Introduction
As a contagious, parasitic dermatosis, scabies has been widely distributed throughout the world; it annually affects 300 million people from all age groups and social classes [1,2].
The mite Sarcoptes scabiei causing scabies has a worldwide distribution. Infestation risk factors (nosocomial) include contact with fomites, animals, infected clothes or intimate contact with people other than their main partner [3,4]. In the classical case of a scabies infection, the number of mites is few (10-15 mites) [5].
S. scabiei are small white disc-like arthropods visible with unaided eye. Female mites (0.3-0.4 mm) have the ability to burrow into the layers of skin in 2-3 minutes, making a winding burrow with length ranging from few millimeters to several centimeters through the stratum corneum which can be extended by ~2-3 mm each day [5]. The female mite lay the eggs (2-3 per day) in the burrows which will be developed to larvae (2-4 days) and then into adults (10-17 days) during four weeks [5,6]. The life cycle of S. scabiei is 4-6 weeks. The adult mites and its products (faces, eggs and dead parasites) generate an immediate or delayed hypersensitivity reaction with scabies symptoms. In the classic type, lesions are most often present on the fingers, around the wrists, buttocks, axillae, feet, elbows, scrotum, breasts and nipples and sometimes the face attracted by mites [5].
Crusted scabies is a severe form of scabies that can occur in some persons who are immunocompromised (have a weak immune system), elderly, disabled, or debilitated. It is also called Norwegian scabies. It is estimated that patients with crusted scabies have up to 4,000 mites per gram of skin. People with crusted scabies are very contagious to other persons and can spread the infestation easily both by direct skin-to-skin contact and by contamination of tools such as their clothing, bedding, and furniture. This form of scabies was first observed in a Norwegian leprosy patient in 1848 [7,8].
In people who have had scabies before, symptoms usually become visible much shortly (1-4 days) after contact. The most common signs and symptoms of scabies are intense itching (pruritis), especially at night, and a pimple-like popular itchy rash. The itching and rash may affect much of the body or be limited to common sites such as wrist, elbow, armpit, webbing between the fingers, nipple, penis, waist, belt-line and buttocks. The rash also can include tiny blisters (vesicle) and scales. Scratching the rash can cause skin sores; sometimes these sores become infected by bacteria. Persons with crusted scabies may not show the usual signs and symptoms of scabies such as the characteristic rash or itching [9].
In some outbreaks, exploration for scabies only commence upon emergence of Healthcare Workers (HCWs) developing itching. Scabies outbreaks are frequently documented in long-term Care Facilities (LTCF) [10].
Topical scabicides possess neurotoxic impacts on mites, larvae and eggs [11]. Various agents (mostly topical) have been applied for scabies treatment. These agents contain 5 to 10% sulfur in paraffin (an agent widely employed in Africa and South America) [8] 1% lindane, which has been prohibited in many western countries due to neurotoxicity concerns [12], 10 to 25% benzyl benzoate (often used in Europe and Australia), malathion [13], 10% crotamiton [14] and 5% tea-tree oil in combination with benzyl benzoate [9,15]. Topical 5% permethrin cream is considered as the first-line treatment [16].
Despite qualitative variations in methodology of trials, a recent meta-analysis determined topical permethrin as the most effective scabicide. Since its Food and Drug Administration (FDA) approval in 1989, permethrin (a synthetic pyrethroid insecticide), has been employed as a topical 5% cream for scabies treatment. Benzyl benzoate has been used as a safe drug in program treating scabies for 60 years [11].
Oral treatment is preferred in cases with difficulty in topical therapy. Oral ivermectin is a convenient substitution. It results in improved patient compliance and has shown usefulness in mass treatment for controlling endemic and epidemic cases [17].
Outbreak of scabies reported by researchers include lessons learned that can be used to prevent the prevalence of scabies in gathering locations. For example, an outbreak of scabies in hospitals, due to the entry of AIDS patients with Norwegian scabies, which infected nursing staff, doctors and services [18].
There are different opinions about treating people with scabies. In the study of Leppard B and Naburi AE. ivermectin 150 μg/kg was used for the treatment and prophylaxis of 1153 prisoners residing in a prison in northern Tanzania, which treated 95% of patients after eight weeks, but patients with Norwegian scabies were confronted with failure. It was suggested that topical treatment should be performed with ivermectin [19].
Lindane lotion was used for 30 years as a drug used to treat scabies but researchers reported concerns about toxicity to the nervous system, there are also studies of Hernandez-Perez E, Taplin D et al., Roth WI, which reported resistance to lindane. Therefore, the use of permethrin 1% in the treatment of this disease is recommended [20-22].
The aim of this study was to detect early disease scabies, finding its risk factors, and prevention of epidemic diseases among the people who are susceptible to scabies due to immune deficiency system.
Materials and Methods
Study Area
This was a descriptive cross-sectional study conducted in a rehabilitation centre, which is responsible for the care of disabled and mentally retarted people of Iran for a period of two months (In July 27 2018 until September 28, 2018 year). This centre had five units (A, B, C, D and E) comprising of 46 employees (34 staff; 2 nurses and 10 service personnel), catering to 110 handicapped persons.
Index Case
The index case of scabies in the disability centre was a 16-year-old boy with Down syndrome, who was in contact with the patients in Unit 5. In spring season 2018, symptoms of itching were caused in the person’s head and body, which according to the physician’s order, the patient were treated with permethrin shampoo 1% and leaves of the quarantine.
Clinical Examination and Case Definition
In July 27 2018, one outbreak of scabies was reported in a rehabilitation centre to one Centre Care Health (CCH) of Iran.
The patients and employees were examined by a team including entomologists and dermatologists and demographic information of the patients was collected by completing the questionnaire (with regard to the principles of medical ethics). Nineteen patients had symptoms of typical scabies including: skin itching; papule on testis and penis and generalised rash on the body and two patients (Norwegian) had thick crust on skin in armpit and anal. Four service personnel had papule on neck skin and two persons were pregnant. The clinical picture of Classic and Norwegian type of scabies seen in the body of mentally handicapped persons is shown in [Table/Fig-1]. In the present study, the five patient’s skin scrapings (because of the terrible behaviour of patients) were sent to the laboratory and mounted by potassium hydroxide (KOH). The mite microscope slide was analysed by entomologist. After receiving the laboratory results of the samples, simultaneous treatment of patients and non-patients was performed according to the choice drugs. All staff and nurses of this disability centre were also examined by a dermatologist.
The symptoms of Classic and Norwegian type scabies on the body of mentally handicapped person: a) Created rash in the armpit; b) Hand skin thickening; c) Skin lesion under armpit; d) Inflammation of the skin in the armpit; e) tiny burrows that can be seen in the skin; f) scabies blister on the skin (original picture).

Topical Treatment
On July 28, all mental patients were treated topically with 5% permethrin and for the chemo-prophylaxis of individuals residents in other units also used 5% permethrin (twice with one week interval), according to its protocol. The nurses, service personnel and staff of the centre received chemoprophylaxis and were treated by 10% crotamiton for two days, twice with one week interval, except for the pregnant woman’s service personnel who used 10% sulfur ointment for two or three weeks. As the disease was not found in other units, to prevent the epidemics, all disabled persons were cured with 5% permethrin cream twice with one week interval.
Risk Factors for the Incidence of Scabies
According to the opinion service staff, the risk factors for this disease were included:
The clothes of all disabled persons were received every day and they were washed in a large washer in contact with each other.
The towel of each unit was shared among all disabled persons.
Patients were accustomed to sleep on each other’s bed.
Residents of the units had skin contact with each other.
The service personnel were using one pair of gloves to wash the disabled person of any unit.
Bathroom cleaning supplies were commonly used between the patients.
Centre supporters and ordinary people with disability persons had skin contact.
The service personnel used common one bedspread and pillow for sleeping.
The inhabitants of each unit were accustomed to touch all the equipment in the centre with the hands.
Statistical Analysis
In this research SPSS, version 20 was used to analyse the data and then the relationships between factors (dependent) and genus and age indices (independent) variables were assessed through stepwise multiple regression analysis. The data normality was examined by Kolmogorov-Smirnov test.
For univariate description of data, the median, percentiles, range and frequency were given, and 95% Confidence Intervals (CI) of relative frequencies were calculated. For categorical data, the chi-square-test statistic for statistical significance was calculated and binary logistic regression was used for assessing the significance of the effect risk factors on prevalence scabies. The likelihood ratio statistic was used to test for statistical significance. Linear correlations between the risk factors and the incidence of scabies were calculated by Pearson’s correlation method.
Results
A total of 110 individuals with mental and physical disorders (23.6% males and 76.4% females) [Table/Fig-2] were resident in five units [Table/Fig-3] out of which 19% of individuals were exposed and 81% unexposed [Table/Fig-4]. The sex ratio of female to male was 3.2:1 [Table/Fig-2]. The mean age of patients was 27 years (SD=7.09, Range 14-48 years) and most affected age group was 21-30 years (45.4%), 92% of this group was females and 8% were males [Table/Fig-5]. In this study prevalence of scabies was 16.02%.
Frequency of gender disabled persons in care unit.
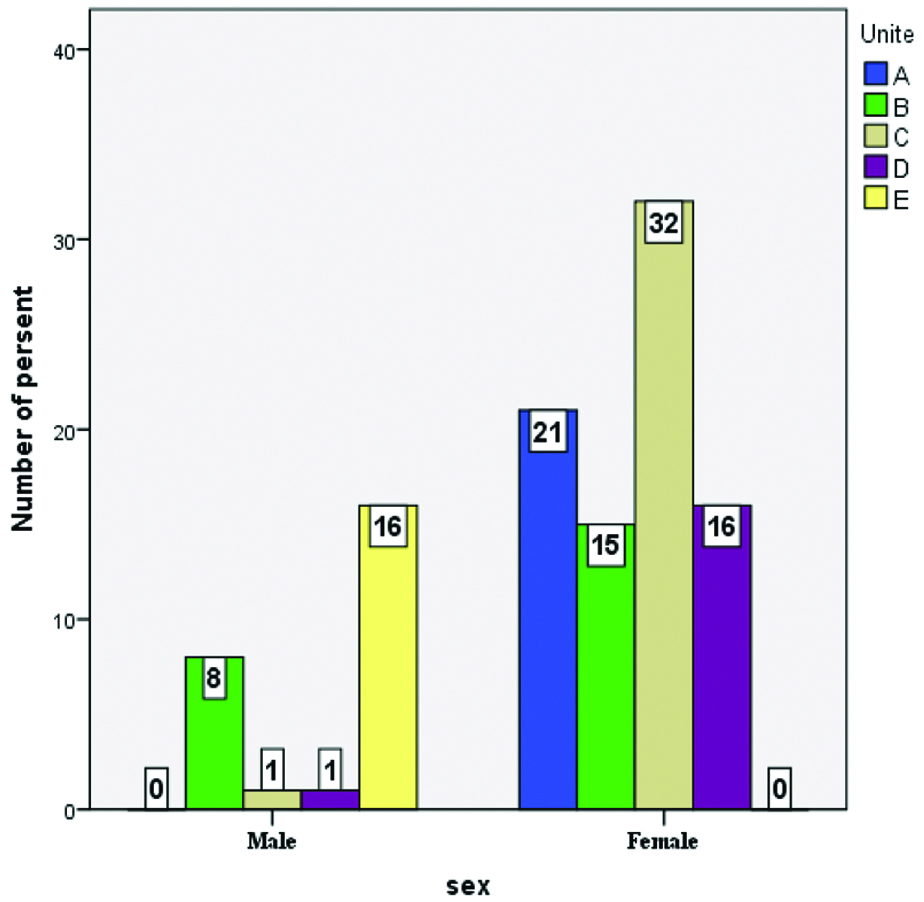
Frequency of scabies in care mental patient units according to the patient’s gender.
| Unite | No. of handicaps | Sex ratio | % infestation |
|---|
| A | 21 | 0 | 0 |
| B | 23 | 1.8:1 | 4.3 |
| C | 33 | 32:1 | 3 |
| D | 17 | 16:1 | 11.7 |
| E | 16 | 0 | 100 |
Age and gender of patients and service personnel with scabies in centre for mental and physical handicaps-2018.
| Patient | Age and gender | Treatment with permethrin 5%/crotamiton | Start of symptom | Age group and sex | OR (95% CI) | p-value |
|---|
| W2 | W3 |
|---|
| 1 | 26 F | Y | | 27 Jul | | | |
| 2 | 24 F | Y | | 27 Jul |
| 3 | 25 M | Y | | 27 Jul |
| 4 | 43 F | Y | | 27 Jul |
| 5 | 35 M | Y | | 27 Jul |
| 6 | 34 M | N | Y | 27 Jul | 15-30 | 1.1 (0.10-12.08) | 0.93 |
| 7 | 19 M | Y | | 27 Jul | 31-40 | 2.2 (0.20-24.26) | 0.50 |
| 8 | 20 M | Y | | 27 Jul | 41-50 | 0.52 (0.51-5.42) | 0.59 |
| 9 | 35 M | Y | | 27 Jul | Male and Female | 0.02 (0.005-0.08) | 0.00 |
| 10 | 33 M | Y | | 27 Jul |
| 11 | 30 M | Y | | 27 Jul |
| 12 | 18 M | Y | | 27 Jul |
| 13 | 33 M | Y | | 27 Jul |
| 14 | 31 M | Y | | 27 Jul |
| 15 | 15 M | Y | | 27 Jul |
| 16 | 14 M | Y | | 27 Jul |
| 17 | 33 M | Y | | 27 Jul |
| 18 | 34 M | Y | | 27 Jul |
| 19 | 23 M | Y | | 27 Jul |
| 20 | 32 M | Y | | 27 Jul |
| 21 | 30 M | Y | | 27 Jul |
| 22 | 46 F | Y | | 20 Jul |
| 23 | 39 F | Y | | 20 Jul |
| 24 | 42 F | Y | | 20 Jul |
| 25 | 44 F | Y | | 20 Jul |
W2: Second week; W3: The third week
The frequency of disabled people based on age year and sex.
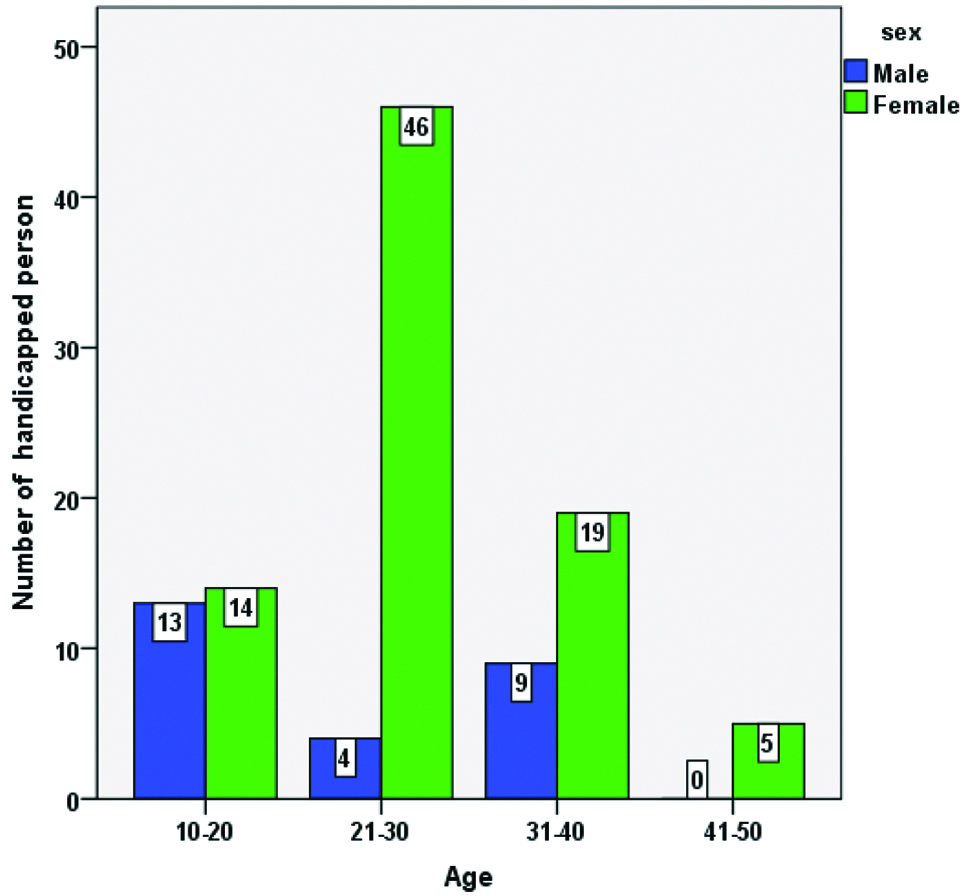
In this outbreak two mental patients were infected by Norwegian and 19 persons infected by classic type scabies. More of infected patients (11 male) were in 30-35 age groups [Table/Fig-4]. Only 4 females out of 46 staff had the symptoms of classic type of scabies. Here was a significant difference between the age and sex of the infected persons (p=0.015). Risk factors of the disease incidence were summarised in five factors including: washing clothes of the disabled patients together, sharing towel between patient (p>0.05), sharing bathroom supplies (p=0.04), sleeping in a common bed (p>0.05), were significantly associated with scabies and sharing glove (p=0.77) were factors that were not significantly associated with having scabies [Table/Fig-6].
Factors associated with scabies identified by logistic regression analysis.
| Variable | p-value | OR |
|---|
| Washing the clothes with each other | - | - |
| Sharing towel | >0.05 | 23.25 (8.91-60.64) |
| Sharing bathroom supplies | 0.04 | 3.31 (1.03-10.64) |
| Sleeping in a common bed | >0.05 | 23.25 (8.91-60.64) |
| Sharing glove | 0.77 | 0.86 (0.28-2.18) |
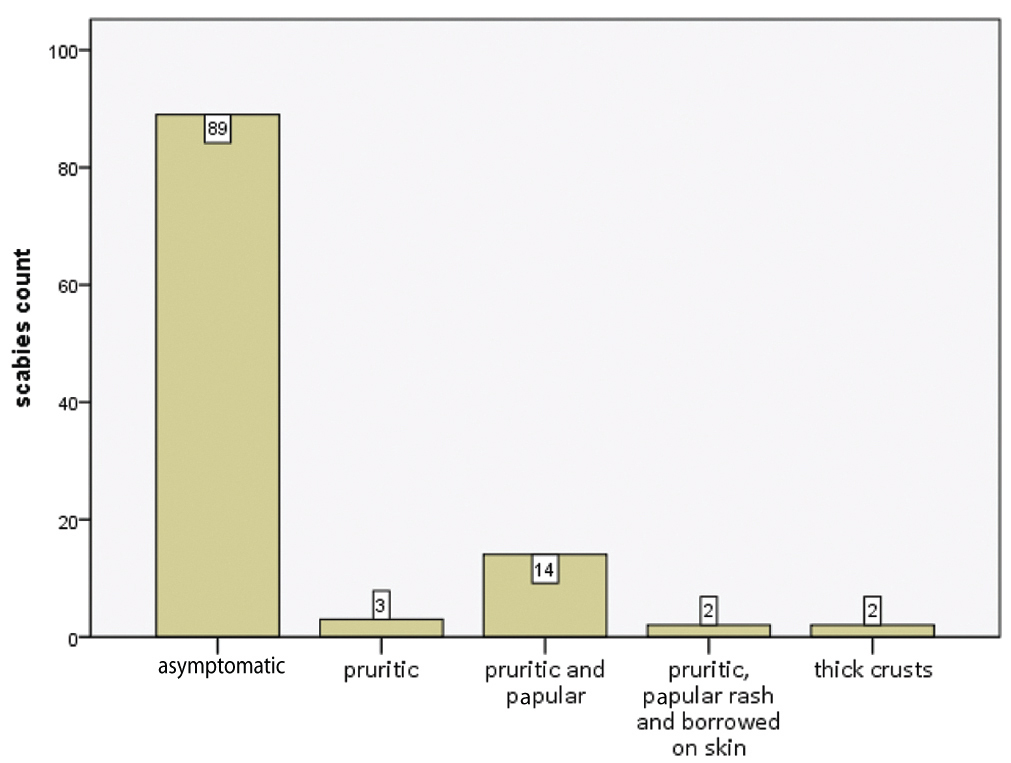
The result of logistic regression analysis is listed in [Table/Fig-6]. Using of sharing towels (odds ratio: 23.25, 95% CI: 8.91-60.64), sharing bathroom supplies (odds ratio: 3.31, 95% CI: 1.03-10.64), sleeping in a common bed (odds ratio: 23.25, 95% CI: 8.91-60.64) and sharing glove (odds ratio: 0.86, 95% CI: 0.28-2.18) were the most important risk factors of the scabies. In the study, three patients (2.7%) only had pruritic symptoms, 14 patients (12.7%) had pruritic and papular rash with excoriations, 2 patients (1.8%) were associated with pruritic, papular rash with excoriations and borrowed on skin and 2 patients (1.8%) had thick crusts [Table/Fig-7]. Twenty (95%) of the mental patients were treated with 5% permethrin cream for twice, within a week of each other and 5% were treated after three time and 100% of the staff that had symptom of scabies were cured with 10% crotamiton cream [Table/Fig-4].
The frequency of symptoms scabies in patients.
Discussion
This is the first ever study done in a population with specific physical, mental and walking health conditions, which often have problems with the control of scabies disease in this group. Those who are not educated and whose control and care require special conditions [18,19]. In this research, to prevent the spread of disease to other units, we recommend: 1) identification of infected patients by expert clinician; 2) prophylactic treatment with permethrin cream 5% for all exposed person; 3) use of permethrin cream 5% for twice with one week interval for all cases of Norwegian and Classic scabies; 4) retaining isolation patients for 8 days and prevention of relapse of the disease for 72 hours after completing second treatment for the diagnosis of scabies [23].
Most of the published reports were including spread of scabies between nurses and patients admitted to infectious diseases, students of a school, in prisons and nursing home [5,23-25]. In this study, due to the timely action of the early warning system, the spread of disease to other units was prevented and the contamination of scabies was limited to one unit by implementing the method of isolating patients and the timely separation of clothing from infected people, the disease epidemic ended after two months.
This article presented a patient with a rare case of scabies, Norwegian scabies. Elderly debilitated and immunocompromised patients are exposed to the risk of more severe forms of scabies. The same mite causing more classic presentation of the scabies skin infestation is also present in Norwegian scabies; in this case, declined immune response of the host was probably the reason for more severe symptoms. Absence of itching indicates lack of proper immune response [7].
In an overview of the published institutional scabies outbreaks by Stoevesandt J et al., 55 outbreak of scabies were reviewed, out of which three report were in institution for the disabled [26].
One of the criticisms about the persons of unit E was, their clothes were washed in the same washing machine with mild water daily and then they were dehydrated in drying machine but they were not subjected to sun light. The other mistake about this unit was that they had one towel which was used by three persons, unlike the study by Raza N et al., which found that sharing of towels or clothes was not a risk factor for scabies, whereas sharing of beds was [27,28].
The washing method of the disabled patients was one of the recommended strategies, in a way that the clothes of persons of the unit E were boiled separately at first then they should be washed by washing machine and after drying with drying system, they should be subjected to sunlight for 24 hours. The clothes of other units with no case of disease, though were washed with each other but it was recommended to boil the clothes until complete cure of the patients and till the end of their treatment periods.
Washing machine was disinfected daily with sodium hypochlorite 1%. For the case of classic type, it was set to prepare one towel for each person entitled with their own names and for doing personal cleaning, the nurses of each unit should change their gloves. All surfaces, walls and fences which are special for the disable persons were disinfected with 10% sodium hypochlorite twice daily. The classic visits of the unit’s residents were limited.
In the units with scabies infection, the patients were isolated until complete treatment. About the classic bedspread and pillow cases of the nurses, it was suggested each nurse to use his own personal sleeping supplies [29]. The uniform of all service personnel were washed twice in one week and they were replaced with the clean uniform. Two pregnant service personnel were treated with 10% sulfur ointment instead of 10% crotamiton and their contacts with the patients of other units were banned. All the patients’ were treated, with 5% permethrin cream twice, with one week interval and in order to reduce the itching; 5 mg prednisolone was prescribed to the mental patients (having scabies) daily for one week. The 16.02% initial prevalence rate of scabies were detected in this study compared with Fiji (18.5%), Vanuatu (24%), the Solomon Islands (25%), Timor-Leste (17.5%) and Malaysia (31%) [30-33].
In terms of control measures for the nosocomial setting, efforts have been mainly focused on staff training and conduction of mass treatment management suggested by various guidelines based on the regional regulations protocol. Recommendation of permethrin 5% topical treatment indicates high efficacy of permethrin and its rare adverse effects in comparison with other topical treatments and oral ivermectin. No adverse effects were recorded in patients treated in our study [34].
In a scabies outbreak (Leppard B et al.,), that happened in a prison in Tanzania, many prisoners were infected within four weeks. To cure these persons, 66 liters of Benzyl Benzoate were needed but it was too costly. Even application of lindane lotion and permethrin cream were more costly. The alternative drug was ivermectin. In this outbreak, actellic insecticide with 80 mg amount in 20 liters of water was sprayed on the floor and the walls of the rooms, where the patients were living [19].
Arlian LG et al., explanted that away from their hosts, mites are able to survive and remain infective for 24-36 hours at 21°C and 40-80 % relative humidity. Therefore, according to this theory, we did not use insecticides in our study [35]. In a study of Leppard B et al., the personnel of the prison were cured with 1% lindane but in our study, 10% crotamiton cream was applied. The age group of the patients was between 20 to 30-year-old and they were males which were in accordance with our study. An 88% of the prisoners were treated with ivermectin within four weeks but in our study, 95% of the patients were treated with 5% permethrin cream [19].
Andersen BM et al., explained a scabies outbreak that occurred in five months (October 1998–February 1999) influencing 19 people related to a nursing home in Oslo. Thirteen patients were diagnosed with scabies including six long-term patients and five short-term patients who were treated at home [5]. Chosidow O described an outbreak in an HIV-positive patient with crusted scabies led to development of scabies symptoms in 14 out of 19 staff. A total of 32 patients out of 33 patients of a closed nursing home were diagnosed with scabies, and some of them had crusted scabies. Long-term failures by repeated treatments of permethrin, gamma-benzene hexachloride, benzyl benzoate etc., resulted in application of oral treatment with ivermectin (an anti-parasitic drug) which showed effectiveness [12].
In a literature analysis of 44 scabies epidemics over the years 1976-1996, the authors found six factors that contributed to transmission and recurrent scabies in healthcare institutions: a) among residents in health care institutions a considerable number are, once infested, at risk of developing crusted scabies; b) many people are exposed through close contact; c) the generally long diagnostic delay; d) insufficient survey of the epidemiological problem; e) treatment failures; and f) incomplete post-intervention monitoring [36].
Limitation
According to the patient’s physical and mental disabilities that were aggressive, we could not collect skin scrapings scabies of all patients. Due to the lack of funds at the centre, common supplies were used for the care of the people, which caused an outbreak. Another was the lack of required service personnel, which made it difficult to take care of the patients.
Conclusion
According to the findings, the delay in treatment and reported case scabies in a child with Down syndrome led to the epidemics among the disabled persons. So, it can be inferred that there is an urgent need in social places, including hospitals, centres for the care of the elderly and mentally handicapped people, the nurses and service personnel to get trained about the importance of urgent report of epidemic diseases especially scabies to Health care centres and it is too necessary to isolate the infected persons with scabies and to avoid their touch with healthy persons until their complete recovery.
W2: Second week; W3: The third week
[1]. Golant AK, Levitt JO, Scabies: a review of diagnosis and management based on mite biologyPediatr Rev 2012 33(1):e1-2.10.1542/pir.33-1-e122210934 [Google Scholar] [CrossRef] [PubMed]
[2]. Vorou R, Remoudaki HD, Maltezou HC, Nosocomial scabiesJ Hosp Infect 2007 65(1):9-14.10.1016/j.jhin.2006.08.01217141368 [Google Scholar] [CrossRef] [PubMed]
[3]. Chosidow O, Scabies and pediculosisThe Lancet 2000 355(9206):819-26.10.1016/S0140-6736(99)09458-1 [Google Scholar] [CrossRef]
[4]. Devaraju B, Study of efficacy of invermectin in comparison to classicly used topical antiscabetic drugs (Doctoral dissertation, RGUHS) [Google Scholar]
[5]. Andersen BM, Haugen H, Rasch M, Haugen AH, Tageson A, Outbreak of scabies in Norwegian nursing homes and home care patients: control and preventionJ Hosp Infect 2000 45(2):160-64.10.1053/jhin.1999.071610860693 [Google Scholar] [CrossRef] [PubMed]
[6]. Carslaw Rw, Dobson Rm, Hood AJ, Taylor RN, Mites in the environment of cases of Norwegian scabiesBr J Dermatol 1975 92(3):333-37.10.1111/j.1365-2133.1975.tb03084.x807230 [Google Scholar] [CrossRef] [PubMed]
[7]. Georgiev VS, Infectious diseases in immunocompromised hosts 1997 CRC Press:29 [Google Scholar]
[8]. Hengge UR, Currie BJ, Jäger G, Lupi O, Schwartz RA, Scabies: a ubiquitous neglected skin diseaseLancet Infect Dis 2006 6(12):769-79.10.1016/S1473-3099(06)70654-5 [Google Scholar] [CrossRef]
[9]. Makigami K, Ohtaki N, Ishii N, Yasumura S, Risk factors of scabies in psychiatric and long-term care hospitals: A nationwide mail-in survey in JapanJ Dermatol 2009 36(9):491-98.10.1111/j.1346-8138.2009.00691.x19712276 [Google Scholar] [CrossRef] [PubMed]
[10]. Walton SF, Myerscough MR, Currie BJ, Studies in vitro on the relative efficacy of current acaricides for Sarcoptes scabiei var. hominisTrans R Soc Trop Med Hyg 2000 94:92-96.10.1016/S0035-9203(00)90454-1 [Google Scholar] [CrossRef]
[11]. Currie BJ, McCarthy JS, Permethrin and ivermectin for scabiesN Engl J Med 2010 362(8):717-25.10.1056/NEJMct091032920181973 [Google Scholar] [CrossRef] [PubMed]
[12]. Chosidow O, ScabiesN Engl J Med 2006 354:1718-27.10.1056/NEJMcp05278416625010 [Google Scholar] [CrossRef] [PubMed]
[13]. Scheinfeld N, Controlling scabies in institutional settings: a review of medications, treatment models, and implementationAm J Clin Dermatol 2004 5:31-37.10.2165/00128071-200405010-0000514979741 [Google Scholar] [CrossRef] [PubMed]
[14]. Strong M, Johnstone PW, Interventions for treating scabiesCochrane Database Syst Rev 2007 3:CD00032010.1002/14651858.CD000320.pub217636630 [Google Scholar] [CrossRef] [PubMed]
[15]. Monsel G, Chosidow O, Management of scabiesSkin Therapy Lett 2012 17(3):01-04. [Google Scholar]
[16]. Stamm LV, Strowd LC, Ignoring the “itch”: the global health problem of scabiesAm J Trop Med Hyg 2017 97(6):1647-49.10.4269/ajtmh.17-024229016295 [Google Scholar] [CrossRef] [PubMed]
[17]. Geary TG, Ivermectin 20 years on: maturation of a wonder drugTrends Parasitol 2005 21:530-32.10.1016/j.pt.2005.08.01416126457 [Google Scholar] [CrossRef] [PubMed]
[18]. Obasanjo OO, Wu P, Conlon M, Karanfil LV, Pryor P, Moler G, An Outbreak of Scabies in a Teaching Hospital Lessons Learned. InfectControl Hosp Epidemiol 2001 22(1):13-18.10.1086/50181811198016 [Google Scholar] [CrossRef] [PubMed]
[19]. Leppard B, Naburi AE, The use of ivermectin in controlling an outbreak of scabies in a prisonBr J Dermatol 2000 143(3):520-23.10.1111/j.1365-2133.2000.03704.x10971323 [Google Scholar] [CrossRef] [PubMed]
[20]. Hernandez-Perez E, Resistance to antiscabietic drugsJ am Acad Dermatol 1983 8:121-23.10.1016/S0190-9622(83)80285-0 [Google Scholar] [CrossRef]
[21]. Taplin D, Meinking TL, Porcelain SL, Castillero PM, Chen JA, Permethrin 5% dermal cream: a new treatment for scabiesJ Am Acad Dermatol 1986 15(5 Pt 1):995-1001.10.1016/S0190-9622(86)70263-6 [Google Scholar] [CrossRef]
[22]. Roth WI, Scabies resistant to lindane 1% lotion and crotamiton 10% cream [Letter]J Am Acad Dermatol 1991 24:502-03.10.1016/S0190-9622(08)80078-3 [Google Scholar] [CrossRef]
[23]. International classification of impairments, disabilities and handicaps: a manual of classification relating to the consequences of disease. Geneva, World Health Organization, 1980 [Google Scholar]
[24]. World Health Organization. Classification internationale des handicaps: dé ficiences, incapacités, désavantages-manuel de classification des consé quences des maladies. Paris, Institut national de la Santéet de la Recherche médicale and Centre technique national d’Education et de Réadaptation des Handicapéset Inadaptés, 1988 [Google Scholar]
[25]. Ejidokun OO, Aruna OS, O’neill B, A scabies outbreak in a further education college in GloucestershireEpidemiol Infect 2007 135(3):455-57.10.1017/S095026880600707216948878 [Google Scholar] [CrossRef] [PubMed]
[26]. Stoevesandt J, Carlé L, Leverkus M, Hamm H, Control of large institutional scabies outbreaksJDDG: J Dtsch Dermatol Ges 2012 10(9):637-47.10.1111/j.1610-0387.2012.07892.x22458610 [Google Scholar] [CrossRef] [PubMed]
[27]. Barbotte E, Guillemin F, Chau N, Prevalence of impairments, disabilities, handicaps and quality of life in the general population: a review of recent literatureBulletin of the World Health Organization 2001 79:1047-55. [Google Scholar]
[28]. Raza N, Qadir SN, Agha H, Risk factors for scabies among male soldiers in Pakistan: case-control studyEast Mediterr Health J 2009 15(5):1105-10. [Google Scholar]
[29]. Gulati PV, Singh KP, Braganza C, Role of sociocultural and environmental factors in the cause of scabiesInt J Dermatol 1977 16(4):281-83.10.1111/j.1365-4362.1977.tb04321.x863573 [Google Scholar] [CrossRef] [PubMed]
[30]. Carapetis JR, Connors C, Yarmirr D, Krause V, Currie BJ, Success of a scabies control program in an Australian aboriginal communityPediatr Infect Dis J 1997 16:494-99.10.1097/00006454-199705000-000089154544 [Google Scholar] [CrossRef] [PubMed]
[31]. Currie BJ, Connors CM, Krause VL, Scabies programs in aboriginal communitiesMed J Aust 1994 161:636-37.10.5694/j.1326-5377.1994.tb127655.x [Google Scholar] [CrossRef]
[32]. Dos Santos MM, Amaral S, Harmen SP, Joseph HM, Fernandes JL, Counahan ML, The prevalence of common skin infections in four districts in Timor-Leste: a cross sectional surveyBMC Infect Dis 2010 10:61-66.10.1186/1471-2334-10-6120219136 [Google Scholar] [CrossRef] [PubMed]
[33]. Muhammad Zayyid M, Saidatul Saadah R, Adil AR, Rohela M, Jamaiah I, Prevalence of scabies and head lice among children in a welfare home in Pulau Pinang, MalaysiaTrop Biomed 2010 27:442-46. [Google Scholar]
[34]. Marotta M, Toni F, Dallolio L, Toni G, Management of a family outbreak of scabies with high risk of spread to other community and hospital facilitiesAm J Infect Control 2018 10.1016/j.ajic.2017.12.00429397231 [Google Scholar] [CrossRef] [PubMed]
[35]. Arlian LG, Biology, host relations, and epidemiology of Sarcoptes scabieiAnnu Rev Entomol 1989 34:139-61.10.1146/annurev.en.34.010189.0010352494934 [Google Scholar] [CrossRef] [PubMed]
[36]. Samsom M, Causes of spread and return of scabies in health care institutes; literature analysis of 44 epidemicsNederlands Tijdschrift Voor Geneeskunde 1998 142(7):354-57. [Google Scholar]