Rehabilitation of congenital lower limb deficiencies remains a challenge. A four-year-old boy presented with bilateral lower limb deficiency since birth and inability to stand. Orthoprosthesis with modified bucket type socket accommodating the right rudimentary limb, connected by a tubular shank and a modified foot piece on right side was prescribed. The left side of socket was incomplete inferiorly for the limb to pass through. An additional left Ankle Foot Orthosis (AFO) was also prescribed. The child achieved independent standing as well as started taking steps with a rollator.
Foot, Orthosis, Prosthesis, Rudimentary limb, Socket
Case Report
A four-year-old male child was brought by his mother to the Physical Medicine and Rehabilitation Out Patient Department of a Government Hospital in Northern India with deficiency of both lower limbs since birth and inability to stand independently. He was the second born child of a non-consanguinous marriage and has an elder sister who is apparently normal. There was no similar complaint in any of the family members or close relatives. The mother gave history of taking over-the-counter ‘Saridon’ tablets (Paracetamol, Caffeine+Propyphenazone) for headache intermittently during the early months of pregnancy (7-10 tablets per week). Antenatal check-up was inadequate. The boy had normal developmental milestones except for motor milestones involving his lower limbs. He had normal higher mental functions and was able to follow commands. He had achieved independent household mobility by means of bottom shuffling and creeping. He was able to indicate bladder and bowel consistently.
The left lower limb was small with no apparent knee joint [Table/Fig-1]. The right side was rudimentary and 12 cm in length. He had a power of 5 according to Medical Research Council (MRC) scale [1] in the muscles around the hip and ankle joints on the left side. He also had a power of 5 over the rudimentary stump on the right side as per the MRC scale as there was movement against full resistance applied by the examiner. When made to stand on his left lower limb, the hip joint had a tendency to dislocate laterally which was reducible with pressure from the lateral aspect of greater trochanter of femur. Spine and upper limb examination was unremarkable. Sensation was intact throughout. There were no callosities or any other skin lesions. He had good static and dynamic sitting balance.
Small left lower limb with no apparent knee joint and rudimentary right side.

An Antero-Posterior Radiograph of the pelvis with both lower limbs (in lying down position) showed absence of the right femur, tibia, fibula, tarsals, all metatarsals except one and all phalanges except one proximal and distal phalanx; absence of left tibia and fibula with the femur articulating at the ankle [Table/Fig-2].
Antero-Posterior radiograph of the pelvis with both lower limbs (in lying down position).

The following diagnosis was made: Congenital Bilateral Lower Limb Deficiency with Right-Longitudinal, Femur total, Tibia total, Fibula total, Tarsus total, Ray 2,3,4,5 total; Left-Longitudinal, Tibia total, Fibula total as per The International Society for Prosthetics and Orthotics (ISPO) Classification System [2]. ‘Femur total’ denotes a total absence of the femur; ‘Tibia total’ denotes a total absence of the tibia; ‘Fibula total’ denotes a total absence of the fibula and ‘Tarsus total’ denotes total absence of tarsal bones. Ray 2, 3, 4, 5 Total implies that the 2nd, 3rd, 4th and the 5th metatarsals and their corresponding phalanges are totally absent. Despite the fact that the most common cause of congenital limb deficiencies is idiopathic, the child was evaluated for secondary causes such as chromosomal aberrations, amniotic band syndrome, Fanconi anaemia, Poland sequence, Vascular Disruptions among others in consultation with the Department of Paediatrics and Genetics but was not conclusive of any definite syndrome. No deformity was detected in organ systems such as the Cardiac, Respiratory, Gastrointestinal and the Central Nervous System.
Taking into consideration the mother’s felt need of achieving independent standing, an orthoprosthesis was planned. The mother was counselled about the possibility of amputation of the right rudimentary stump for which she did not consent. She was also counselled about the need for frequent follow-ups and change of the orthoprosthesis. As there was intact sensation and voluntary control, it was decided to accommodate the right rudimentary limb in the orthoprosthesis after mother accepted risk of friction induced skin breakdown. It consisted of a modified bucket type of socket. Enough cut outs were made in the socket for bladder and bowel needs. The socket consisted of a dual structure: a hard frame fabricated using a sheet of Copolymer-Polypropylene of 15 mm thickness and a soft ethaflex inner lining using a sheet of 8 mm thickness. The main feature of the socket was distribution of pressure to prevent pressure ulcers. In addition, the socket had small holes of half an inch diameter for ventilation and weight reduction and a velcro strap for donning. A trochanteric pad made of Low-Density Polyethylene grains covering the left femoral greater trochanter was added to prevent dislocation of the femur. On the right side, a tubular shank was connected to the socket with a press button. The distal aspect of this shank was connected to a modified foot piece. The left side of the socket was incomplete inferiorly for the limb to pass through. An additional left Ankle Foot Orthosis (AFO) was also prescribed [Table/Fig-3,4]. The child not only achieved standing but was able to take steps independently with a rollator [Table/Fig-5]. A twister made of spring connecting the AFO and the Socket using D-rings, was able to correct a mild rotational deformity of the left lower limb present during ambulation. He was given this orthoprosthesis at the very first visit (at the age of 4 years) after completion of fabrication.
Front view of orthoprosthesis.
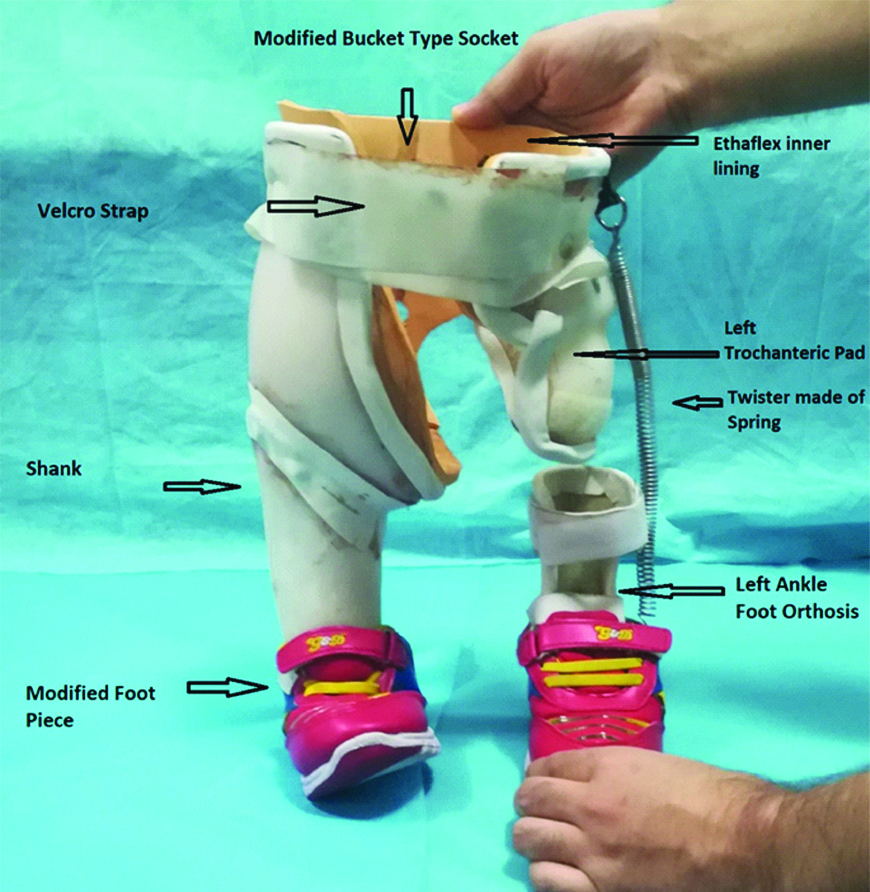
Rear view of orthoprosthesis.

Child propelling a rollator wearing the orthoprosthesis.

The child has been using this as the primary mode of ambulation inside the household as was discerned at the follow-up at three months. The child has been advised to come for the next follow-up at the end of six months from the date of prescription for revision of the orthoprosthesis and possible incorporation of hip joints.
Discussion
Congenital Limb Deficiencies (CLDs) are due to failure in formation or disruption of a part or entire upper or lower limb or digits during foetal development. The prevalence of CLDs is around 5 per 10000 live births [3]. The early “limb bud” consists of a simple ectoderm cover with a mesoderm core that vascularizes with subsequent invasion of somatic mesoderm and nerves. The upper limbs usually develop before the lower limbs. The structure of the limb gets established externally by the end of the embryonic period (8th week of gestation), except for nails and hair [4]. Most of CLDs occur as isolated defects while only 12-33% is found with other major congenital malformations. Preaxial limb defects are frequently associated with microtia, oesophageal atresia, anorectal atresia, heart defects and unilateral kidney dysgenesis. Postaxial defects are usually associated with hypospadias; transverse defects with craniofacial defects, micrognathia, ring constrictions, and muscular defects; intercalary defects with omphalocele; split hand/foot with encephalocele; and amelia with anorectal atresia, omphalocele, severe genitalia defects, unilateral kidney dysgenesis, gastroschisis, and ring constriction [5]. Upper CLDs are more common (58%) and are slightly commoner in males. Amelia, the complete absence of both the upper and lower limbs, occurred at a significantly lower rate (0.2/10,000 births) than upper-limb or lower-limb deficiency; however, rates of amelia among stillbirths was reported to be 30 to 40 times greater than those among live births. Rate of upper-limb deficiency was reported to be 2 to 3 fold than that of lower-limb deficiency in a few studies [6]. The cause is often unknown, but various teratogens (e.g., medications such as thalidomide, misoprostol, phenytoin among others), amniotic band syndrome, chromosomal abnormalities (Trisomy 18, Trisomy 13), VACTERL syndrome, Split hand/foot syndrome, Fanconi anaemia and Holt Oram syndrome have been associated. Smoking and consumption of alcohol have also been implicated in some cases [7-9]. Primary prevention of congenital limb defects is of paramount importance and interventions include nutritional modifications (e.g., Riboflavin and multivitamin supplementation or fortification); prevention of maternal infections and diseases, vaccination (Such as Rubella), peri-conceptional care for women with reconsideration of antiepileptic medications among others, avoidance of teratogenic drugs and lifestyle modifications for factors such as smoking, consumption of cocaine, consumption of alcohol and management of obesity [8-12].
The current and preferred system of describing CLDs is that of the International Society for Prosthetics and Orthotics (ISPO). CLDs are classified into transverse and longitudinal. Transverse implies lack of elements beyond a particular level even though digital buds (nubbins) may exist. Longitudinal indicates reduction (partial) or absence (total) of skeletal elements within the long axis of the limb [13]. This case is difficult to classify according to classical or Revised Frantz and O’Rahilly Classification and such cases were described by many authors as complex before the advent of the ISPO system [14]. Antenatal history revealed only positive history of intake of ‘Saridon’ tablets (Paracetamol, Caffeine, Propyphenazone) during the early months of pregnancy. An exhaustive literature search done by us did not reveal any association of caffeine (Pregnancy category-C) [15], Paracetamol (Pregnancy category-B) [16] or Propyphenazone with teratogenic effects. The co-administration of propyphenazone and caffeine or propyphenazone and paracetamol to sexually mature albino rats resulted in growth retardation, however, no teratogenic effects were observed [17]. Consultation with the Department of Paediatrics and Genetics was not conclusive of any definite syndrome. Other organ systems were also found to be normal.
The orthoprosthesis was made in the prosthetic and orthotic workshop attached with the Department of Physical Medicine and Rehabilitation in our hospital in a stepwise approach. Measurements were taken and this was followed by casting. Subsequently, pouring of Plaster of Paris and modification of the negative mould was done. This was followed by fabrication of the socket and the AFO. A shank along with an adjustable rod inside and a modified foot piece were subsequently made. A modified bucket type of socket was designed with an emphasis on accurate negative mould to incorporate the rudimentary right lower limb to minimise the possibility of pressure or friction injuries. Trimlines of the socket extended superior to the iliac crest. The socket on the right side was attached by a hollow shank to a 3 mm thick modified foot piece. The height of the orthoprosthesis was determined based on the length of relatively better left lower limb as measured from the perineum to the floor. A rod inside the hollow shank was used to determine precise height of the right side of orthoprosthesis to achieve a balanced upright posture in order to compensate for any possible limb length discrepancy. This rod was moved in a telescopic manner until the correct height was achieved and eventually fixed to the shank via screws. The trimline of the AFO was 19 mm below the head of the fibula, anterior to the malleolus and up to the toes. The child faced two problems on initial fitment of the orthoprosthesis. The first problem was lateral displacement of left femoral head as evident by palpable laterally displaced greater trochanter on weight bearing. The use of trochanteric girdle prevents lateral hip displacement by exerting a medially directed force on the greater trochanter during weight-bearing [18] and, therefore a trochanteric girdle was made. The trimlines of the trochanteric girdle extended from one and a half inch above the greater trochanter and inferiorly up to the mid-thigh. Secondly, there was a mild rotational deformity of the left lower limb. A twister made of spring was made and attached from the socket to the AFO to correct for the mild rotational deformation of the left lower limb. Twisters attached to AFO have been used successfully in the past to correct for rotational deformities and the same principle was used here [19]. A pre-tensioned twister attached with AFO provides a torque which acts to keep the foot forward during walking [20]. The patient subsequently received gait training. This was followed by final fitment of the prosthesis. Rehabilitation plan for congenital amputees requires a unique approach for each case. There has been no case described in literature wherein an orthoprosthesis of this type was used. The primary goal was to achieve standing and the goal was met with this custom made orthoprosthesis as the child has been using this as the primary mode of ambulation inside the household as was discerned at the follow-up at three months. The child has been advised to come for the next follow-up at the end of six months from the date of prescription for revision of orthoprosthesis and possible incorporation of hip joints. There has been no difficulty in walking with the prosthesis. The child has accepted the prosthesis well. We plan to incorporate the hip joint at a later date as it is likely to improve the gait pattern.
Conclusion
There is no single prescription for CLD. It has to be customised from child to child. Contrary to adult prosthetic prescription, children undergo major growth changes and require more frequent follow-ups and prosthetic changes. There is little body image adjustment for the child himself born with limb deficiency, however, the same is not true for his parents and other family members for whom support is required. Some of these children with CLDs may require amputation and for them, the issue of adjustment needs to be looked into. The management of paediatric limb deficiency requires an anticipatory outlook as the child will go through many development stages and various needs to be taken into account especially with respect to age, growth spurts, terminal overgrowth, leg length discrepancies, body image and guidance for the family.
[1]. John J, Grading of muscle power: Comparison of MRC and analogue scales by physiotherapists. Medical Research CouncilInt J Rehabil Res 1984 7(2):173-81.10.1097/00004356-198406000-000056490272 [Google Scholar] [CrossRef] [PubMed]
[2]. Day HJ, The ISO/ISPO classification of congenital limb deficiencyProsthet Orthot Int 1991 15(2):67-69. [Google Scholar]
[3]. Källén B, Rahmani TM, Winberg J, Infants with congenital limb reduction registered in the Swedish Register of Congenital MalformationsTeratology 1984 29(1):73-85.10.1002/tera.14202901096701808 [Google Scholar] [CrossRef] [PubMed]
[4]. Hill MA, Musculoskeletal System-Limb Development-EmbryologyAvailable from: https://embryology.med.unsw.edu.au/embryology/index.php/Musculoskeletal_System_-_Limb_Development [Accessed 2018 Dec 11] [Google Scholar]
[5]. Rosano A, Botto LD, Olney RS, Khoury MJ, Ritvanen A, Goujard J, Limb defects associated with major congenital anomalies: clinical and epidemiological study from the International Clearinghouse for Birth Defects Monitoring SystemsAm J Med Genet 2000 93(2):110-16.10.1002/1096-8628(20000717)93:2<110::AID-AJMG6>3.0.CO;2-9 [Google Scholar] [CrossRef]
[6]. Ephraim PL, Dillingham TR, Sector M, Pezzin LE, MacKenzie EJ, Epidemiology of limb loss and congenital limb deficiency: A review of the literatureArch Phys Med Rehabil 2003 84(5):747-61.10.1016/S0003-9993(03)04932-8 [Google Scholar] [CrossRef]
[7]. Gold NB, Westgate MN, Holmes LB, Anatomic and etiological classification of congenital limb deficienciesAm J Med Genet A 2011 155A(6):1225-35.10.1002/ajmg.a.3399921557466 [Google Scholar] [CrossRef] [PubMed]
[8]. Czeizel AE, Kodaj I, Lenz W, Smoking during pregnancy and congenital limb deficiencyBMJ 1994 308(6942):1473-76.10.1136/bmj.308.6942.14738019281 [Google Scholar] [CrossRef] [PubMed]
[9]. Froster UG, Baird PA, Maternal factors, medications, and drug exposure in congenital limb reduction defectsEnviron Health Perspect 1993 101(Suppl 3):269-74.10.1289/ehp.93101s32698143629 [Google Scholar] [CrossRef] [PubMed]
[10]. Etemad L, Moshiri M, Moallem SA, Epilepsy drugs and effects on fetal development: Potential mechanismsJ Res Med Sci 2012 17(9):876-81. [Google Scholar]
[11]. Persson M, Cnattingius S, Villamor E, Söderling J, Pasternak B, Stephansson O, Risk of major congenital malformations in relation to maternal overweight and obesity severity: Cohort study of 1.2 million singletonsBMJ 2017 357:j256310.1136/bmj.j256328615173 [Google Scholar] [CrossRef] [PubMed]
[12]. Robitaille J, Carmichael SL, Shaw GM, Olney RS, National Birth Defects Prevention Study. Maternal nutrient intake and risks for transverse and longitudinal limb deficiencies: data from the National Birth Defects Prevention Study, 1997-2003Birth Defects Res A Clin Mol Teratol 2009 85(9):773-79.10.1002/bdra.2058719350655 [Google Scholar] [CrossRef] [PubMed]
[13]. Jain S, Rehabilitation in limb deficiency. 2. The pediatric amputeeArch Phys Med Rehabil 1996 77(3 Suppl):S9-13.10.1016/S0003-9993(96)90237-3 [Google Scholar] [CrossRef]
[14]. Hall CV, Lambert CN, O’Rahilly R, Swinyard CA, Nomenclature for Congenital Skeletal Limb Deficiencies, a Revision of the Frantz and O’Rahilly ClassificationO&P Virtual LibraryAvailable from: http://www.oandplibrary.org/al/1966_01_024.asp [Accessed 2018 Dec 11] [Google Scholar]
[15]. Nikoui V, Ostatdhadi S, Takzare N, Nabavi SM, Giorgi M, Bakhtiarian A, The role of clomipramine in potentiating the teratogenic effects of caffeine in pregnant ratsScientific World Journal 2013 2013:38243410.1155/2013/38243424298213 [Google Scholar] [CrossRef] [PubMed]
[16]. Bulloch MN, Carroll DG, When one drug affects 2 patients: a review of medication for the management of nonlabor-related pain, sedation, infection, and hypertension in the hospitalized pregnant patientJ Pharm Pract 2012 25(3):352-67.10.1177/089719001244207022544624 [Google Scholar] [CrossRef] [PubMed]
[17]. Burdan F, Developmental effects of propyphenazone in analgesic and antipyretic combination with caffeine or paracetamolHum Exp Toxicol 2004 23(5):235-44.10.1191/0960327104ht439oa15222401 [Google Scholar] [CrossRef] [PubMed]
[18]. Ruys EC, Trochanteric Girdle to Prevent Hip Dislocation in Standing: Suggestion from the FieldPhys Ther 1988 68(2):226-27.10.1093/ptj/68.2.2263340662 [Google Scholar] [CrossRef] [PubMed]
[19]. Swaroop VT, Dias L, Orthopedic management of spina bifida. Part I: hip, knee, and rotational deformitiesJ Child Orthop 2009 3(6):441-49.10.1007/s11832-009-0214-519856195 [Google Scholar] [CrossRef] [PubMed]
[20]. Hefti F, Pediatric Orthopedics in Practice 2015 2nd EditionBerlinSpringer10.1007/978-3-662-46810-4 [Google Scholar] [CrossRef]