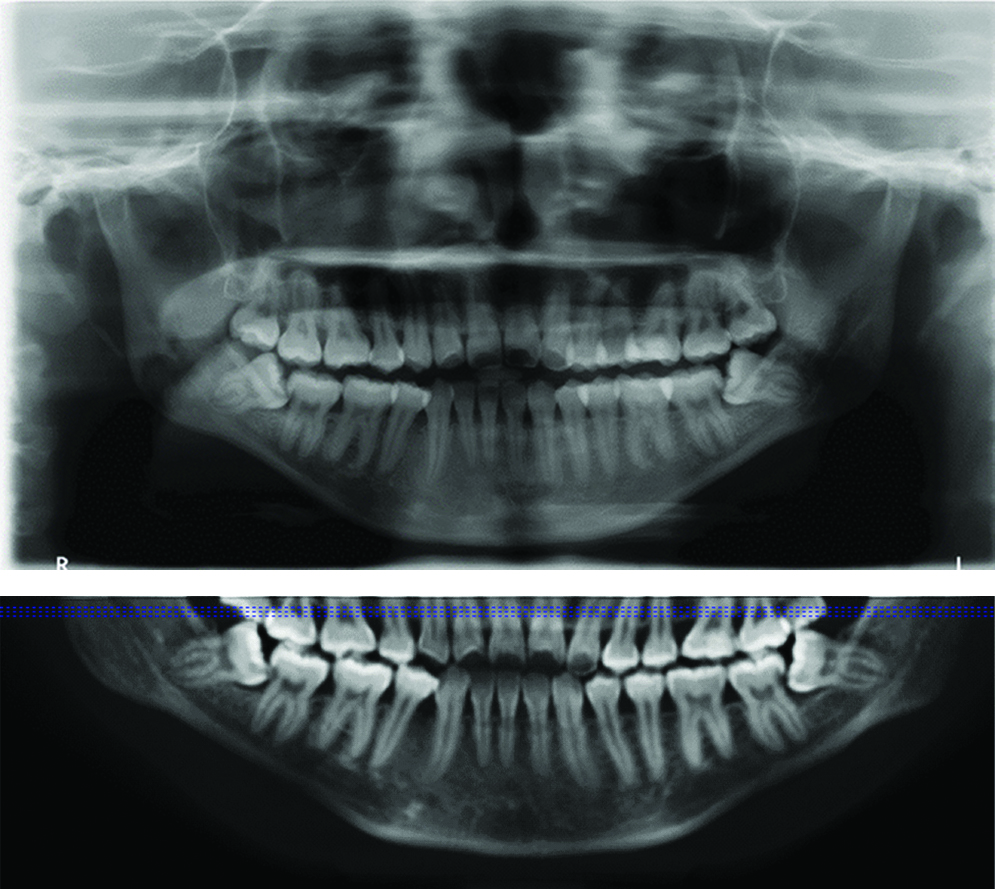
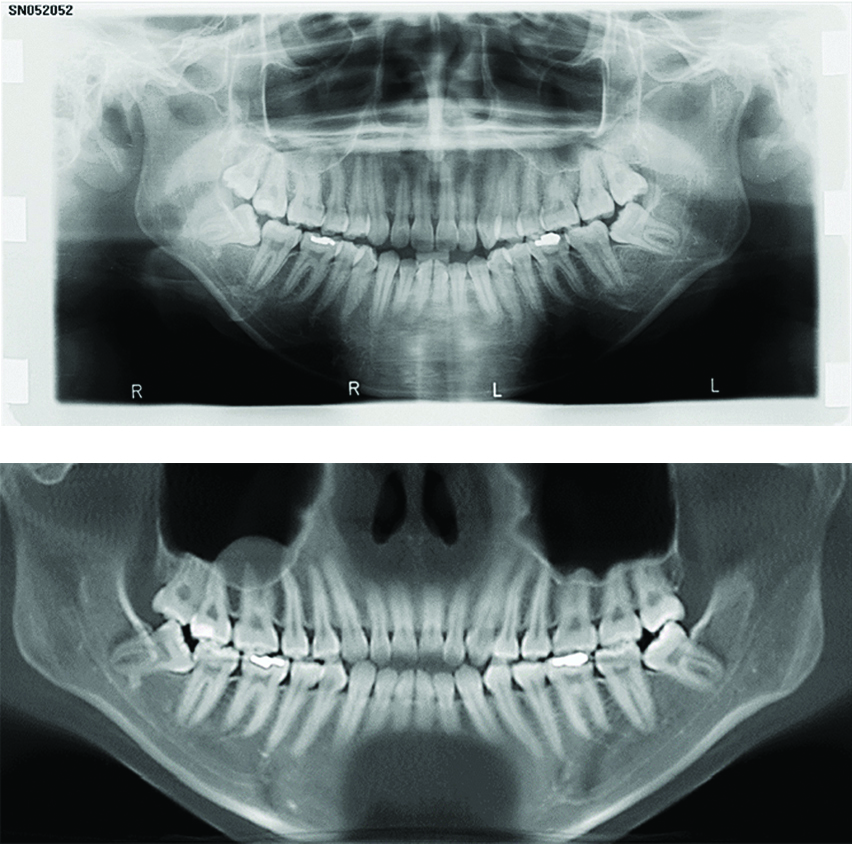
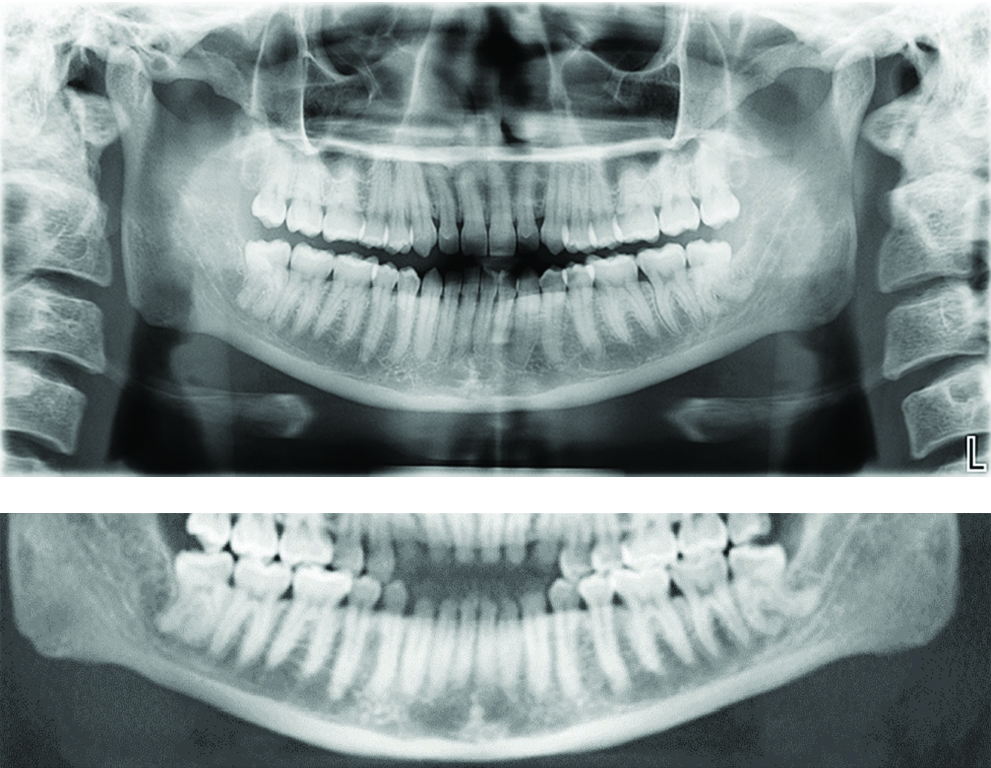
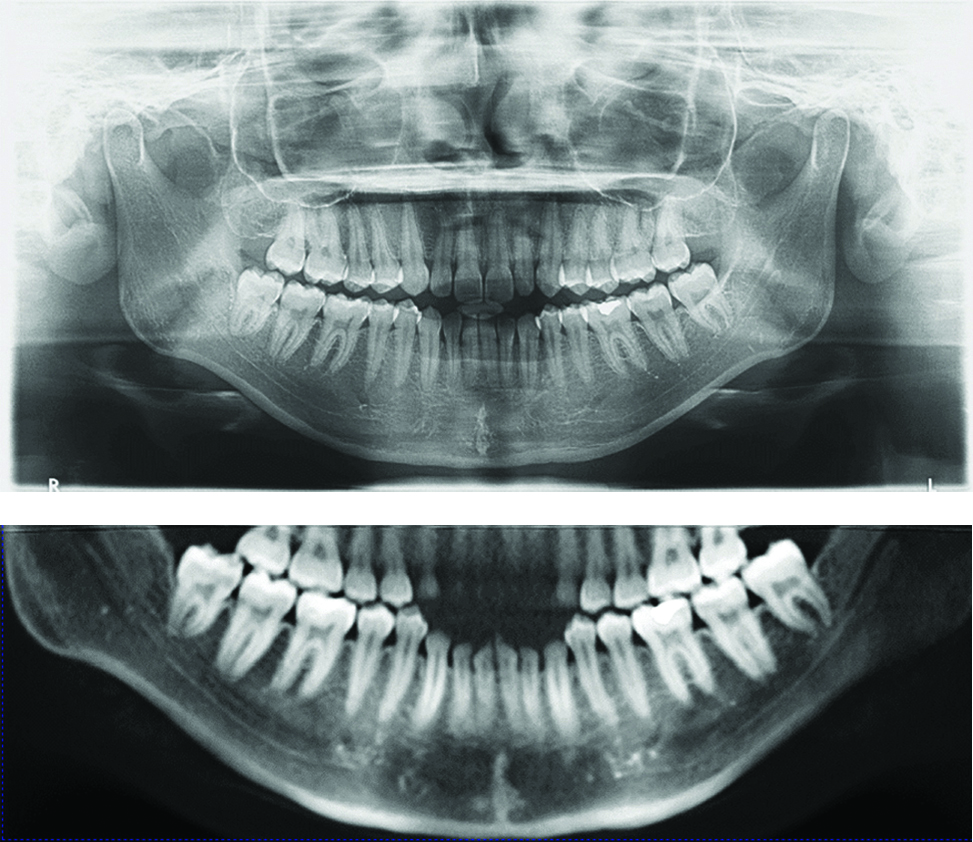
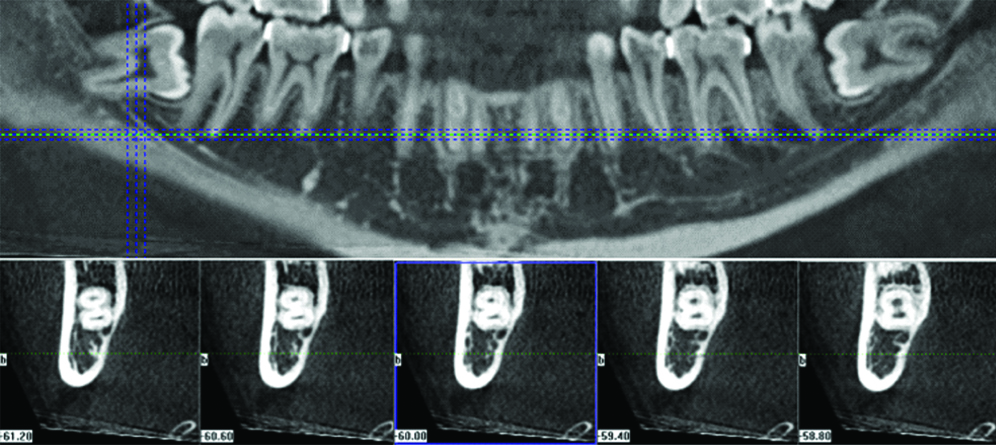
In this study, the type of IMTM impaction was categorised using Winters’ classification; giving five types of IMTM impaction (horizontal, vertical, mesioangular, distoangular and buccolingual impaction). Meanwhile, the type of panoramic radiological markers was categorised by expanding the seven panoramic radiological markers originally by Rood JP et al., to 15 markers [5]. The 15 markers were; deviation of the MC [Table/Fig-1], narrowing of the MC [Table/Fig-2], interruption of superior white line posterior to the third molar [Table/Fig-3], interruption of superior white line anterior to the third molar [Table/Fig-4], interruption of superior white line below the root/s [Table/Fig-5], interruption of superior white line between the mesial and distal roots of the third molar [Table/Fig-6], interruption of inferior white line [Table/Fig-7], darkening of one root [Table/Fig-8], darkening of two roots [Table/Fig-9], deflection of one root [Table/Fig-10], deflection of two roots [Table/Fig-11], dark and bifid one root [Table/Fig-12], and, dark and bifid two roots [Table/Fig-13], narrowing of one root [Table/Fig-14], narrowing of two roots [Table/Fig-15]. Using the modified classification of panoramic markers, the observer recorded the type of radiological markers presented on each panoramic radiograph. Following that, validation of the proximity of the IMTM to the MC of the same subject was carried out using the CBCT image. This was performed one month after the panoramic radiograph’s evaluation. Two type of signs were recorded from CBCT images for the evaluation of the proximity of the IMTM to the MC; presence and abscence of MC exposure signs. Presence of MC exposure sign was characterised by a disruption in the radiopaque cortex of MC by the impacted molar [Table/Fig-16]. A panoramic marker would suggest an increased risk of MC exposure by IMTM when the respective CBCT image demonstrated the presence of MC exposure sign. On the other hand, abscence of MC exposure sign was characterised by no disruption in the radiopaque cortex of MC by the impacted molar. Hence, this sign would suggest reduced risk of MC exposure by IMTM.
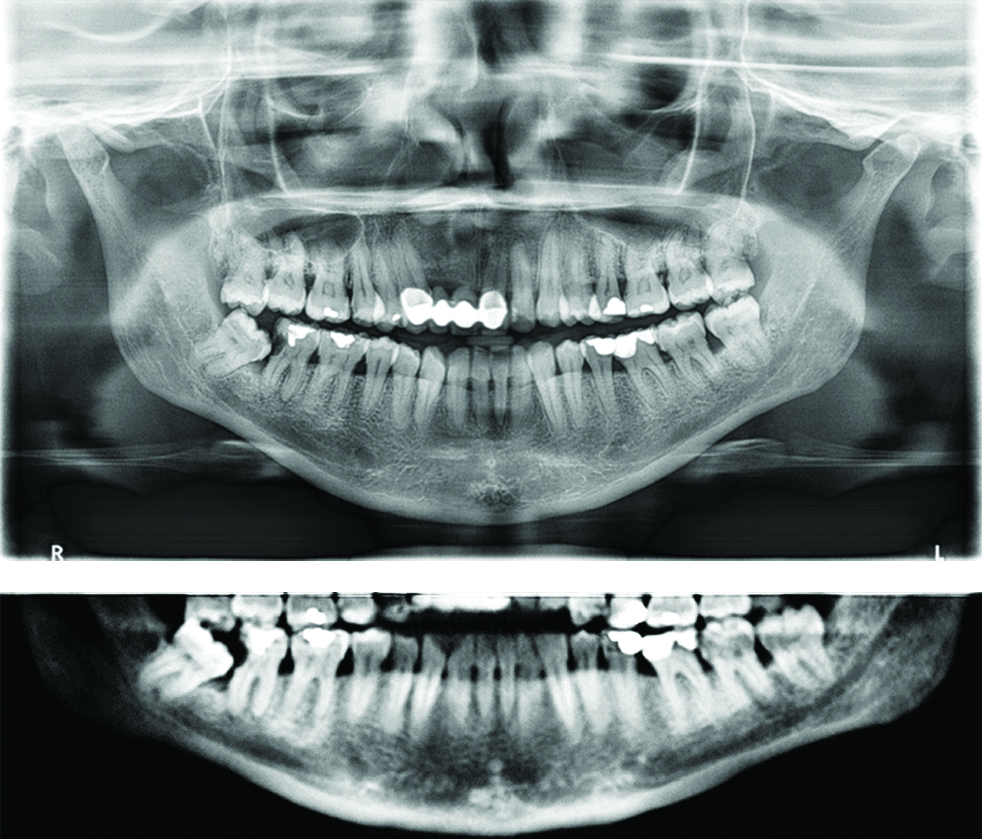
The following panoramic radiograph demonstrates the presentation of deviation of the MC adjacent to the right IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of narrowing of the MC adjacent to the left IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
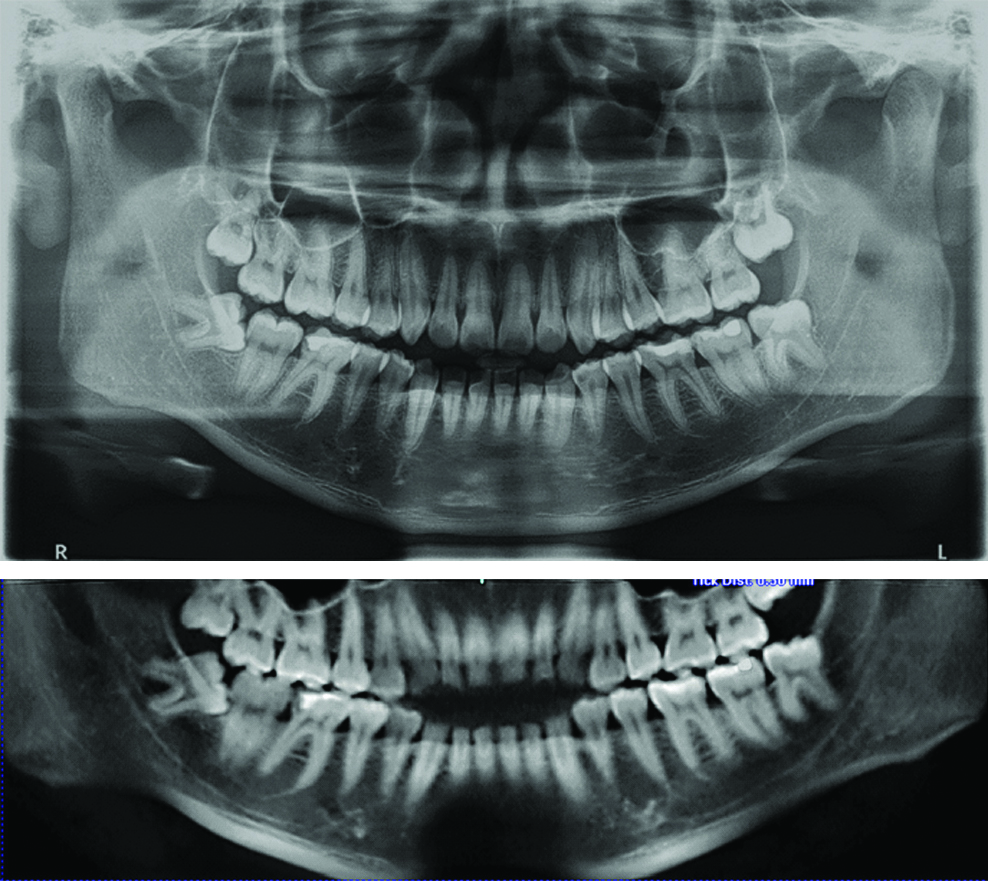
The following panoramic radiograph demonstrates the presentation of interruption of superior white line posterior to the right IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of interruption of superior white line anterior to the right IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of interruption of superior white line below the root of the left IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of interruption of superior white line between the mesial and distal roots of the right IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of interruption of inferior white line adjacent to the right IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of darkening of one root of the left IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of darkening of two roots of the left IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of deflection of one root of the left IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of deflection of two roots of the left IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of dark and bifid one root of the left IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of dark and bifid two roots of the right IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
The following panoramic radiograph demonstrates the presentation of narrowing of one root of the right IMTM. Below the panoramic radiograph is a 10 mm panoramic reconstruction slice of CBCT image showing the same panoramic marker of its respective panoramic radiograph.
This diagram is used to illustrate narrowing of two roots of the IMTM. However, none of panoramic radiograph samples in this study demonstrate the presentation of this marker.

The following 0.3 mm panoramic reconstruction slice of CBCT image at middle half level of the right IMTM demonstrate disruption of radiopaque line of the MC by the mesial root of the impacted molar. Cross-sectional slices of the molar from CEJ towards its furcation level demonstrate well-defined cortical lining of MC at the CEJ level. However, in the two cross-sectional slices at the furcation level of the IMTM, disruption of the cortical lining the roof of MC becomes evident. This finding confirms the presence of MC exposure sign observed in the panoramic slice of this CBCT image.
Statistical Analysis
All data were analysed using the SPSS software Version 23 (IBM Corp., New York, USA). The demographics characteristics, type of IMTM impaction and distribution of the panoramic radiological marker were shown as frequencies and percentages. The Chi-square test was used to evaluate the association of the type and number of panoramic radiological markers with the risk of MC exposure from CBCT. Result was statistically significant when p-value <0.05. Evaluation of the inter-observer agreement was performed by measuring the Kappa (k) values. A k value <0.40 was considered as poor agreement, 0.40 to 0.60 as moderate agreement, and good agreement when the value was between 0.61 to 1.00.
Results
The study sample comprised paired panoramic radiographs and CBCT images of 188 IMTMs from 103 patients (70 females and 33 males) with mean age and Standard Deviation (SD) of 27.3±4.98 years. A total of 142 (75.5%) of the impacted molars were documented in Malay patients, 19.1% in Chinese and 5.3% in Indians and other races as shown in [Table/Fig-17].
Demographic characteristics and type of impaction in the total sample of 188 IMTMs.
| Demographic information | Total No of IMTM {n (%)} N=188 |
|---|
| Age |
| Mean±Standard Deviation | 27.3±4.98 |
| Minimum | 18 |
| Maximum | 47 |
| Race |
| Malay | 142 (75.5) |
| Chinese | 36 (19.1) |
| Indian | 2 (1.1) |
| Others | 8 (4.2) |
| Gender: |
| Male | 63 (33.5) |
| Female | 125 (66.5) |
| Type of IMTM’s impaction: |
| Horizontal | 56 (29.8) |
| Vertical | 79 (42.0) |
| Mesioangular | 48 (25.5) |
| Distoangular | 4 (2.1) |
| Buccolingual | 1 (0.5) |
Using the Winters’ classification, the most common type of IMTM impaction was vertical impaction which contributed to 42% of the total sample. Other types of impaction were horizontal (29.8%), mesioangular (25.5%), distoangular (2.1%) and buccolingual (0.5%) impactions.
The inter-observers agreement in the panoramic image assessment of IMTM was substantial (k-value: 0.68) with 90.41% total agreement. In case of CBCT image assessment, excellent inter-observers’ agreement (k-value: 0.90) with total agreement of 96.7% was documented.
There were 456 panoramic markers obtained. The most common marker was the interruption of white line underneath the roots, n=106 (23.2%). The next most common marker was the interruption of white line anterior to the third molar, n=64 (14%), and interruption of the white line in between mesial and distal root, n=58 (12.7%).
[Table/Fig-18] summarised the distribution of the panoramic radiological findings and the odds of MC exposure with each marker. Three types of panoramic radiological markers were statistically significant in relation to the high risk of MC exposure (p<0.05). These markers were deviation of the canal, interruption of the white line posterior to the third molar and interruption of the white line anterior to the third molar. The odds for MC exposure was 8.45 times greater in the presence of deviation of canal in comparison to the absence of this marker. Meanwhile, the odds of MC exposure in the presence of interruption of the white line posterior to the third molar and interruption of the white line anterior to the third molar was 2.74 and 2.65, respectively. Other panoramic markers also demonstrated high likelihood of MC exposure; however, the result was not statistically significant. Absence of a marker was significantly associated with a low odds of MC exposure (odd ratio=0.28, p<0.05).
The association of panoramic markers and odds of MC exposure.
| Panoramic markers | Total, N=456 {n(%)} | Odds ratio | p-value |
|---|
| Deviation of MC | 19 (4.2) | 8.45 | 0.02* |
| Narrowing of MC | 27 (5.9) | 0.98 | 0.96 |
| Interruption of white line posterior to molar | 45 (9.7) | 2.74 | 0.02* |
| Interruption of white line anterior to molar | 64 (14.0) | 2.65 | 0.01* |
| Interruption in between mesial and distal roots | 58 (12.7) | 1.27 | 0.50 |
| Interruption of white line underneath the root | 106 (23.2) | 1.68 | 0.11 |
| Interruption of inferior white line | 8 (1.75) | N/A** | 0.11 |
| Darkening of one root | 40 (8.8) | 1.31 | 0.51 |
| Darkening of two roots | 14 (3.1) | 2.63 | 0.54 |
| Narrowing of one root | 4 (0.9) | 0.41 | 0.58 |
| Narrowing of two roots | - | - | - |
| Deflection of one root | 15 (3.3) | 6.35 | 0.07 |
| Deflection of two roots | 6 (1.3) | 2.11 | 0.67 |
| Dark and bifid of one root | 4 (0.9) | 0.41 | 0.58 |
| Dark and bifid of two roots | 1 (0.2) | - | 1.00 |
| Absence of panoramic marker | 45 (9.9) | 0.28 | 0.00 |
**Odds ratio cannot be computed because there is 0 in 1 cell
*Statistically significant high risk markers (odds ratio >1, p<0.05) Pearson Chi-square test was used for type of marker with n(%) > 18 (4), Fisher-exact test was used for type of marker with n(%) ≤ 18 (4)
The number of markers observed on one panoramic radiograph ranged from 0 to 6, with a median of 2 (IQR 3) as shown in [Table/Fig-19]. We assessed the effect of number of markers in the next analysis [Table/Fig-20]; where the number of panoramic markers were divided into two groups which are more than 2 markers (>2 markers) and 2 or less markers (≤2 markers). Comparable number of MC exposure in (≤2 markers) and (>2 markers) group, 68 and 65 respectively with two times higher number of unexposed MC in (≤2 markers) than (>2 markers) group correlate with our next finding. We showed that panoramic radiographs with more than two markers had 2.14 times likelihood of having MC exposure than those with only two or less marker.
Distribution of total number of panoramic markers.
| Characteristics of markers | Total No of IMTM {n (%)} N=188 |
|---|
| Total number of markers |
| Median (IQR) | 2 (3) |
| Minimum | 0 |
| Maximum | 6 |
| Number of markers on an image |
| 0 | 46 (24.5) |
| 1 | 27 (14.4) |
| 2 | 33 (17.6) |
| 3 | 31 (16.5) |
| 4 | 34 (18.2) |
| 5 | 14 (7.4) |
| 6 | 3 (1.6) |
Association between numbers of markers with MC exposure. Data was analysed using Pearson Chi-Square test.
| Number of panoramic markers | MC exposure in CBCT finding {n (%)} | Odds ratio | p-value |
|---|
| Presence | Absence | Total |
|---|
| ≤2 | 68 (51.1) | 38 (69.1) | 106 (56.4) | Reference | Reference |
| >2 | 65 (48.9) | 17 (30.9) | 82 (43.6) | 2.14 | 0.04 |
| Total | 133 (100%) | 55 (100%) | 188 (100%) | | |
Discussion
According to the original classification of panoramic markers by Rood JP et al., that was published nearly three decades ago, there were seven types of markers associated with high risk of MC exposure by IMTM [5]. One of these markers, include the interruption of white line. Today, with more interactive media in digital radiography, it is possible to expand the original markers of seven to fifteen markers considering the significant quality of life impact to the iatrogenic injury of IAN. In this study, we aimed to record panoramic radiograph signs based on the 15 types of markers and investigate their relationship with the risk of MC exposure by IMTM. Detail evaluation of the panoramic radiograph signs in the pre-operative assessment of IMTM, could give better insight about the risk of MC exposure following surgical removal of the impacted molar.
Three panoramic radiological markers that indicate close relationship between the IAN and the IMTM have been described in the literature [6,7]. These markers are: darkening of the root, interruption of the white line, and deviation of the MC. A systematic review by Atieh MA showed low sensitivity and high specificity for the three markers, suggesting that presence of one of these markers on panoramic radiograph not necessarily indicate an intimate relationship between IMTM roots and MC [10]. Atieh MA further advocated surgeons to use other detailed imaging technique in determining MC exposure by IMTM [10]. This concept was supported by Matzen LH et al., and the use of a CBCT is recommended [11]. In this study, each of the panoramic markers was further evaluated with CBCT finding.
Based on the 15 types of panoramic markers, we found three markers were statistically significantly associated with high risk of MC exposure with the odds of 2-8. Between the three markers, we showed that deviation of the MC has the highest odds of MC exposure. MC deviation was shown as the only significant marker in other studies [3,12]. Interruption of the white line was often described as significant high-risk marker [3,6,7] with the odds ratio ranged from 2.95 to 5.4. However, the specific region of the white line which demonstrates the disruption sign was never been mentioned in the previous studies [3,6,7]. The mandibular canal is observed on the panoramic radiograph as two white lines, the superior and inferior lines. Interruption of the superior white line may occur posterior to the third molar, anterior to the third molar, underneath the root, and in between the mesial and distal roots. We found strong association with high risk of MC exposure when there was an interruption of the white line anterior to the IMTM (OR=2.74, p<0.05) and interruption of the white line posterior to the IMTM (OR=2.65, p<0.05). On the other hand, interruption of the line in between the mesial and distal roots and underneath the root did not illustrate any significant association.
Darkening of the roots was shown by many researchers to be the single most important warning sign of IAN exposure or injury [4,6,7]; however, other researchers failed to confirm this finding [3,12]. This included our study. Although the odds of having the MC exposure was 2.63 for darkening of two roots, the association was not statistically significant.
Presence of more than two markers was significantly associated with the MC exposure, with 2.14 likelihood of exposure in comparison with one or two markers. This was in line with the results of previous studies [13,14].
In relation to the absence of markers, our study is in agreement with a study by Sedaghatfar M et al, where the likelihood for MC exposure was shown to be low [6]. Atieh MA concluded that panoramic radiography is a more reliable tool in excluding the close relationship between the IMTM and the IAN in the absence of these radiographic markers [10].
From the clinical perspective, in a case where an increased-risk of MC exposure is anticipated, high risk consent is recommended and procedures such as coronectomy or other technique such as the one described by Landi L et al., could be considered after a thorough discussion with the patient [15].
CBCT is emerging as the diagnostic imaging of choice prior to surgery due to its ability to demonstrate the three-dimensional information such as the bucco-lingual assessment of the IMTM. Lingual position of the MC in relation to IMTM has been reported and this position increases the risk of IAN injury following surgical removal of IMTM [7]. Whenever surgical extraction of IMTM need to be considered in a presence of significantly associated high risk panoramic marker, further assessment with CBCT is highly recommended. The reliable three-dimensional information from CBCT image which allows bucco-lingual assessment of the IMTM and MC may influence the treatment decision and patient inform consent. Moreover, knowing the bucco-lingual relationship of IMTM to the MC will also be useful in preventing excessive pressure to MC or the careless use of burs and elevators when surgical removal of the impacted molar is performed.
In this study, the type of panoramic markers was recorded in more precise manner by considering the specific regions of the interruption of white line. These new criteria are clinically important as it add information in understanding the risk of MC exposure in the presence of interruption of white line. As demonstrated in this study, the interruption of white line was significantly associated with high risk of MC exposure when it was located anterior or posterior to the IMTM.
Limitation
Unlike previous studies, we did not confirm the exposure of the MC with clinical findings, i.e., surgery. The results were based on radiographical analysis alone.
Another limitation was related to the depth of the study in relation to absence of the panoramic markers. The conclusion we made was low likelihood of having an MC exposure. In the future, when there is absence of a panoramic marker, the actual distance between the IMTM and the MC could be measured, and this could be highlighted as the safe distance between the IMTM and the MC.
Conclusion
Interruption of the superior white line is strongly correlated with high risk of MC exposure when the diminishing sign of the white line specifically located anterior or posterior to the IMTM.
Other panoramic feature associated with increased odds of MC exposure was deviation of the MC. Presence of more than two markers also indicated increased likelihood to have MC exposure.
**Odds ratio cannot be computed because there is 0 in 1 cell
*Statistically significant high risk markers (odds ratio >1, p<0.05) Pearson Chi-square test was used for type of marker with n(%) > 18 (4), Fisher-exact test was used for type of marker with n(%) ≤ 18 (4)