Prostate cancer is the second most common cancer in men with estimated 161,360 new cases and estimated 26,730 deaths in 2017. Approximately, 11.6% of men are diagnosed with prostate cancer at some point during their lifetime; 79.2% cases are diagnosed at the local stage and the five-year survival for localised prostate cancer is 100.0% [1]. Incidence rate varies according to the geographical location. Statistics from the Saudi Prostate Cancer Management Guidelines group showed that a total of 1869 cases of prostate cancer were recorded in Saudi Arabia between 1994 and 2004 and a considerable number of patients present with disease at an advanced stage [2]. Prostate biopsy is performed in men having raised PSA blood levels or with abnormal digital rectal examination findings. The Gleason grading method devised in the 1960s is an established prognostic indicator which is different from grading system of other cancers [3]. Gleason grading system was complex with a score ranging from 2-10 and Score 6 considered as lowest. Certain morphologic criteria for Gleason Pattern 3 were redefined and recommended as Pattern 4. New variants were also described. Therefore, grading underwent significant revisions and the new grading system was accepted by the 2016 World Health Organisation (WHO) with an aim to avoid confusion among treating urologists and the patients [4]. Thus, the present study aimed to analyse the pattern of prostate carcinoma and to compare with new grading system as proposed by WHO 2016.
Materials and Methods
This study was conducted in the Department of Pathology, Aseer Central Hospital, Abha, Kingdom of Saudi Arabia (KSA) from January 2015 to December 2017. The biopsies obtained from Trans Rectal Ultrasound Guided (TRUS) and Transurethral Resection of Prostate (TURP) positive for malignancy were included in the study. The laboratory data were collected from histopathology unit and the clinical data obtained from urology department. The haematoxylin and Eosin (H&E) stained sections and relevant immunostains {Prostate Specific Antigen (PSA), high molecular weight cytokeratin, synaptophysin} of formalin fixed paraffin embedded blocks were reviewed again by histopathologist. The basic statistical analysis of cases and findings were applied manually, which has been represented by percentages and tables and sensitivity and specificity of conventional (old) Gleason Scoring (GS) was calculated in comparison to new Grade Grouping (GG).
Results
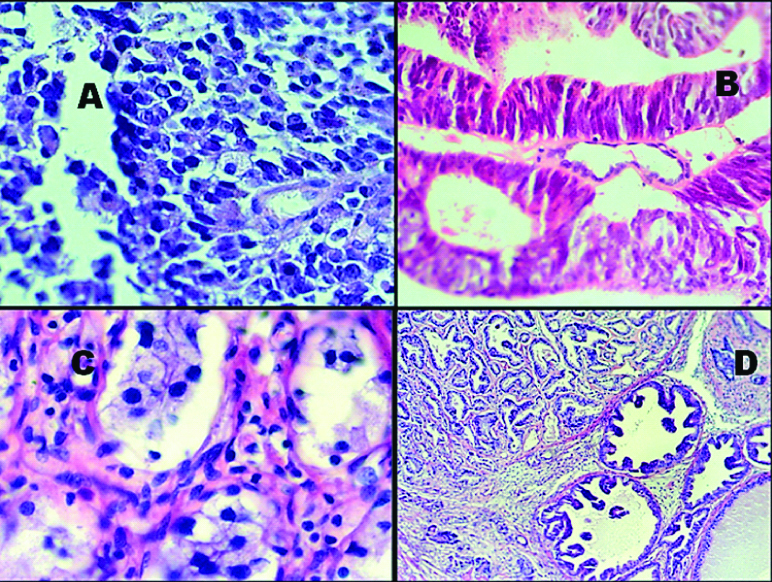
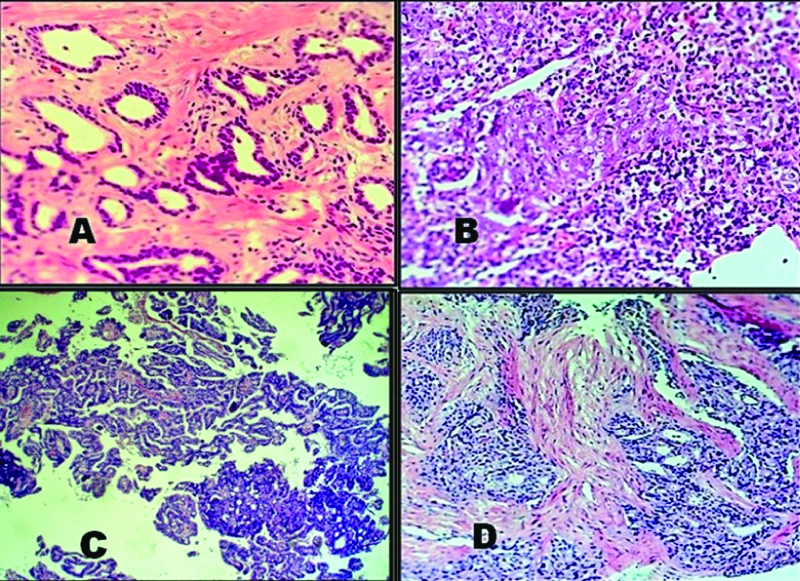
A total number of 47 cases of prostate cancer were collected out of which 33 (70.2%) were TRUS and 14 (29.8%) were TURP biopsies. All the cases were above 50 years of age. Four patients (8.5%) between 50-60, 14 (29.8%) between 60-70, 21 (44.7%) between 70-80, five (10.6%) between 80 to 90, 2 (4.2%) were between 90-100 years of age. One patient (2.1%) was 101-year-old. Histopathological examination revealed 44 (93.6%) cases of adenocarcinoma and 3 (6.4%) cases of small cell carcinoma. Twelve histological variants were noted, which are of diagnostic implications and prognostic significance. Ductal adenocarcinoma had papillary and tall columnar cell type of patterns (one case each) [Table/Fig-1,2 and 3].
Summarises the significant histologic types and variants of prostatic adenocarcinoma.
| Characterstic | Number of cases/Total 47 cases | Percentage |
|---|
| Histological variants | | |
| Small cell | 3 | 6.38 |
| Foamy cell | 1 | 2.12 |
| Ductal adenocarcinoma | 2 | 4.25 |
| Atrophic | 2 | 4.25 |
| Signet ring | 1 | 2.12 |
| Pseudohyperplastic | 2 | 4.25 |
| Lymphoepithelioma like | 1 | 2.12 |
| Carcinoma with squamous differentiation | 1 | 2.12 |
| Carcinoma with urothelial differentiation | 2 | 4.25 |
| Acinar adenocarcinoma | 32 | 68.08 |
| Total | 47 | 100 |
A) Prostatic adenocarcinoma- small cell variant (H&E 400x); B) Prostatic adenocarcinoma- ductal adenocarcinoma with tall columnar cells and pseudostratification (H&E 200x); C) Prostatic adenocarcinoma-foamy cell variant (H&E 400x); D) Prostatic adenocarcinoma-pesudohyperplastic variant (H&E 200x).
A) Prostatic adenocarcinoma-atrophic variant (H&E 200x); B) Prostatic adenocarcinoma-lymphoepithelial variant (H&E 200x); C) Prostatic ductal adenocarcinoma-papillary variant (H&E 200x); D) Prostatic adenocarcinoma-urothelial differentiation (H&E 200x).
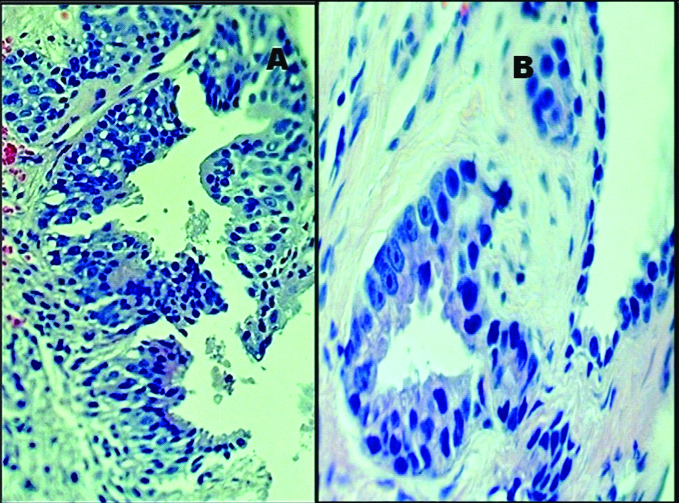
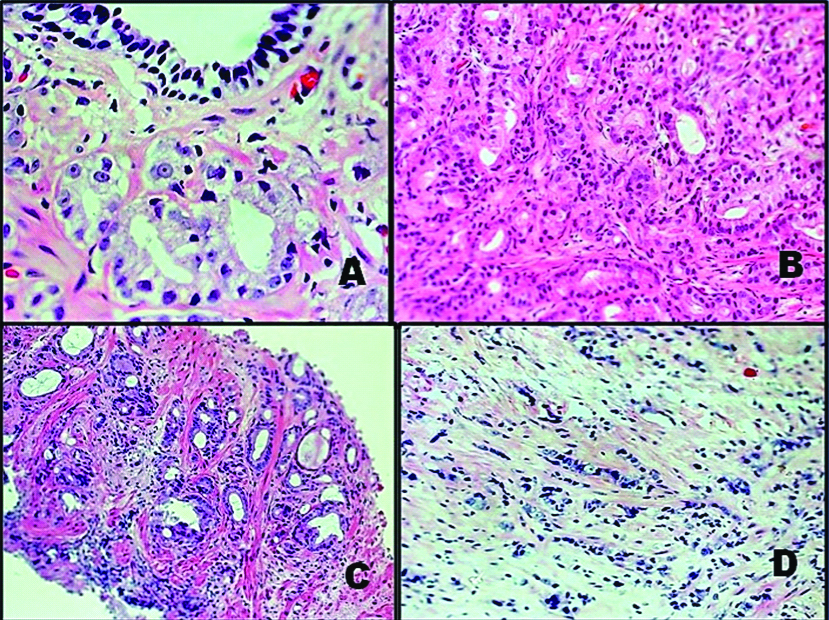
Prostate Intraepithelial Neoplasia (PIN) was observed in 10 (21.2%) cases; which includes six cases of High Grade PIN (HG-PIN) with three cases of retrograde spread [Table/Fig-4]. HG-PIN were tufting (3 cases), micropapillary (2 cases) and flat pattern (one case). The cases were graded as per modified Gleason grading system and scored by adding the most common patterns and the second common pattern and grouped according to new grading system [4]. Six cases with well-formed glands were GG 1 having a GS of 3+3=6. Five cases were in GG 2 (3+4=7) and four with scores of 4+3=7 (GG 3). A total of 3+4 shows predominantly well-formed glands with a lesser component of poorly formed/fused/cribriform glands while 4+3 has predominantly poorly formed/fused/cribriform glands with a lesser component of well-formed glands. Four cases (4+4=8) were in GG 4 (GS 8) indicates any combination of primary or secondary grades amounting to score of 8, while GG 5 (GS 9, 10) lacks gland formation or shows necrosis with or without poorly formed/fused/cribriform glands. Maximum number of 25 cases (53. 18%) were in GG 5 [Table/Fig-5a, 6]. Three cases which were previously assigned 3+3=6 were found to be 3+4=7 and one case with 3+4=7 score was re-scored as 4+3=7. Three cases which were previously reported as 5+3=8 were scored as 5+4=9. One case where both Pattern 3 and 5 were approximately 5% along with predominant Pattern 4 and was reassigned as 4+5. Thus, eight cases (17%) were regrouped by the present retrospective analysis according to new grading system. Revised GS resulted in upward shift of scores in 8 cases [Table/Fig-5b]. Classifying them into GG is simpler to understand. Determination of patterns especially Pattern 4 and their percentages becomes important which changes he GG and hence the treatment strategy. Thus in the present study, old system of GS was found to be less sensitive (90.9%) and specific (95.45%) as compared to new GG.
A) High grade PIN with tufting pattern. (H&E 400x); B) Retrograde PIN (H&E 400x)
Categorisation of prostate carcinoma cases as per latest WHO 2016 grade groups.
| Grade Group (GG) | Gleason Score (GS) | No. of Cases | Percentage |
|---|
| 1 | 3+3 | 6 | 12.77 |
| 2 | 3+4 | 5 | 10.64 |
| 3 | 4+3 | 4 | 8.51 |
| 4 | 8 | 4 | 8.51 |
| 5 | 9 (4+5)9 (5+4)10 (5+5) | 1393 | 25 | 53.19 |
| Small cell | | 3 | 6.38 |
| Total | | 47 | 100 |
Comparison of old GS and new Gleason GG.
| Old Gleason Score (GS) | No. of cases | NewGrade Groups (GG) | No. of cases |
|---|
| 6 (3+3) | 9 | 1 (3+3) | 6 |
| 7 (3+4, 4+3) | 6 | 2 (3+4) | 5 |
| 8 (4+4. 5+3) | 8 | 3 (4+3) | 4 |
| 9 (4+5, 5+4) | 18 | 4 (4+4, 5+3) | 4 |
| 10 (5+5) | 3 | 5 (4+5, 5+4, 5+5) | 25 |
| Total | 44 | | 44 |
A) Prostatic adenocarcinoma-Grade 3+3 (GG 1) H&E 400x); B) Prostatic adenocarcinoma-Grade 4+3 (GG 3) (H&E 200x); C) Prostatic adenocarcinoma-Grade 3+4 (GG 2) (H&E 200x); D) Prostatic adenocarcinoma-Grade 5+5 (GG 5) (H&E 100x).
Invasion was reported in 30 cases (63.82%) with perineural invasion most common [Table/Fig-7]. Twenty-one cases (70%) out of 30 where invasion was identified were in GG 5. Also, more cases of invasion were seen in GG3 i.e., 4+3 as compared GG 2 i.e., 3+4 [Table/Fig-8]. PSA was more than 10 ng/mL in 38 (80.85%) cases out of which eleven (23.4%) cases had PSA level above 100 ng/mL. Nine cases (19.15%) had PSA between 4 to 10 ng/mL.
Invasion seen on biopsy in different Grade Groups.
| Invasion | Grade Groups (GG) |
|---|
| 1 | 2 | 3 | 4 | 5 |
|---|
| No. of cases (30) | | 1 | 4 | 4 | 21 |
Various types of invasion seen on biopsy with Different Gleasons Patterns.
| Invasion | Gleason’s score of associated cancer |
|---|
| 3+3 | 3+4 | 4+3 | 4+4 | 4+5 | 5+4 | 5+5 |
|---|
| Perineural | | 1 | 2 | 2 | 9 | 5 | 3 |
| Periprostatic fat | | | | | 5 | 1 | 1 |
| Seminal vesicle | | | 1 | | 3 | | 1 |
| Lymphovascular | | | 1 | | 5 | | 2 |
| Retrograde ductal | | | | 2 | 1 | | |
Discussion
The prevalence and incidence of prostate carcinoma vary in different parts of the world. Though it is one among the most common cancers, mortality rate due to prostate adenocarcinoma is relatively low compared to other common cancers among men. The number of deaths were 20.1 per 100,000 men per year based on Surveillance, Epidemiology, and End Results (SEER) summary 2010-2014 [1]. In Saudi Arabia, the International Agency for Research on Cancer (IARC) estimated that the age-standardised incidence rate for prostate cancer was 7.7 per 100,000 men in 2008, and the age-standardised mortality rate was 5.1 per 100,000 men which is much lower than developed countries [5]. There were 47 cases in three years in our study in a tertiary hospital of Aseer province which has a population of 2.2 million [6].
The most commonly followed method of grading cancer of prostate is Gleason grading which has significantly modified after two major revisions [7,8].
The new knowledge in the pathology and genetics of prostate cancer has lead to ISUP 2014 multidisciplinary consensus conference, from which evolved new five GG system as opposed to multiple possible scores depending on various Gleason pattern combinations. GG 1=GS≤6, GG 2=GS 3+4=7, GG3=GS 4+3=7, GG 4=GS8, GG 5=GS 9 and 10 [9].
Initial Patterns 1 and 2 are recently described as mimickers of carcinoma, such as adenosis or partial atrophy. Therefore the grading starts from Pattern 3 and lowest Gleason’s score becomes 3+3=6 [7].
A new five GG system has been developed opposed to multiple possible scores depending on various Gleason pattern combinations. GG 1=GS≤6, GG 2=GS 3+4=7, GG 3=GS 4+3=7, GG 4=GS 8, GG 5=reporting particularly 3+4 and 4+3. The prognosis of patients under previous three-tier system of GS 6,7 and 8-10 were found to be of different under this new grade groups. Studies have shown poorer pathological stage and biochemical recurrence for 4+3 as compared to 3+4 [10,11].
Also, the lowest score assigned as 6, although it is on a scale of 2-10 leads to an incorrect assumption on the part of patients that their cancer is in the middle of the scale, believing that the cancer is more serious. The new five GG system removes this dilemma and therefore reduces overtreatment of indolent prostate cancer. Authors reclassified the present cases according to these GG.
Atrophic, pseudohyperplastic, foamy gland, and microcystic variants of acinar adenocarcinoma that may be deceptively benign have been emphasised in WHO classification. They are assigned a grade of 3[ 4,12]. Authors reported cases of atrophic, pseudohyperplastic and foamy gland type and graded them accordingly.
Signet ring, sarcomatoid, and pleomorphic giant cell adenocarcinoma variants of acinar adenocarcinoma have worse prognosis. Microcystic adenocarcinoma and pleomorphic giant cell adenocarcinoma are newly recognised variants in the WHO 2016 classification [4,12].
Small cell carcinoma, an aggressive high-grade neuroendocrine carcinoma should be diagnosed without assigning a Gleason grade. Authors reported three cases of small cell which were Cytokeratin and synaptophysin positive. In case of mixed small cell carcinoma and adenocarcinoma, the prostatic adenocarcinoma component should be given a GS, although the small cell carcinoma component is still not graded.
Mucinous adenocarcinoma, a variant diagnosed in the presence of extra glandular mucin should be graded based on the underlying pattern. Intracytoplasmic vacuoles and signet ring like features should not influence the grade, and like mucinous carcinoma, the grade should be assigned based on the underlying architectural pattern as if the intracytoplasmic vacuoles were not present. We had one case with signet ring cells and was assigned grade Pattern 5. Prostatic duct adenocarcinoma, a distinctive entity, with its tall, pseudostratified columnar cells is graded as Gleason Pattern 4 if without necrosis. Authors reported two cases of ductal adenocarcinoma one with tall columnar cells and other with papillary pattern. Most prostatic duct adenocarcinomas have a cribriform pattern and are given the Grade 4, also ductal adenocarcinoma with papillary architecture and true fibrovascular cores are graded as Gleason Pattern 4.
Hypernephromatoidpattern 4 is no longer recommended to be used. It has also been indicated that pattern 5+3 is not clinically correct and most of these cases are either 5+4 or 5+5 if thoroughly examined. In the present study, three such cases were corrected to 5+4.
Previously primary (most common) and secondary (second most common) patterns were reported and a minor component of higher-grade cancer, if present, was not mentioned [4,8]. Tertiary patterns are recorded only on radical prostatectomies and not on needle biopsy. The usual situation with 3-grade patterns is a core with Gleason Patterns 3, 4, and 5. The Gleason score is determined by adding the most common pattern with the highest-grade pattern and typically not mentioning the remaining pattern. Low-grade pattern of less than 5% is not significant, whereas high-grade pattern of any quantity is to be included in GS [7,8].
In the present study, invasion was reported in 30 cases (63.82%). Twenty-one cases out of thirty cases where invasion was identified were in GG 5 (GS 9, 10) making it obvious that higher grade groups are associated with bad prognosis. Also, incidence of invasion was more in GG 3 i.e., 4+3 as compared to GG 2 i.e., 3+4. The 5-year biochemical risk-free survivals for the 5 GG based on radical prostatectomy was found to be GG 1 – 96.6%, GG 2-88.1%, GG 3 – 69.7%, GG 4 – 63.7%, GG 5 – 34.5 % in one study and 96% for GG 1, 88% for GG 2, 63% for GG 3, 48% for GG 4, and 26% for GG 5 in an another important study [10,11].
However, the problem of inter-observer variability on the Gleason grading and grouping is only moderate and the new Gleason GG has not improved inter-observer agreement [13].
Limitation
This is only a retrospective study where histopathological re-evaluation of prostatic carcinoma was done in light of new WHO grading system. A further study is recommended involving large numbers of cases to find out inter observer variability and long term follow-up of patients for prognosis.
Conclusion
The study compared prostate cancer using the conventional and 2016 WHO modified Gleason system. New five GG system removes the dilemma of old GS with lowest Score 6 on a scale of 2-10. New variants of adenocarcinoma emphasised in WHO 2016 classification are identified and graded accordingly. Determination of patterns especially Pattern 4 and their percentages become important which changes the GG. The old system of GS is less sensitive (90.9%) and specific (95.45%) as compared to new GG.