A Rare Case of Paranasal Sinus Schwannoma with Intracranial Extension
Mihir Mohan Vaidya1, Asha Sharad Shenoy2, Naina Atul Goel3
1 Fellow, Department of Neuropathology, Seth GSMC and KEM Hospital, Mumbai, Maharashtra, India.
2 Professor, Department of Pathology, Seth GSMC and KEM Hospital, Mumbai, Maharashtra, India.
3 Associate Professor, Department of Pathology, Seth GSMC and KEM Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Asha Sharad Shenoy, 301, Arihant, 613-B, 15th Road, Khar, Mumbai-400052, Maharashtra, India.
E-mail: shenoyasha@yahoo.co.in
Paranasal sinus schwannomas are uncommon and account for less than 4% of head and neck schwannomas. Intracranial extension and aggressive behaviour are very rarely observed in these tumours leading to misdiagnosis of a malignant neoplasm. Here, we report a case of a 35-year-old male with complaint of proptosis. MRI showed a tumour in the region of ethmoid sinus with expansion into anterior cranial fossa. Microscopy revealed a biphasic tumour with compact and loose areas. Tumour was composed of spindle cells with wavy nuclei, showing focal palisading and a strong immunoreactivity for S100. MIB-1 index was around 1%. A diagnosis of Schwannoma was favoured based on histology and immunohistochemistry.
S100, Antoni A, Antoni B, Middle cranial fossa
Case Report
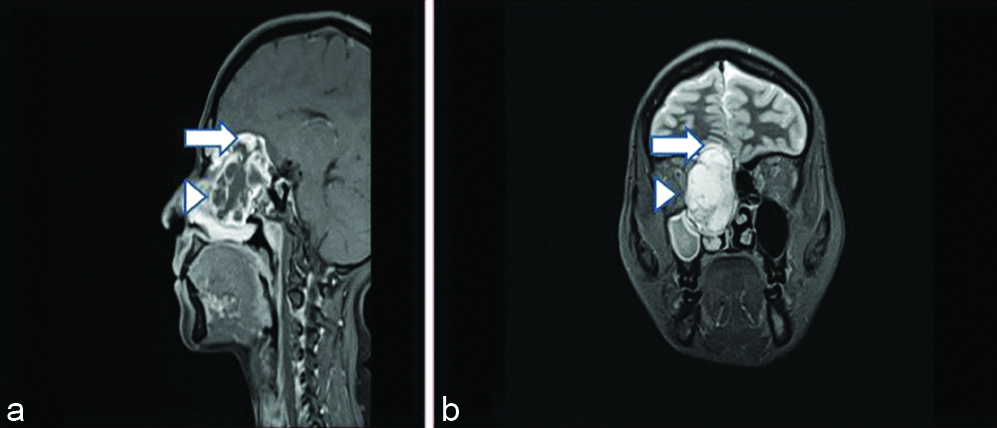
A 35-year-old male presented with right eye proptosis since one and half months. His general, systemic and rest of neurological examination were within normal limit. Haematological and biochemical tests revealed no abnormality. MRI brain+PNS taken in sagittal and coronal planes revealed a 51×28×28 mm mass in the region of right ethmoid sinus, expanding into anterior cranial fossa and causing erosion of skull base [Table/Fig-1]. Radiologically, the possibility of a malignant tumour was considered. Excisional biopsy was performed. Intraoperatively, mass was soft and vascular in nature, which was received in multiple small bits and fragments. Grossly many congested and haemorrhagic areas were seen and few bits had a glistening appearance.
Magnetic Resonance Imaging (MRI) demonstrating the extent of the paranasal sinus mass in the region of ethmoid sinus (arrowhead) with expansion into anterior cranial fossa (arrow); (a) MRI-brain + PNS, T1W-post contrast-sagittal (b) MRI-brain+PNS, T2W Coronal.
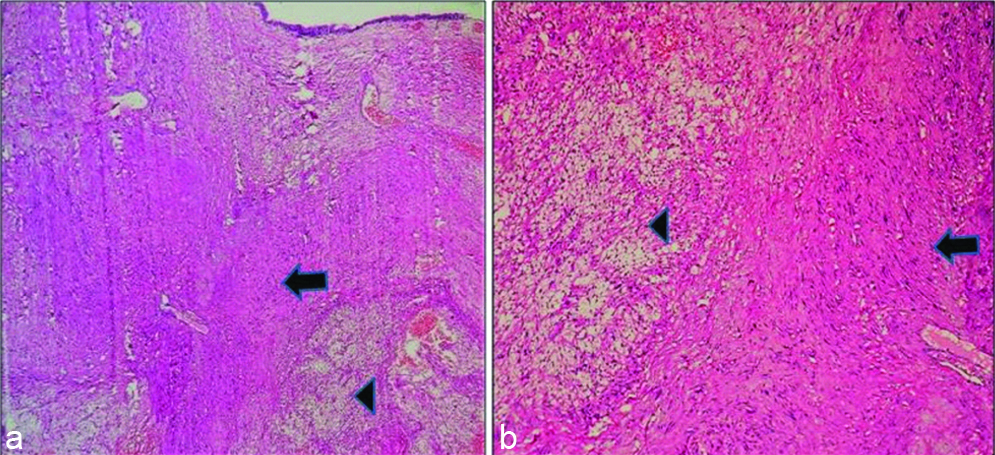
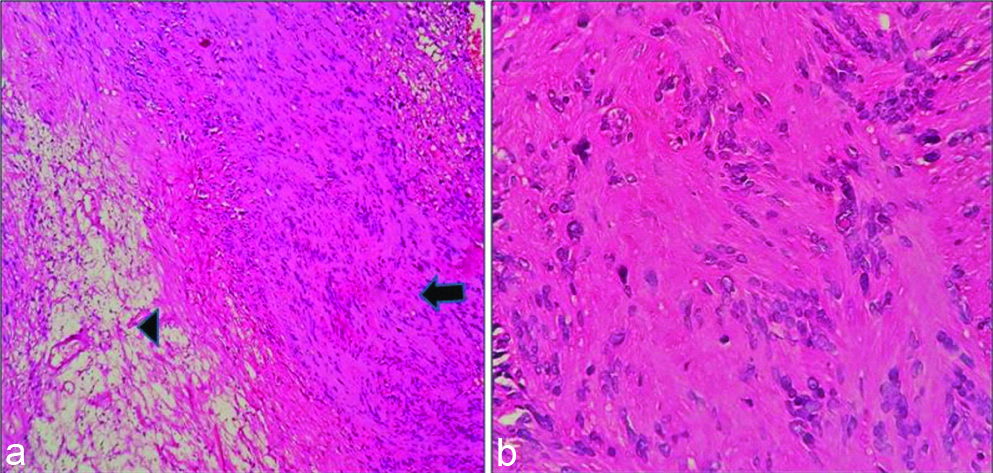
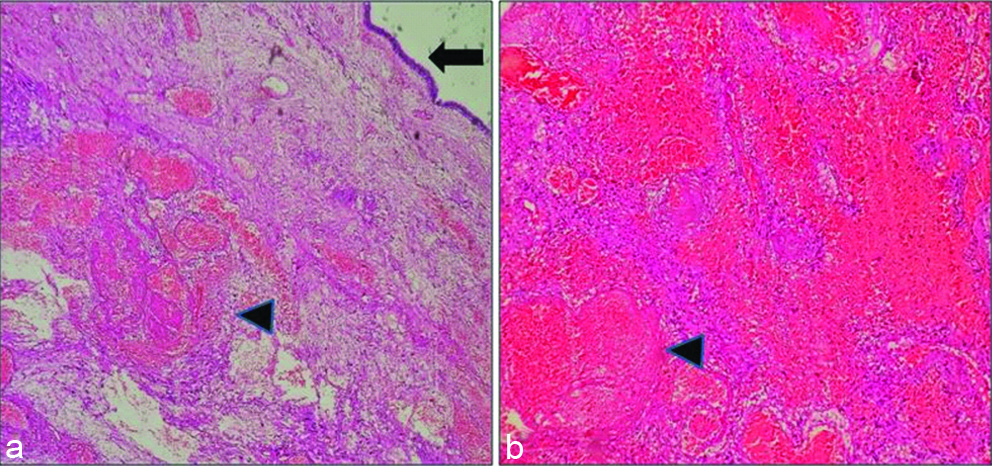
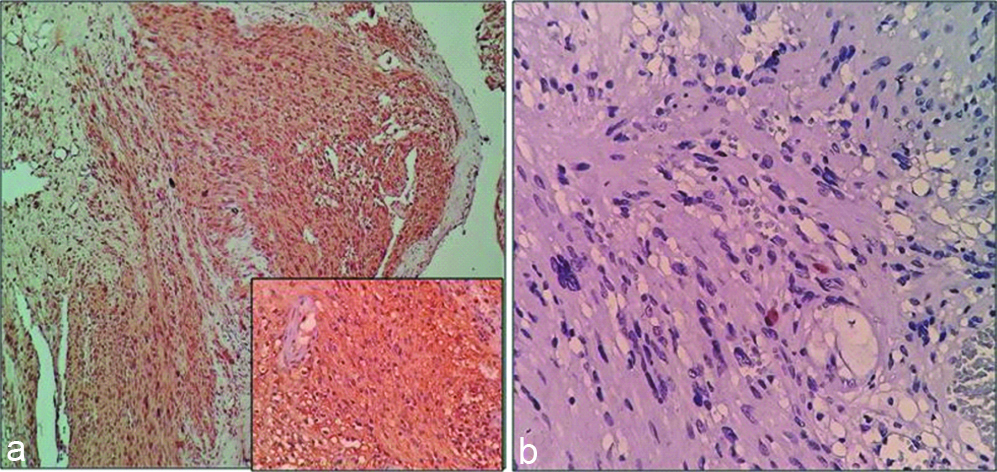
On microscopic examination, multiple biopsy bits showed fragments lined by ciliated columnar type of epithelium of ethmoid sinus. In the subepithelial region, an unencapsulated tumour was seen composed of compact and loose areas [Table/Fig-2]. Compact Antoni A areas showed spindle cells with wavy nuclei, arranged in fascicles. Nuclear palisading was noted at places, however no well-formed Verocay bodies were seen [Table/Fig-3]. Few cells with pleomorphic and bizarre nuclei were also seen. Loose Antoni B areas showed haemorrhage, vessels with hyalinised walls and many large angiectatic blood vessels, some of which showed recent thrombi [Table/Fig-4]. Mitotic activity was not significant and there were no areas of necrosis.
(a) Sinus mucosa with underlying tumor. Even on scanner view, compact (arrow) and loose (arrowhead) areas are identifiable (H&E,4X). (b) Biphasic nature of the tumour with compact Antoni A (arrow) and loose Antoni B (arrowhead) areas (H&E10X).
(a) Adjacent Antoni A (arrow) and Antoni B (arrowhead) areas (H&E,10X). (b) Antoni A areas composed of fascicles of tumour cells showing palisading at places. However, no well-defined verocay bodies seen (H&E,40X).
Aggregates of blood filled ectatic vascular spaces, some of which show recent thrombi (arrowhead). Overlying sinus mucosa is also seen in a. (arrow) (H&E,a-4X,b-10X)
The morphology was strongly suggestive of Schwannoma, however, a differential diagnosis of Pleomorphic Hyalinizing Angiectatic Tumour was considered as it can be a close mimicker of Schwannoma and the fact that the tumour in the present case lacked a capsule and showed a few ectatic blood filled spaces.
On immunohistochemistry, tumour showed strong positivity for S100. Thus, considering the histomorphological features and S100 positivity, a diagnosis of Schwannoma was favoured. Ki-67 labelling index (MIB-1 was the antibody used to determine Ki-67 labelling index) was approximately 1% which confirmed the benign nature of the tumour [Table/Fig-5].
(a-10X, Inset-40X, b-40X) (a) Tumor showing strong immunoreactivity for S100. (b) MIB-1 index was low (approximately 1%).
Discussion
Schwannomas are benign nerve sheath tumours that can be encountered at any age. Peak incidence is 4th to 6th decade. No sex predilection is noted [1]. Paranasal sinus schwannomas follow this overall epidemiological trend with one case series by Kim YS et al., reporting a wide age range of 14 to 79 years [2], while another one by Hasegawa SL et al., reporting it to be 38 to 65 years with no particular sex predilection [3]. Present case was a 35-year-old male.
Common locations of schwannoma are the flex or surfaces of the extremities, neck, mediastinum, retroperitoneum, posterior spinal roots, and cerebellopontine angle [4].
Head and neck schwannomas are common, accounting for 25-45% of schwannoma cases, however, only 4% of head and neck schwannomas are reported to arise in sinonasal cavity [2,5,6]. Majority of sinonasal tumours are epithelial in origin and most of the soft tissue tumours which are encountered in that site are vascular or fibrohistiocytic. Neural tumours are only rarely encountered in paranasal sinuses. Paranasal sinus schwannomas are exceedingly rare and just over 100 cases were reported until 2016 [7].
Among the paranasal sinus tumours, ethmoid sinus is reported to be the most common location, followed by the maxillary sinus and sphenoid sinus [8,9]. In the present case, tumour was located in the region of right ethmoid sinus.
The symptoms are often related to chronic nasal obstruction for e.g., rhinorrhoea, epistaxis, anosmia, and facial swelling etc., [10]. The sole complaint in the present case was right eye proptosis which is described as a symptom of paranasal sinus schwannomas by Wong E et al., and Singh M et al., [11,12].
On MRI scan, the tumour appeared to behave aggressively with erosion of skull base and expansion into anterior cranial fossa leading to the suspicion of a malignant tumour. While bone erosion can be a relatively common occurrence in the setting of schwannoma, particularly cellular schwannoma, intracranial extension is a rare feature with very few reported cases [13-15].
These features coupled with microscopic features of lack of encapsulation and occasional pleomorphic and bizarre cells can pose a diagnostic challenge and an erroneous diagnosis of a malignant lesion can be given [3,7]. The present case lacked a capsule but otherwise showed classic morphology of schwannoma. Pleomorphic Hyalinizing Angiectatic Tumour was considered as one of the differential diagnosis due to the presence of angiectaticvessles. Definite diagnosis was rendered when tumour cells showed strong positivity for S100. Pleomorphic Hyalinizing Angiectatic Tumour lacks expression of S100 which is a useful marker to differentiate the two entities [16]. Angiectatic vessels have been described in schwannoma [17]. No microscopic features of malignancy such as increased mitotic activity and necrosis were noted. A low MIB-1 index of around 1% confirmed its benign nature. Buob D et al., have reported MIB-1 index of 1-5% for sinonasal schwannoma [10]. While, majority of schwannomas are capsulated, it’s important to note that visceral and mucosal (such as sinus) schwannomas can lack a capsule [3,10,18].
Conclusion
While paranasal sinuses are a rare location for nerve sheath tumours, schwannomas can be encountered there and they should be considered as differential diagnosis of soft tissue lesions at this site. Lack of encapsulation, bone erosion and intracranial extension can be observed in schwannomas and do not necessarily indicate malignant behaviour.
[1]. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, WHO Classification of Tumours of the Central Nervous System 2016 Revised 4th edLyonIARC [Google Scholar]
[2]. Kim YS, Kim HJ, Kim CH, Kim J, CT and MR imaging findings of sinonasal schwannoma: A review of 12 casesAm J Neuroradiol 2013 34(3):628-33.10.3174/ajnr.A325722954739 [Google Scholar] [CrossRef] [PubMed]
[3]. Hasegawa SL, Mentzel T, Fletcher CD, Schwannomas of the sinonasal tract and nasopharynxMod Pathol 1997 10:777-84. [Google Scholar]
[4]. Rodrigues G, Rao A, Digital neurilemmoma: A case reportBahrain Med Bull 2002 24(2):76-77. [Google Scholar]
[5]. Dhawle MS, Rathod SG, Bhatkule MA, Bindu RS, Sinonasal schwannoma- A case reportJ Clin Diagn Res 2017 11(5):ED22-ED23.10.7860/JCDR/2017/21532.985128658783 [Google Scholar] [CrossRef] [PubMed]
[6]. Mangubat EZ, Pitelka L, Petruzzelli GJ, Byrne RW, Frontal sinus schwannoma: Case report and review of literatureSkull Base Rep 2011 1:17-22.10.1055/s-0031-127524623984197 [Google Scholar] [CrossRef] [PubMed]
[7]. Gencarelli J, Rourke R, Ross T, Gravel D, Purgina B, Jordan D, Atypical presentation of sinonasal cellular schwannoma: A nonsolitary mass with osseous, orbital, and intracranial invasionJournal of Neurological Surgery Reports 2014 75(01):e144-48.10.1055/s-0034-137642425083375 [Google Scholar] [CrossRef] [PubMed]
[8]. Berlucchi M, Piazza C, Blanzuoli L, Battaglia G, Nicolai P, Schwannoma of the nasal septum: A case report with review of the literatureEur Arch Otorhinolaryngol 2000 257:402-05.10.1007/s00405000024211052256 [Google Scholar] [CrossRef] [PubMed]
[9]. Batsakis J, Tumours of the head and neckClinical and pathological considerations 1979 2nd edBaltimoreWilliams and Wilkins:313-33. [Google Scholar]
[10]. Buob D, Wacrenier A, Chevalier D, Aubert S, Quinchon JF, Gosselin B, Schwannoma of the sinonasal tract: A clinicopathologic and immunohistochemical study of 5 casesArchives of Pathology & Laboratory Medicine 2003 127:1196-99. [Google Scholar]
[11]. Wong E, Kong J, Oh L, Cox D, Forer M, Giant primary schwannoma of the left nasal cavity and ethmoid sinusCase Reports in Otolaryngology 2016 :1-3.10.1155/2016/170691527379190 [Google Scholar] [CrossRef] [PubMed]
[12]. Singh M, Bhagat S, Sharma DK, Monga R, Chhabra N, A large sinonasal schwannoma: a rare entityInt J Otorhinolaryngol Head Neck Surg 2017 3:1126-29.10.18203/issn.2454-5929.ijohns20174348 [Google Scholar] [CrossRef]
[13]. Somasekhar , Lakshmi S, Ramya S, Sinonasal schwannoma with secondary changesIndian J Otolaryngol Head Neck Surg 2008 60(3):274-76.10.1007/s12070-008-0092-z23120562 [Google Scholar] [CrossRef] [PubMed]
[14]. Takahashi E, Hull N, Stevens C, Hoxworth J, Weindling S, Wood C, Sinonasal schwannoma: A case report and updated review of the literatureOpen Journal of Medical Imaging 2015 5:66-70.10.4236/ojmi.2015.52010 [Google Scholar] [CrossRef]
[15]. Siqueira Mario G, Jennings E, Moraes Osmar JS, Santos Marco Tulio S, Zanon N, MattosBelmiro J, Naso-ethmoid schwannoma with intracranial extension: Case reportArq Neuro-Psiquiatr. [Internet] 2001 59(2B):421-23.10.1590/S0004-282X200100030002111460191 [Google Scholar] [CrossRef] [PubMed]
[16]. Raghavan V, Shivaprashanth K, Ramesh Rao K, Pleomorphic hyalinising angiectatic tumour: Immunohistochemical study with review of literatureIJSS Case Reports & Reviews 2015 1(8):46-49. [Google Scholar]
[17]. Iwamoto C, Garcia C, Fung C, Pathologic quiz case: A 52-year-old woman with a liver massArch Pathol Lab Med [Internet] 2003 127(5):631-32. [Google Scholar]
[18]. Hegazy HM, Snyderman CH, Fan CY, Kassam AB, Neurilemmomas of the paranasal sinusesAm J Otolaryngol 2001 22(3):215-18.10.1053/ajot.2001.2343411351293 [Google Scholar] [CrossRef] [PubMed]