A seizure is a paroxysmal alteration in neurological function. This can be behavioural, motor or autonomic. Neonatal seizures are more frequent in neonatal period with a reported incidence of 0.95 to 3.5/1000 live births [1]. Neonatal seizures are dissimilar from adults due to lack of myelination and arborisation of axons and dendritic processes resulting in impaired propagation of electric impulses [2,3]. Predominant types of neonatal seizures include subtle, clonic, tonic and myoclonic seizures. Most common aetiological factors for neonatal seizures comprise of neonatal encephalopathy (60%), intracranial infection (5-10%), intracranial haemorrhage, cerebral malformations and correctable metabolic disturbances like hypoglycaemia and electrolytes derangements (sodium, calcium and magnesium) [4].
In the newborn, there is an unusual problem of electro-clinical dissociation. Seizures occur when a large group of neurons undergo excessive, synchronised depolarization, which can result from excessive excitatory amino acid release or deficient inhibitory neurotransmitter. Another potential cause is disruption of ATP-dependent resting membrane potentials, which causes a flow of sodium into the neuron and potassium out of the neuron. Hypoxic Ischemic Encephalopathy (HIE) disrupts the ATP-dependent sodium-potassium pump and appears to cause excessive depolarization. It is an important cause of neonatal seizures [1]. Alterations in ion gradients across cellular membranes can have direct and indirect effects on neuronal discharge and may facilitate epileptiform activities [5]. Principally the electrolyte haemostasis is a function of ionic gradient across the neuronal cells, blood brain barrier, and glia [5]. As early diagnosis and management improves outcomes it is vital to have high index of suspicion, prompt investigation and intervention.
Hyponatremia is defined as serum sodium concentration <133 mmol/L which is reported in 70% of convulsions in infants without other detectable aetiology [6]. It is often life threatening leading to cerebral oedema and herniation. Also, the severity of neurological manifestations is proportional to the degree of hyponatremia. Hyponatremia can be an accompaniment of perinatal asphyxia due to volume overload (occurring from renal impairment) and inappropriate secretion of antidiuretic hormone [7]. Cerebral oedema worsens further due to loss of adaptive mechanism of brain in presence of hypoxia and ischemia. Similarly, hypernatremia (serum sodium levels >146 mmol/L) is equally injurious leading to neuronal manifestations and rate of increase of serum sodium is an important determinant of CNS manifestations [8]. The severity of clinical manifestations will be proportionate to the degree of hypernatremia which is severe with serum sodium levels >158-160 mmol/L.
Research question for this study was to find out how many percentages of neonates with convulsion (irrespective of cause) presents with alteration of serum sodium levels? Hence, this study was carried out to estimate the serum sodium levels in neonates presenting with seizures and to correlate the serum levels with clinical manifestations and to delineate its aetiological factors.
Materials and Methods
This prospective cross-sectional study was carried in a tertiary level NICU of Dr BC Roy Postgraduate Institute of Paediatric Sciences, Kolkata, West Bengal, India from November 2014 to October 2015. Ethical approval was taken from institute’s ethics committee (Registration No: (BCH/ME/PR/2658C). All the consecutive extramural neonates with seizures who met the inclusion criteria were enrolled. A detailed history was obtained in all neonates with special emphasis on the onset, duration, frequency, type of seizures and level of consciousness during and in between seizures alongside antenatal, natal and postnatal details of risk factors. Also, history pertaining to the clinical manifestations like lethargy, poor feeding, jaundice, excessive cry, fever and vomiting were noted. The neonatal seizures were classified according to Volpe’s classification into subtle, clonic, tonic and myoclonic seizures [4]. Detailed clinical examination comprising vitals, general physical examination and systemic examination with regard to central nervous system was performed. Relevant investigations (CBC, sepsis screening, RBS, serum electrolytes) were done as per clinical requirement and unit protocol Serum electrolytes were done by Ion Selective Electrode method (ISE). Serum sodium levels of 133-146 mmol/L were considered normal. Hyponatremia was considered when serum sodium of <133 mmol/L and severe hyponatremia <120 mmol/L. Hypernatremia is defined as serum sodium levels >146 mmol/L. Serum ionized calcium levels 1.07-1.23 mmol/L were considered normal [9]. Random blood sugar was done with glucostick bedside and subsequently confirmed by glucose oxidase method. Hypoglycaemia was diagnosed if RBS is <40 mg/dL. Serum potassium levels of 3.2-6 mmol/L were considered normal [9]. Cranial ultrasound examination was done in all neonates with seizures to rule out ICH, hydrocephalus, congenital cerebral anomalies and infarction. Additional investigations were done as per clinical requirement (CSF analysis, CT brain, MRI Brain, EEG, IEM work up with Tandem mass spectrometry). All the neonates were treated according to the standard unit protocols.
Inclusion Criteria
Neonates presenting with seizures at admission or developing seizures during the hospital stay before 28 days of life and in whom parental consent was obtained were included.
Exclusion Criteria
Neonates with jitteriness, tetanic spasms, isolated subtle phenomenon, apnea or paroxysmal autonomic changes i.e., only subtle motor movements or apnea without tachycardia were excluded from the study. Also, neonates in whom parental consent could not be taken were excluded.
Definition
Neonatal seizures: as with any other type of seizure, are paroxysmal, repetitive and stereotyped events. They are clinically subtle, inconspicuous and difficult to recognize from the normal behaviours of the inter-ictal periods or physiological phenomena [4]. Perinatal Asphyxia: National neonatology forum of India has suggested that birth asphyxia should be diagnosed when “baby has gasping and inadequate breathing or no breathing at 1- minute” [10].
Sample Size Calculation
The total sample size was estimated using formula n=z2pq/d2. With 95% Confidence level and 80% power, p=prevalence of hyponatremia among neonatal seizures (70%), q=100-p=30%, d=Relative precision taken as 15% of p=15×70/100=10.5. n(1.96)2×70×30/(10.5)2 =73.17≈76 neonates with the seizure met the study criteria during study period so all of them were included.
Statistical Analysis
The data was analysed using SPSS version 20. Chi-square test was applied to find the association between categorical variables. The level of significance for this study taken was 0.05.
Results
Mean age of mothers at time of delivery was 22.41±3.76 years (minimum of 16 years to maximum of 35 years). 93.4% of mothers have received regular antenatal checkup and 100% have received tetanus toxoid immunization. 3.9% of mothers have suffered from febrile illness during pregnancy, 2.6% had suffered PIH and 2(2.6%) mothers had oligohydramnios.
None of the mothers had history of diabetes or intake of drugs and prenatal steroids. 16 (21.05%) babies were born to mothers with Prolonged Rupture of Membrane (PROM). There was no history of birth injury. History of fever was present in 10 neonates, 54 had history of refusal of feeds, five had history of excessive crying, four neonates had vomiting and history of jaundice was present in five neonates. History of perinatal asphyxia was present in 62 neonates.
Early onset (up to 7 days of life) of seizures was seen in 72 neonates (94.7%), out of which seizures in first four days of life was present in 69 (90.8%). Late onset seizures (after 8 days of life) were present in only 4 (5.3%) cases [Table/Fig-1]. Majority of neonates 28 (36.8%) had suffered one episode, 20 (26.3%) from two episodes, 9 (11.8%) suffered three episodes, 12 (15.8%) suffered four episodes while multiple episodes were present in 7 (9.2%) neonates. Maximum duration was 2-3 minutes, present in 35 (46.1%) neonates. There were 10 (13.2%) preterm and 2 (0.9%) post-term babies. Majority of neonates 61 (80.3%) were Appropriate for Gestational Age (AGA) and 15 (19.7%) Small for Gestational Age (SGA). Males (48/76) were 1.7 times that of females (28/76). Mean gestational age of neonates was 37.86±2.71 weeks ranged from 24 to 43 weeks.
Serum sodium levels according to day of onset of neonatal seizure.
| Day of onset of seizures | Serum sodium <133 mmol/L | Serum sodium 133-146 mmol/L | p-value |
|---|
| 1-7 days | 44 (97.8%) | 28 (90.3%) | 0.364 (>0.05) |
| 8-28 days | 1 (2.2%) | 3 (9.7%) |
Of the total 76 neonates presented with seizures, hyponatremia{<133 mmol/L was present in 45 neonates (59.2%)} and out of those 45, 8 (17.7%) had severe hyponatremia (<120 mmol/L). Normal serum sodium levels (133-146 mmol/L) were present in 40.8% (n-31) and none of the study neonates had hypernatremia. Hyponatremia was significantly more common among preterm neonates (90%) as compared to term babies (p=0.020) [Table/Fig-2]. HIE was the commonest cause of neonatal seizures in the current study being present in 81.6% (n-62). All the neonates with severe hyponatremia had HIE and majority (97.3%) with mild hyponatremia had HIE [Table/Fig-3]. Neonatal sepsis was present in 13 neonates (17.1%) (EOS&LOS). Isolated hyponatremia was not seen and it was always secondary to HIE or HIE along with other comorbidities like sepsis and meconium aspiration syndrome (MAS) (n-7). Meningitis was cause of seizures in three (3.9%) cases. Isolated metabolic abnormalities were present in 11 neonates (14.5%), which included hypoglycaemia (13.2%) followed by hypocalcaemia (6.5%).
Serum sodium levels according to gestational age.
| Gestational age (weeks) | Serum sodium levels (mmol/L) | p-value |
|---|
| <120 | 120-133 | 133-146 |
|---|
| Term (37-42) | 4 (6.2%) | 30 (46.9%) | 30 (46.9%) | 0.02 (<0.05) |
| Preterm (<37) | 3 (30.0%) | 6 (60%) | 1 (10%) |
| Post term (>42) | 1 (50%) | 1 (50%) | 0 |
Serum sodium levels according to presence of HIE.
All the neonates with severe hyponatremia had HIE and majority with mild hyponatremia had HIE
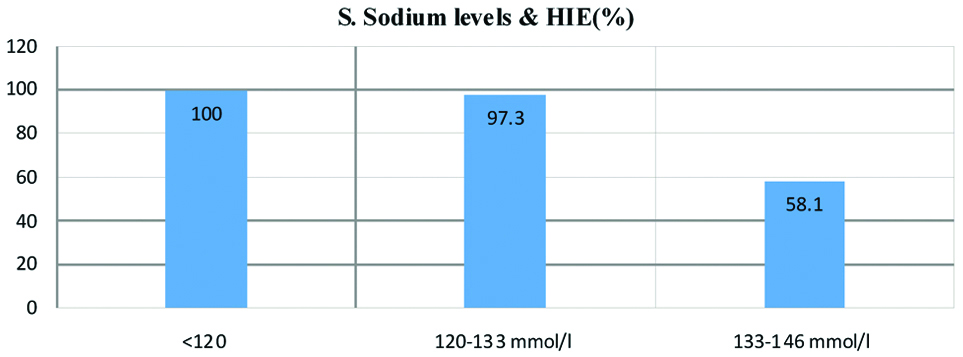
Incidence of hyponatremia was significantly high in neonates with HIE (70.9%, 44/62, p<0.001). Among 76 neonates, mean serum sodium levels seen were 130.94 mmol/L (7.88). Drowsiness was significantly more frequent in hyponatremic neonates (80%, 36/45, p<0.001) [Table/Fig-4]. Comparatively, greater percentage 85.5% (n=65) of neonates had developed seizures in first three days and 63% (n-41) of them were hyponatremic: 35 (53.8%) had serum sodium levels 120-133 (mmol/l) and 6 (9.2%) had severe hyponatremia. While among late onset seizures, 25% cases were hyponatremic [Table/Fig-1]. But these differences were not significant (p=0.364). Similarly, greater percentage of neonates who had subtle seizures were hyponatremic i.e.,64.3% followed by 54.3% in focal seizures. Again these differences in serum sodium levels according to type of neonatal seizures were not found to be significant (p=0.875). Majority of neonates 65 (85.5%) had been discharged and outcome was fatal in 11(14.5%). A 50% (4/8) of severely hyponatremic neonates had expired. A 16.2% (6/37) of those having serum sodium levels 120-133 mmol/L had expired and comparatively 96.8% (30/31) of normonatremic neonates were discharged after treatment. Poor outcome like death among neonatal seizures was found to be significantly associated with hyponatremia (p=0.003) Metabolic abnormalities were seen in 66 (86.8%) of neonates, out of which 11 had isolated metabolic derangement and 55 had metabolic abnormalities along with other associated comorbidities. Interestingly, hyponatremia and hypocalcaemia were common among multifactorial/mixed seizures while hypoglycaemia (10 cases) was most common among primary metabolic seizures. Mean potassium levels noted were 4.45 (1.03) and mean calcium levels noted were 1.235 (1.3). The most common biochemical abnormality detected was hypocalcaemia (n-49,64.5%), 22 (28.9%) had normal serum calcium levels whereas 5 (6.6%) cases had hypercalcaemia (serum calcium levels >1.23 mmol/L).
Serum sodium levels according to consciousness.
| Serum sodium levels (mmol/L) | Consciousness | p-value |
|---|
| Drowsy | Normal | Unconscious |
|---|
| <120 mmol/L (Severe Hyponatremia) | 4 (50%) | 2 (25%) | 2 (25%) | <0.001 (<0.05) |
| 120-133 mmol/L (Hyponatremia) | 32 (86.5%) | 4 (10.8%) | 1 (2.7%) |
| 133-146 mmol/L (Normal) | 18 (58.1%) | 13 (41.9%) | 0 (0%) |
Discussion
HIE has been reported to be the commonest cause of neonatal seizures in this study affecting 52.6% of neonates. There is increased depolarization of ATP dependent Na+- K+ pump in HIE. Seizures due to HIE may be seen in first 72 hours of life in both term and preterm infants. Loman AM et al., found HIE in 53.9% of neonatal seizures [11]. Similarly, Sood A et al., and Kumar A et al., reported that perinatal asphyxia was the cause for neonatal seizures in 45.7% and 48.3% cases respectively, which was comparable with the results of current study [12,13]. Sahana G et al., found that birth asphyxia was the commonest cause of neonatal seizures in 57.8% followed by transient metabolic factors, hypoglycaemia (9.2%) and hypocalcaemia (6.4%) and infections in 16 (14.7%) cases [14]. Whereas other studies, like Singh SD et al., found perinatal asphyxia as the most common cause of neonatal seizures in 33.3% cases only [15]. The biochemical effects of neonatal seizures include derangements of energy metabolism, disturbances of glucose, calcium, magnesium along with sodium abnormalities. Also, amino acid, organic acid, urea cycle disorders, use of certain drugs like local anaesthetics and pyridoxine dependency or deficiency, and hyperbilirubinemia, can be associated with convulsive phenomena in newborn infants. However, the aberrations of glucose and the divalent cations were the most frequent.
In present study, metabolic abnormality was seen in 66 cases, of which 11 were isolated metabolic seizures and 55 were associated with both metabolic and non-metabolic factors. 66 (86.84%) of neonates with seizures demonstrated one or more biochemical abnormalities including hyponatremia, hypoglycaemia, hypocalcaemia. Some of these biochemical disturbances may trigger seizures or potentiate further brain damage especially in asphyxiated infants. Therefore, in infants with perinatal asphyxia, close biochemical monitoring is vital for better long term prognosis.
In this study, hyponatremia was found in 59.2% of neonates. None of the cases had hypernatremia which was similar to findings by Kumar A et al., [13]. Neonates with perinatal asphyxia might have had hyponatremia due to fluid overload as a result of renal compromise or due to inappropriate secretion of antidiuretic hormone [1]. In the present study hyponatremia was present in 44 out of 62 neonates with HIE. 6 out of 10 cases with septicaemia were also hyponatremic which can be explained again on the basis of inappropriate secretion of antidiuretic hormone seen in this condition. None of cases with meningitis in present study were hyponatremic although they were hypoglycaemic. Primary metabolic disorders accounted to 14.5% of cases in this study, comparable to the report from Loman AM et al., in which metabolic disorders were seen in 10.9% of neonatal seizures [11]. Improvements in infant feeding practices have made this category an uncommon cause of seizures. Among pure metabolic seizure hypoglycaemia (90.9%) was most common and 4.8% of neonates with HIE had hypoglycaemia and this finding is in disagreement with others. Studies done by Reddy KV et al., hypoglycaemia was seen in 9.5% neonates [16], by Kumar A et al.,11.11% neonates [13] and Sahana G et al., 9.17% neonates [14], as cause of pure metabolic seizures.
Sahana G et al., found hypocalcaemia in 6.4% neonates [14]. Early onset hypocalcaemia occurs in premature babies and babies in whom asphyxia or trauma has occurred and infants of mothers with hypoparathyroidism. Kumar A et al., studied 35 neonates of which 22 (62.8%) had biochemical abnormalities [13]. Sood A et al., studied 59 neonates of which 29 (49.15%) had biochemical abnormalities i.e., hypocalcaemia was detected in 14 (48.3%), hypoglycaemia in 14 (48.3%) [12]. The study conducted by Sood A et al., and Kumar A et al., showed that biochemical abnormalities were seen in cases of HIE, intracranial bleeding, infections and metabolic disorder [12,13]. Moreover, Sood A et al., also demonstrated that hypocalcaemia and hypoglycaemia were most common metabolic abnormalities [12]. The above results were comparable with the findings of the present study.
It was found that higher percentage of neonates with subtle seizures were hyponatremic (64.3%) followed by focal seizures in present study (54.3%). Drowsiness was also found to be significantly more common in hyponatremic neonates (p<0.001). Hyponatremia was significantly more common among preterm neonates (90%) as compared to term babies in present study (p=0.020).
Final Outcome/Survival among Neonates with Seizures
In the neonatal intensive care unit, the incidence of neonatal seizures remains as high as 10- 25%, out of which about 15% die and 35-40% have major neurological sequelae [17,18]. In present study most of neonates 85.5% were discharged and fatal outcome was seen in 14.5%. Also, among the neonates who expired, 50% had severe hyponatremia. Poor survival among neonatal seizures was significantly related to hyponatremia (p=0.003) and thus fatality was most frequent in hyponatremic neonates. In present study among severely hyponatremic neonates all had HIE and there is only one case with hyponatremia not associated with HIE but with sepsis. HIE had been significantly associated with hyponatremia (p<0.001).
Limitation
The current study is a hospital based study; the findings cannot be generalised in broader population. It only depicts the clinical picture of neonatal seizure in this study setting. For association of hyponatremia with seizure further analytical study needs to be carried out in large sample population.
Conclusion
Hyponatremia is an important treatable causative and prognostic factor for neonatal seizures due to perinatal asphyxia. Hyponatremia should be screened and managed promptly in all cases of neonatal seizures for better outcome.