The Global Burden of Disease ranked Low Back Pain (LBP) in top as a clinical condition with disability and ranked sixth under disability-adjusted life years [1,2]. LBP of 12 weeks longer duration or lasting LBP is termed as Chronic Low Back Pain (CLBP) [3]. Around (10-40%) of individuals experience chronic LBP which causes economic burden to the society [4,5].
The increased CLBP prevalence rate (19.6%) was observed between 20 and 59 years than between 24 and 39 years (4.2%) individuals. CLBP is more prevalent in women between 30 and 60 years [6] and noted in 6.2% of general population and 92% in construction workers in specific to Indian population [7].
CLBP can be approached with various treatment options such as drug therapy, surgical interventions and other non invasive interventions like physical therapy and psychological therapy. One of the most effective treatment possibility of CLBP is exercise therapy [3,8,9]. The recent evidences on therapeutic exercise suggest that no form of therapeutics is superior to another [3,8].
Exercises have shown to have slight impact on functional improvement and pain reduction in non specific CLBP [8]. The national and international guidelines recommend exercise therapy for treating CLBP [10]. The concept of motor control in CLBP has been viewed by many researchers [11-14]. It is believed that pain cause impairment of movement and motor control [15,16].
Movement Control Impairment (MCI) is defined as limited active movement in the lumbar spine on performing functional tasks. CLBP patients tend to have reduced movement control or control impairment which provokes pain [12]. Various researches hypothesised movement control deficits fall under a large subgroup of LBP and can benefit from specific exercises [12,13]. All forms of low back pathologies as like nerve root pain, peripheral neuropathic and centrally mediated pain will lead to altered motor behavior [12,17].
The efficient treatment option in CLBP lies in sub grouping into homogenous groups and imparting of tailored interventions. Further the effectiveness of movement control exercises in sub-groups of spinal instability and spondylolisthesis were found to be beneficial [18,19]. An updated systematic review in motor control exercises on chronic non specific LBP [20] suggests the need for analysing its efficacy in target subgroups.
The future scope in CLBP suggests that core stability is a subset of motor control [21] and assessment of motor control using tests as proposed by Luomajoki H et al., is warranted [22]. Several systematic reviews and meta-analysis has highlighted the importance of stabilisation program and core stability program [23-27]. The concept of sub grouping based on motor control has not been adopted widely. The method of tailor made motor control exercises based on the type of impairments was studied sporadically. Hence the current study intends to evaluate the efficacy of motor control training program in CLBP using pressure biofeedback.
Materials and Methods
The present study was quasi-experimental study (pre-post design) which was conducted at the Outpatient Physiotherapy Department, Sri Ramachandra Hospital, Chennai Tamil Nadu, India. Study was approved by the ethics committee for students’ projects, Sri Ramachandra Medical College and Research Institute (REF: CSP/17/AUG/60/248). The recruitment process was started in December 2017 and completed by April 2018 with two weeks follow-up for all participants. A verbal explanation of the research project was made followed by an informed consent process.
Participants and Sample Size
Subjects with CLBP (pain greater than 12 weeks); with signs of centralization and decreased core muscle strength and motor control impairment were recruited for the study. Spinal surgery, abdominal surgery within last 12 months or specific spinal pathology (Inflammatory joint diseases, tumour, and fracture) and pregnant women were excluded. The estimated sample size was calculated using comparison of two means (Power-80%, CI-95%), needed at least 24 participants. Anticipating 20% loss to follow-up, sample size was rounded to 30.
The subjects who met the inclusion criteria were randomly assigned to two groups i.e., control group and experimental group based on convenient sampling method. A standardised physical therapy care was given for all subjects by experienced physiotherapist after initial evaluation. Both groups received exercises to improve pain, functions and enhanced quality of life.
Motor control assessment and training: The subjects in the experimental group were assessed for motor control impairments. The motor control tests [22] include waiters bow (flexion control), prone knee bend (extension control and rotation control), and sitting knee extension (flexion control) were administered to identify the type of impairment. All these tests are active test where the subject is asked to perform and any abnormal or excessive movement is noted.
Waiter’s Bow Test [22]
The test is done in upright standing by flexing the hips without causing movement of the low back region (flexion). Ideally, no movement of the low back is expected with hip flexed to 50-70°. Flexion control impairment is confirmed if low back movement is observed with hip flexion angle less than 50°.
Sitting Knee Extension Test [22]
The subject is positioned in upright sitting and instructed to extend the knee without causing movement of the low back region (flexion). Normally, 30-50° knee extension occurs without movement in low back region. If low back moves in flexion while extending the knee, the presence of flexion control impairment is diagnosed.
Prone Knee Bend Test [22]
The test is done in prone lying with knee flexion to 90° without causing movement in low back region and pelvis. If the low back does not stay in neutral while flexing the knees (either the lumbar spine goes into extension or pelvis into rotation) then extension control or rotation control is said to be impaired. According to the type of impairment, specific control impairment exercises [22] were taught with appropriate dosage.
Control impairment exercises: The procedures of exercise are performed in seated or standing position with lumbar spine in neutral posture. Initially the subjects are instructed to squat and to stand by maintaining the spine in neutral through verbal commands and minimal assistance. Sitting knee extension exercise is performed in sitting at the edge of the couch, instructions are provided to extend one knee without flexing the lumbar spine. The exercise regime is progressed to quadruped position (four point kneeling) with spine in neutral and subjects are instructed to rock pelvis backwards [Table/Fig-1].
Squatting-Lumbar spine in neutral position.

The extension control impairment exercises prevent the lumbar spine from moving into excessive extension. The exercises include posterior pelvic tilting in crook lying and prone lying position in neutral spine which can control excessive lumbar spine extension. The prone straight leg raising exercise was performed with a pillow placed under the abdomen for maintaining the lumbar spine in neutral and unilateral leg lift maneuver was performed [Table/Fig-2].
Prone straight leg raise-Lumbar spine in neutral position.

Rotation control impairment exercises were prescribed to avoid excessive pelvic rotation and lumbar spine movements during lower limb activities and control is gained by maintaining the spine in neutral position. In prone position, with knee flexion the limb is moved in to rotation without causing any movement of lumbar spine. This procedure is further progressed in crook lying with one limb is moved into abduction without pelvic rotation. In side lying position, one of the limbs is abducted with lumbar spine and pelvis in neutral. The control impairment exercises have been advised to be performed 20 repetitions and two sessions per day.
Standard Care
The subjects in the control group received an electrotherapeutic agent for pain relief, basic core stability exercise (abdomen-drawing in maneuver in crook lying position). The muscle contractions were held for 10 seconds and repeated for 10 times. Lower limb flexibility exercises for hamstrings, gluteals and piriformis muscle groups were educated with dosage of 30 seconds and repeated for three times. The subjects underwent three treatment sessions per week for two weeks. All outcomes were measured at baseline and after two weeks of training.
Outcomes
Baseline measures of Fear Avoidance Beliefs Questionnaire (FABQ) comprising physical activity (FABQ-PA) and work (FABQ-W) subscales were recorded [28]. The subjects were assessed for pain characters and severity of pain was documented using a 10-point numerical pain rating scale [29]. All the details were secured and the same assessment procedure was followed at the end of the session for the analysis.
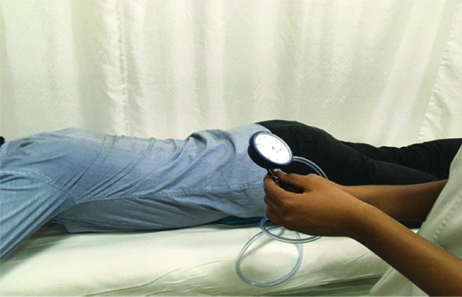
The Chattanooga stabiliser pressure biofeedback unit was used to measure the change in pressure of Transversus Abdominis (TrA) muscle contraction [11]. The tool has been validated by imaging studies and is considered as gold standard in measuring TrA contraction [30]. The subject positioned in prone lying, the pressure biofeedback unit was inflated to 70 mm Hg was placed under the abdomen and was asked to perform a drawing in maneuver. A decrease or increase in the pressure (normally the pressure should decrease by 6-10 mm Hg) during the drawing in maneuver was noted. The subject was instructed to sustain the pressure drop for up to 10 seconds [Table/Fig-3] [31].
Transversus abdominis facilitation.
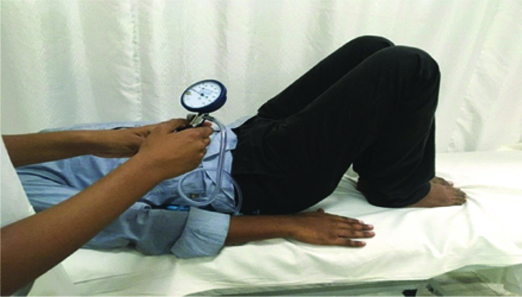
The corseting effect of lumbar core muscles was measured by placing the patient in supine/crook lying; the pressure biofeedback is placed in the lumbar lordosis (centered about L3). The pad was inflated to a base pressure of 40 mm Hg. A decrease or increase in the pressure (normally the pressure should decrease by 5-10 mm Hg) during the drawing in maneuver was noted. The pressure decreased was asked to be consistently maintained [Table/Fig-4] [11,30].
Corseting effect of lumbar core muscles.
Assessment of Lumbar Core Muscle Strength using Pressure Biofeedback
The Roland Morris Disability Questionnaire is a reliable [32] and valid [33] tool in measuring the level of disability in LBP. The tool is available in public domain and is free to use, comprising 24 items measuring subject’s perception in activities of daily living. The scoring of item with 0 indicates no difficulty and 1 indicates difficulty in activities of daily living. The overall scores fall between 0 to 24, with a greater score predicting activity limitation. The scores are interpreted by calculating the percentage of improvement based on pre and post scores.
Statistical Analysis
The statistics was calculated using website for statistical computation (http://vassarstats.net/). The descriptive statistics, percentage analysis was used for categorical variables and the mean and SD was used for continuous variables. The normality of data was verified using Shapiro-Wilk test. Independent t-test was used to compare the control and experimental group for normal data. The between group analysis of skewed data (pain severity) was done by Mann Whitney U test. Paired t-test was used to analyse the within group analysis of all variables. Pearson Correlation Coefficient was used to analyse the relationships between variables. The statistical tests were considered significant when the p-value<0.05.
Results
A total of 30 subjects were included in the study and all subjects completed the follow-up at two weeks. The demographic characteristics of both groups are outlined in [Table/Fig-5]. A total number of 12 males and 18 females participated in the study. All baseline values of pain severity, lumbar core muscle strength and functional outcome in both groups were found similar and statistically insignificant.
| Control group (N=15) mean (SD) | Experimental group (N=15) mean (SD) | p-value |
|---|
| Age (years) | 39.6 (8.34) | 44.7 (10.11) | 0.35 |
| Strength of Transversus abdominis (mm Hg) | 70.06 (1.23) | 70.73 (1.70) | 0.69 |
| Strength of corseting effect. (mm Hg) | 40.86 (0.54) | 40.46 (0.95) | 0.94 |
| Pain severity | 7.46 (0.65) | 7 (0.51) | 0.48 |
| Level of disability | 14.73 (1.89) | 15 (2.42) | 0.22 |
| FABQ (PA) | 20.6 (4.82) | 19.86 (4.15) | 0.76 |
| FABQ (W) | 33.6 (6.34) | 34.33 (5.07) | 0.74 |
FABQ: Fear avoidance belief questionnaire; PA: Physical activity; W: Work
The between group analysis in [Table/Fig-6] shows statistically significant improvements (p-0.01) in pain reduction, corseting effect (p-0.01) and transversus abdominis muscle strength (p-0.04) in experimental group. The experimental group also showed more functional improvement than the control group.
Analysis of outcomes between groups.
| Variables | Control mean (SD) | Experimental mean (SD) | Mean difference | p-value |
|---|
| Pain severity (NPRS)1 | 4.06 (0.96) | 2.66 (0.72) | 1.4 (0.53-0.39) | 0.01* |
| Corseting effect-strength of Lumbar core muscles contraction (mm Hg)2 | 39.33 (0.97) | 37.13 (1.45) | 2.2 (0.53-0.80) | 0.01* |
| Transversus abdominis strength of contraction (mm Hg)2 | 67.46 (2.23) | 65.06 (1.86) | 2.4 (1.23-1.03) | 0.04* |
| Functional improvement (RMDQ)2 | 30.60 (18.44) | 44.46 (16.15) | 13.86 (10.19-8.92) | 0.03* |
NPRS: Numerical pain rating scale; RMDQ: Roland morris disability questionnaire; CI: Confidence interval 1-Mann Whitney U test; 2-Independent t-test; * -Significant at p<0.05
[Table/Fig-7] represents the pre-post analysis of pain severity and strength of lumbar core muscles in the control group and experimental groups. Statistically significant (p-0.001) pain reduction and improvement in the lumbar core muscle strength and functional outcome was noted within both groups.
Pre-post analysis of outcomes in both groups.
| Variables | Control group (n=15) | Experimental group (n=15) |
|---|
| Baseline mean (SD) | Final mean (SD) | Mean difference | p-value | Baseline mean (SD) | Final mean (SD) | Mean difference | p-value |
|---|
| Pain severity (NPRS) | 7.46 (0.65) | 4.06 (0.53) | 3.4 | 0.001* | 7 (0.51) | 2.66 (0.39) | 3.06 | 0.001* |
| Corseting effect-strength of contraction (mm Hg) | 40.86 (0.54) | 39.33 (0.53) | 1.53 | 0.001* | 40.46 (0.95) | 37.13 (0.80) | 3.33 | 0.001* |
| Transversus abdominis-strength of contraction (mm Hg) | 70.06 (1.23) | 67.46 (1.23) | 2.6 | 0.01* | 70.73 (1.70) | 65.06 (1.03) | 5.67 | 0.001* |
NPRS: Numeric pain rating scale; Paired t-test; *- Significant at p<0.05
[Table/Fig-8] represents correlation between FABQ subscales and physiological variables. A strong positive correlation was noted (r=0.52) between FABQ-physical activity and baseline pain and also between FABQ- physical activity subscale and strength of transversus abdominis (r=0.45) in the experimental group. A negative correlation was noted (r=-0.23) between FABQ-work subscale and baseline pain and also between FABQ-work subscale and the strength of transversus abdominis (r=-0.28) in the experimental group.
PrCorrelation between FABQ subscales and physiological variables.
| Component 1 | Component 2 | r value | p-value |
|---|
| FABQ-physical activity | Baseline pain (NPRS) | 0.52 | 0.04* |
| FABQ-work | -0.23 | 0.05* |
| FABQ-physical activity | Transversus abdominis activation | 0.45 | 0.04* |
| FABQ-work | -0.28 | 0.04* |
FABQ: Fear avoidance belief questionnaire; Pearson correlation coefficient; *- Significant at p<0.05
Discussion
This is the first experimental study analysing the effectiveness of specific motor control training based on impairments in CLBP. The salient features of the current research are incorporating a battery of tests to categorize flexion control, extension control and rotation control impairments. Secondly, we found the study protocol imparted motor control impairment exercises for a period of two weeks which improved overall functions in CLBP population. Moreover the study findings denote all subjects in experimental group had control impairment and none with movement impairment was typically observed in CLBP. It was observed that motor control training was not influenced, in spite of strong presence of fear beliefs [34].
The Numerical Pain Rating Scale has been an effective pain outcome measure in CLBP [35]. The MCID for NPRS in musculoskeletal conditions is two points [36] but the current study, difference of three points in both the groups depicted clinical significance of reduced pain severity. This finding of the current study is in accordance with the meta-analysis [27] which stated that motor control exercises reduced pain than general exercises and also better than minimal intervention in chronic and recurrent LBP. However, minimal reduction of pain in CLBP for a shorter duration of training supports the significance of control impairment exercises [37].
The pressure biofeedback manufacturers claim an accuracy rate of plus/minus 3 mm Hg [39]. Studies [30,31] have specified a 4 mm Hg pressure reduction in TrA muscle activity for a real change in strength of contraction [39]. The current study finding of 3.33 mm Hg (corseting effect of TrA and multifidus) pressure reduction which accounts near normal and 5.67 mm Hg pressure reduction (TrA) indicating improved lumbar core muscle control.
The motor control training group had more improvement of strength in corseting effect (37.13 mm Hg) and TrA (65.06 mm Hg) than the standard care. It has been proven that the motor control exercises improved the thickness of the lumbar spine core muscles in CLBP [40] which implies that increase in muscle thickness also will increase the strength of contraction.
The intra-rater measurement of the pressure biofeedback using three trials produced similar values of pressure that implies reproducibility of measures ranged from satisfactory to excellent [31]. Though the study was conducted for a limited period of time, there were about four subjects (26%) in the experimental group who had an improvement in the strength of TrA contraction and on the corseting effect (33%).
The minimal clinically important difference of Roland Morris Disability Questionnaire was estimated to be 30% reduction in score from its baseline [41]. A 73% of the subjects in the experimental group and 33% in the control group exhibited clinically meaningful improvements. A study [34] also depicted that the activity limitation caused by CLBP was reduced by motor control exercises within shorter time period of two months and this is in accordance with the current study results. Thus the motor control training sessions was not only found to exhibit statistically significant improvements but also clinically meaningful improvements in CLBP.
Thus this short duration trial resulted in significant clinical improvements but complete recovery in CLBP is purely based on longevity of care, duration of sessions and therapist skill in regaining motor control. The physiological basis of motor control training is based on the relearning principles of movement patterns and in functional activities facilitating corrected trunk muscle behavior [38]. Wide ranges of mechanism have been postulated to highlight the impact of motor control in pain mechanism. The process includes mechanical load reduction, enhanced coordination of muscular and movement control and these changes may be mediated by plastic changes in motor cortex [42].
Fear-Avoidance (FA) beliefs are significantly associated with the experience of chronic pain [43] which was noted in all subjects in the current study. A strong positive correlation was noted (r=0.5) between FABQ- physical activity and baseline pain in experimental group which signifies increase in pain intensity, the fear for avoiding physical activity also increases. A positive correlation was also noted (r=0.4) between FABQ- physical activity subscale and strength of TrA in experimental group which signifies that if the fear of the physical activity increases, there is increase of pressure in mmHg during TrA contraction denoting poor control of the contracting musculature.
A negative correlation was noted (r= -0.2) between FABQ – work subscale and baseline pain which implies if the fear for work increases, the tendency to avoid activity will pave way for decrement of pain severity. A negative correlation was noted (r= -0.2) between FABQ-work subscale and TrA activation implying that if the fear for work increases, the recruitment of the TrA muscle was found to decrease.
As studies have also shown the assessment of motor control is important in LBP [44], the current study has employed motor control tests and the effect of motor control training on lumbar core muscle strength. Hence CLBP patients are to be checked for motor control impairments and should be rendered appropriate motor control training according the impairment type for better clinical outcomes. The results of this study should be applicable to CLBP patients with presence of fear avoidance beliefs seeking active rehabilitation care. Moreover, appropriate physiotherapist training in control impairment exercises is highly recommended.
For future studies, sub grouping of the CLBP into three different impairments and treating them as an individual group is recommended. Supervised motor control training is expected to exhibit further clinical improvements. Using a musculoskeletal ultra sonogram an evidence based tool to visualize the thickness of the TrA muscle is also in need.
Limitation
The study limitations include limited duration of intervention, subject’s comprehensive capacity of the exercises as many could not follow the commands for exercises. Adherence to exercise at home was also not monitored and this could also be one of the reasons for the less amount of improvement in the outcomes. The experimental group included all of the impairments as a single group and sub grouping of the impairments was not done.
Conclusion
The interventional study on motor control training in CLBP concludes motor control exercises was effective in improving the lumbar core muscle strength, corseting effect and functional improvement in CLBP.
FABQ: Fear avoidance belief questionnaire; PA: Physical activity; W: Work
NPRS: Numerical pain rating scale; RMDQ: Roland morris disability questionnaire; CI: Confidence interval 1-Mann Whitney U test; 2-Independent t-test; * -Significant at p<0.05
NPRS: Numeric pain rating scale; Paired t-test; *- Significant at p<0.05
FABQ: Fear avoidance belief questionnaire; Pearson correlation coefficient; *- Significant at p<0.05