Spinal Cord Injury (SCI) is a catastrophic event which is sudden and unexpected that can affect the patient’s normal sensory, motor and autonomic function, leading to dependency, morbidity and deterioration in mental health and QOF [1,2]. SCI leads to immense economic burden on the country’s health care system [3,4]. The true impact of SCI can be reflected through the average prevalence rate of 1:1000, and the mean incidence estimated to be between 4-9 cases per 100,000 populations per year, worldwide [5]. It was also reported that the gender ratio in traumatic SCI is 3:1 (men: women), whereas gender is equally distributed in non-traumatic SCI [4]. Management of acute Traumatic Spinal Cord Injury (TSCI) often involves surgery followed by long term rehabilitation to improve functional abilities and QoL [6]. Patients with SCI often experience post-traumatic stress disorder and distress which are associated with decrease compliance with rehabilitation. Prevalence of other co-morbidities such as emotional distress, psychological issues and Post-Traumatic Stress Disorders (PTSD) is very high which makes an adjustment to Activities of Daily Living (ADL) very poor [7].
Evidence shows raised CRP in chronic SCI patients even without the evidence of any concurrent infections, which is an indicator of systemic inflammation and is associated with poor rehabilitation outcome [8]. Increased Body Mass Index (BMI) in SCI is associated with increased risk of Cardio-Vascular Disease (CVD). BMI has been used in earlier studies as a stand-in predictor of risk of obesity in individuals with SCI [9,10]. The therapeutic benefit of medications is often inadequate in the management of neurological and psychiatric disorders [11]. Various other studies have proved that yoga, a form of mind body intervention and Physical Therapy (PT) have enhanced recovery in various neuropsychiatric illnesses [12]. Yoga enhances motor and sensory function, ADL, gait, mental flexibility, psychological well-being and relaxation in individuals with SCI [13-15].
Different yogic techniques incorporated into the rehabilitation protocol of individuals with SCI, with proper guided assistance, is believed to stimulate neural pathways and neurotransmitters [16]. This, in turn, can be valuable instrument in the regeneration of nerve fibres in SCI patients [17]. However, a large number of studies recommended Randomised Controlled Trials (RCTs) to assess the impact of yoga in SCI [13,15,18]. Therefore, authors hypothesised to see the add-on effect of Yoga therapy along with Physiotherapy may improve motor and sensory scores on ASIA scale, QoL, inflammatory markers, distress and functional independence in patients with Spinal Cord Injury, rather than Physiotherapy rehabilitation alone in paraplegic patients.
Materials and Methods
Design
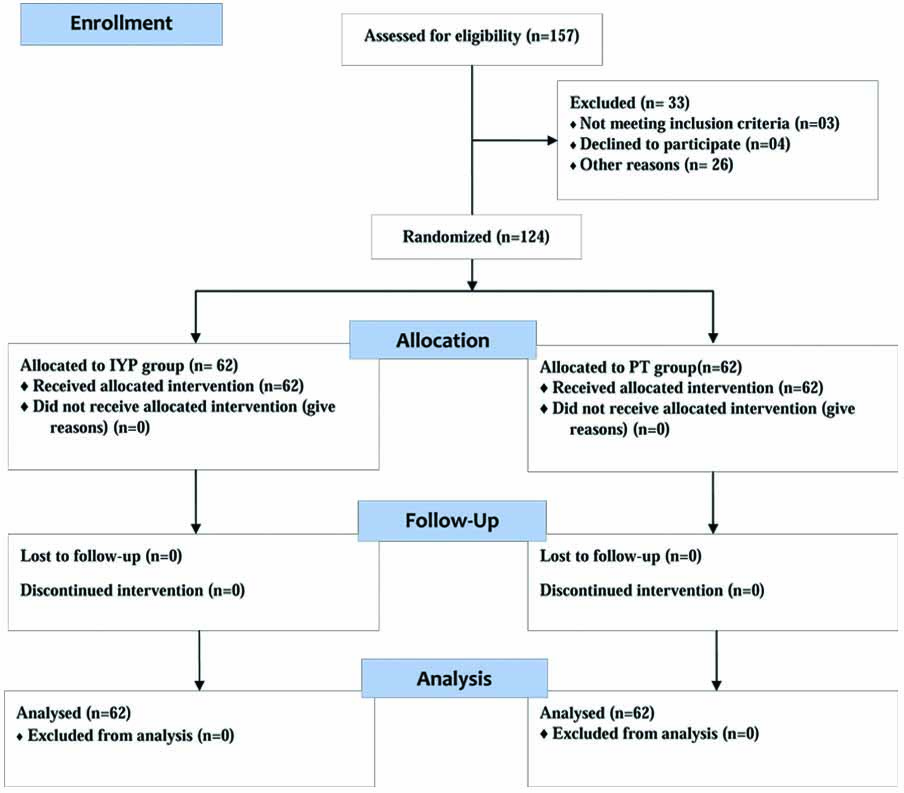
This was a single-blind pre-post randomised controlled trial where all participants were randomly divided into two groups: (i) add-on yoga and physiotherapy group (IYP); and (ii) Physiotherapy Group (PT). Prior to randomisation, each participant was assessed at the baseline.
Participants
A total of 157 SCI patients who were admitted to the Swami Vivekananda National Institute of Rehabilitation, Training and Research (SVNIRTAR), Odisha, India, were screened using ASIA Impairment scale during the period between April 2018 to October 2018. The sample size was calculated using G-power software by fixing the alpha at 0.05 powered at 0.8 and the effect size of 0.55 based on the mean and standard deviation of the SCIM from the previous study [15]. The optimal sample size was 62 participants in each group.
Inclusion Criteria included; being 18-60 years, having incomplete SCI (AIS)-C {motor grade <3 below the neurologic level of injury} and (AIS)-D{a motor grade of at least 3 below the neurologic level of injury} patients of both genders, having sustained a traumatic spinal cord injury for a minimum of six months prior to consent and having completed their primary rehabilitation. Patients were excluded from the study if they: (a) have any contraindications to Faradic Electrical Stimulation (FES) such as a cardiac pacemaker, epilepsy, lower limb fracture or pregnancy; (b) are likely to experience clinically significant autonomic dysreflexia and/or orthostatic hypotension in response to electrical stimulation or prolonged upright postures; (c) have chronic systemic diseases, e.g., Hepatitis-C or HIV-AIDS or have an existing Stage 3 or 4 pressure ulcer; (d) have degenerative myelopathy, neoplasm, congenital spinal cord anomalies or concomitant medical problems that might influence everyday function, such as malignancy, brain injury or mental diseases; and (e) have had recent major trauma or surgery within the last six months. Based on the inclusion/exclusion criteria, 33 participants were excluded. Remaining 124 participants were randomly allocated to the experimental and control group [Table/Fig-1]. Assessments for the male and female participants were done separately.
Ethical Clearance
The study was approved by the Institutional Ethics Committee of University (RES/IEC-SVYASA/93/2016). Signed informed consent was obtained from the head of the institution and each participant, upon explaining the study details. Clinical Trials Registry India (CTRI) Registration Number: CTRI/2018/07/014779.
Randomisation
A Total of 124 participants were assigned in two groups, 62 in each, using computer-based random number generator. One hundred and twenty-four envelopes were prepared, and each participant was asked to pick an envelope. Depending on the number in the envelope, participants were considered either in IYP group or in PT group {known as Sequentially Numbered Opaque Sealed Envelopes (SNOSE) randomisation technique}.
Intervention
Participants in the IYP group received 75 minutes (six days/week) of an integrated yoga intervention for one month. Data collections were done on Day 1 and Day 30. All practices included in the yoga practice protocol were safe, feasible and have been adapted for the intervention with consent from authors of the previous study [19]. An attendance register was maintained to monitor the attendance of the participants. A cut-off of 70% attendance was kept to consider for analysis of data.
Yoga therapy for IYP group: The specific module of yoga therapy for SCI management was developed by using the concepts from traditional yoga scriptures (Patanjali Yoga Sutras, Upanishads and Yoga Vashishtha) that highlight a holistic approach to health management at physical, mental, emotional and intellectual levels. The practices consisted of yogic postures (asanas), breathing practices (pranayama), cleansing techniques (kriya), relaxation techniques, meditation and yogic counselling, chosen specifically for SCI. SCI special techniques progressed from safe yogic movements to yoga postures that provide traction like effect and channelise the vital energy flow all through the spine. The details of yoga therapy practices are given in [Table/Fig-2].
Integrated yoga therapy module for spinal cord injury.
| Type of practice | Practice name (Sanskrit and English) | Duration of practice |
|---|
| Loosening practices/Sukshma Vyayama of Upper limb | Finger movements | Five Minutes. (five rounds each movement) |
| Wrist movements |
| Elbow movements |
| Shoulder movements |
| Loosening practices/Sukshma Vyayama of Lower limb (With or without support) | Toes movements | Five Minutes (five rounds each movement) |
| Ankle movements |
| Knee movements |
| Hip movements |
| Asanas (with support or props) | Padahastasana (hand under foot pose) | Two Minutes (two repetitions) |
| Ardhachakrasana (half-moon pose) | Two Minutes (two repetitions) |
| Ardhakati Chakrasana (half waist rotation pose) | Two Minutes (two repetitions) |
| Vakrasana (half spinal twist pose) | Two Minutes (two repetitions) |
| Kriya | Kapalbhati (high frequency yoga breathing) | Two Minutes (15 rounds) |
| Pranayama | Vibhagiya Pranayama (sectional breathing) | Three Minutes (six rounds) |
| Nadishuddhi (alternate nostril breathing) | Five Minutes (nine rounds) |
| Bhramari (humming sound breathing) | Five Minutes (nine rounds) |
| Bhastrika (rapid ventilation breathing practice) | Two Minutes (six rounds) |
| Relaxation Practice | Deep relaxation technique | 10 Minutes |
| Mind sound resonance technique | 30 Minutes |
For both groups, the Physiotherapy intervention was common and consisted of: (i) Proprioceptive Neuromuscular Facilitation (PNF); (ii) slow and sustained stretching; (iii) prolong icing; (iv) strengthening of anti-gravity muscles; (v) functional electrical stimulation; and (vi) gait training.
Physiotherapy session for both the groups lasted for 60 minutes/day and six days/week for one month.
Assessments
Primary Outcomes
American Spinal Injury Association (ASIA) impairment scale: The ASIA Impairment Scale is an improvisation of the earlier Frankel scale and includes a number of important improvements. The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) was developed by the ASIA as a universal classification tool for SCI, depending upon motor and sensory impairment that results from an SCI. In sensory examination, two aspects of sensation are examined: light touch and pinprick. A grade of 0 denotes absent sensation, 1 denotes impaired or altered sensation and 2 denotes normal sensation. The motor examination consists of testing key muscle functions. Motor strength is recorded for each muscle group bilaterally and is graded using a universal six-point scale (graded as 0-5) where 0 denotes total paralysis and 5 is normal [20].
Bio-marker: C-Reactive Protein (CRP) is a blood test marker for inflammation in the body [21]. Blood samples from the patients were collected early in the morning at 8.00 a.m. for the sake of convenience without any other prior instructions of fasting. The CRP levels <1.0 mg/dL was denoted as negative and CRP levels >1.0 mg/dL was denoted as positive [22].
Spinal Cord Independence Measure (SCIM): Functional recovery may or may not follow/translate into neurologic recovery. SCIM III is a sensitive outcome measure designed to assess functional status relevant to SCI. It can be used as a scale in traumatic and non-traumatic, acute and chronic SCI. There is a total of 19 items on the SCIM III, which are divided into three subscales (self-care, respiration and sphincter management, and mobility). A total score out of 100 is achieved, with the subscales weighted as follows: self-care: scored 0-20; respiration and sphincter management: scored 0-40; and mobility: scored 0-40. Scores are higher in patients that require less assistance or fewer aids to complete basic activities of daily living and life support activities. SCIM III has been validated with excellent internal consistency (Cronbach’s alpha=0.91), excellent inter-rater reliability (r=0.99), and excellent correlation with the Functional Independence Measure (FIM) (r=0.85, p<0.01) [23].
Medical-Based Emotional Distress Scale (MEDS): The MEDS is a 60-item (7 subscales) clinician-administered questionnaire that is completed following a structured interview to assess emotional reactions to severe physical illness or disability that are not the direct result of a physical condition or problem. This instrument measures distress along seven subscales: Dysphoria (8 items), Irritability (9 items), Anhedonia (11 items), Social Withdrawal (9 items), Ruminations over past events (6 items), Cognitive Perspective in the Present (8 items), and Expectations for the future (9 items). Each item provides a question and is followed by a range of responses that are on a 5-point scale for either intensity (how much?) or frequency (how often?). The questions are organised by subscale and the interview is structured such that a denial of problems in a certain area allows the interviewer to skip to the next subscale [24].
Secondary Outcomes
Quality of Life Index Spinal Cord Injury-Version III: The ferrans and powers quality of life index spinal cord injury-version III is an index of 74 items divided into two parts: satisfaction and importance. The Ferrans and Powers Quality of Life (QLI) emerged its specific version for spinal cord injury, known as QLI Spinal Cord Injury - Version III. It was developed by Carol Estwing Ferrans and Powers Marjorie in 1984 [25]. The QLI-SCI was developed to measure quality of life specifically in people with spinal cord injury. It can be administered by interview or by self-report and contains 37 items and each item is rated on a scale of 1 (least satisfied/important) to 6 (most satisfied/important). Five scores of 0-30 (0=less satisfied, 30=most satisfied) are calculated for the following subscales:
Total quality of life score
Health and functioning subscale
Social and economic subscale
Psychological/spiritual subscale
Family Subscale
Calculation of score weighs satisfaction scores according to the level of importance assigned to each item.
Anthropometry: Body Mass Index (BMI), The BMI, or Quetelet index, is a measure of relative weight based on an individual’s mass and height [26]. For measuring the height, the recumbent length of the study participants was measured by making them lie supine on a raised mat table. With the participant’s head in the Frankfort plane, authors placed one metal plate against the top of the participant’s head and the ruler along the right side of the participant’s body. With the right leg aligned with their hip, the other end of the ruler was placed on the distal end of the calcaneus of their right foot. If the participant had spasticity, contractures, or could not lay flat or dorsiflex the ankle to 90°, authors manually assisted them in extending the leg as far as possible or dorsiflexing the ankle. Height was then recorded to the nearest 1/16 of an inch [27]. Total weight was measured using a Wheelchair (WC) platform scale and the participant’s weight was recorded with his/her WC. The participant then transferred out of his/her WC and the WC was weighed alone. Body weight was calculated by subtracting WC weight from the total weight.
Statistical Analysis
Data were analysed using the R-Studio. Shapiro-Francia test was used to check the normality of data distribution. Gender and other categorical variables were analysed using chi-square test. Mc-Nemar test was used to analyse within the group differences in categorical variables. The independent sample t-test was used for between-group analysis and paired samples-test was used for within-group change from pre- to post- at Day 1 and Day 30. Pearson’s correlation was done between age and outcome measured variables. The level of significance considered for the present study was p<0.05.
Results
One-hundred-twenty-four paraplegic patients participated in the study. The mean age of the participants was 33.97±10.0 years and 32.84±9.5 years in IYP and PT group respectively. The number of males and females were almost similar in both the groups. The characteristics and socio-demographic information of study participants are presented in [Table/Fig-3].
Characteristics of the study participants.
| Measurements | Categories | IYP | PT |
|---|
| Age (Mean±SD) | 33.97±10.002 | 32.84±9.465 |
| Gender | Male | 54 | 53 |
| Female | 08 | 09 |
| Languages known | Hindi | 49 (79.03%) | 55 (88.88%) |
| English | 28 (45.16%) | 35 (56.45%) |
| Odiya | 50 (80.64%) | 52 (83.87%) |
| Others | 31 (50%) | 24 (39.36%) |
| Mechanism of injury | Fall from height | 30 (48.19%) | 24 (39.15%) |
| Fall of weight | 06 (9.67%) | 10 (15.52%) |
| Motor vehicle accident | 19 (30.64%) | 24 (38.33%) |
| Miscellaneous | 07 (11.5%) | 04 (07.2%) |
| Educational level | 0-9 years | 09 (14.52%) | 04 (6.45%) |
| 10-12 Years | 48 (77.42%) | 51 (82.26%) |
| >12 Years | 05 (8.06%) | 07 (11.29%) |
| Occupational activity | Employed | 25 (40.32%) | 17 (27.42%) |
| Light physical activity | 18 (29.03%) | 22 (35.48%) |
| Moderate/heavy physical activity | 15 (24.19%) | 21 (33.87%) |
| Unemployed | 4 (6.45%) | 2 (3.23%) |
| Marital status | Married | 35 (56.45%) | 42 (67.74%) |
| Unmarried | 23 (37.09%) | 14 (22.58%) |
| Divorcee | 04 (6.45%) | 06 (9.68%) |
| Neurological level of injury | T2 – T5 | 23 (37.097%) | 25 (40.32%) |
| T6 – T9 | 22 (35.48%) | 20 (32.26%) |
| T10 – L1 | 17 (27.42%) | 17 (27.42%) |
| ASIA impairment scale | C | 45 (72.58%) | 42 (67.74%) |
| D | 17 (27.42%) | 20 (32.26%) |
Within-group Comparisons
At the completion of one month, the difference between BMI, SCI-QOL, SCIM, MEDS, CRP and ASIA impairment score was statistically significant in both the groups however the percentage difference and the change in the number of participants were more in IYP group [Table/Fig-4,5].
Within group comparison of continuous variables of IYP and PT groups.
| Variables | IYP | PT |
|---|
| Pre | Post | % Change | Pre | Post | % Change |
|---|
| BMI | 24.85±3.61 | 24.08±3.26*** | 3.09 | 24.24±3.82 | 23.59±4.32* | 2.67 |
| SCI-QOL | 6.87±2.77 | 9.74±2.75***@ | 41.82 | 7.36±2.72 | 8.43±3.15*** | 14.56 |
| SCIM | 47.69±10.32 | 55.97±11.42*** | 17.35 | 49.27±11.96 | 52.05±12.44*** | 5.64 |
| MEDS | 15.18±5.32 | 11.24±4.47***@@@ | 25.96 | 15.0±5.18 | 15.78±5.34*** | 5.18 |
Paired Sample t-Test was used to analyse within the group differences in Continuous Variables; BMI: Body mass index; SCI-QoL: Spinal cord injury-quality of life index; SCIM: Spinal cord injury independence measure; MEDS: Medically based emotional distress scale; The significance is presented as *p<0.05; *p<0.01, *p<0.001; Within group: pre compared with post; @@@p<0.001; @ p<0.05; Comparison between group: Pre-compared with Pre, and Post compared with Post.
Within and between group comparison of categorical variables of IYP and PT groups.
| Variables | IYP | PT |
|---|
| Pre | Post | Total | p-value | Pre | Post | Total | p-value |
|---|
| CRP | Negative | 14 (100%) | 0 (0.0%) | 62 (100%) | <0.001* | 11 (64.7%) | 06 (35.3%) | 62 (100%) | =0.035* |
| Positive | 34 (70.8%) | 14 (29.2%) | =0.027@ | 17 (37.8%) | 28 (62.2%) | =0.086@ |
| ASIA | C | 24 (53.3%) | 21 (46.7%) | 62 (100%) | <0.001* | 30 (71.4%) | 12 (28.6%) | 62 (100%) | <0.001* |
| D | 0 (0.0%) | 17 (100%) | <0.001@ | 0 (0.0%) | 20 (100%) | <0.001@ |
CRP: c-Reactive protein; ASIA: American spinal injury association; *Mc-Nemar chi-square test was used to analyse within the group differences in Categorical Variables; @chi-square test was used to analyse between the group differences in Categorical Variables
The male participants in IYP (n=54) and in PT (n=53) showed that there was a significant change in BMI (p<0.001; p<0.05), SCI-QOL Index (p<0.001; p<0.001), SCIM (p<0.001; p<0.001), and MEDS (p<0.001; p<0.005) when compared with baseline. Similarly, female participants in IYP (n=8) and in PT (n=9) also demonstrated significant improvement in BMI (p=0.477; p=0.429), SCI-QOL Index (p<0.001; p=0.339), SCIM (p<0.005; p<0.001), and MEDS (p<0.001; p<0.005) when compared with baseline [Table/Fig-6a,b].
Gender difference of continuous variables within the two groups.
| (a) Gender difference of IYP Group |
|---|
| IYP group | Males (n=54) | Females (n=08) |
|---|
| Variables | Pre | Post | Pre | Post |
|---|
| BMI | 24.72±3.6 | 23.89±3.3*** | 25.71±3.67 | 25.35±3.09*** |
| SCI-Qol Index | 6.75±2.8 | 9.41±2.8 (NS) | 8.05±2.07 | 11.58±1.94*** |
| SCIM | 48.11±10.57 | 56.11±11.46** | 44.88±8.53 | 55.0±11.92*** |
| MEDS | 14.95±5.43 | 11.43±4.60 (NS) | 16.74±4.49 | 9.94±3.39 (NS) |
| (b) Gender difference of PT Group |
| PT group | Males (n=53) | Females (n=09) |
| Variables | Pre | Post | Pre | Post |
| BMI | 24.29±3.69 | 23.63±4.38* | 23.93±4.64 | 23.36±4.20 (NS) |
| SCI-Qol Index | 7.31±2.69 | 8.5±3.19** | 7.65±2.99 | 8.07±3.05*** |
| SCIM | 49.87±11.33 | 52.43±12.05*** | 46.10±15.18 | 50.00±14.89** |
| MEDS | 15.17±5.26 | 15.88±5.46*** | 14.08±4.91 | 15.23±4.88** |
The significance is presented as *p<0.05, **p<0.01, ***p<0.001, and NS=Not significant; Within group: pre with post.
Between-group Comparisons
Between groups comparison showed that there was a significant difference in post scores of both the groups in the following assessments: CRP (p<0.001), SCI-QoL Index (p<0.05), MEDS (p<0.001). However, ASIA (p=0.241), SCIM (p=0.069), and BMI (p=0.475) scores were not significantly different [Table/Fig-7]. The male participants in IYP (n=54) and PT (n=53) showed that there was no significant difference in BMI (p=0.729), SCI-QOL Index (p=0.12), SCIM (p=0.109), but a significant difference in MEDS (p<0.001) in post scores of both groups. Similarly, female participants in IYP (n=8) and in PT (n=9) also demonstrated significant difference in SCI-QOL Index (p=0.012), and MEDS (p=0.019), but no significant difference in BMI (p=0.280) and SCIM (p=0.452) when post compared with post.
Between group comparison of continuous variables of IYP and PT groups.
| Variables | IYP Vs PT | IYP Vs PT |
|---|
| Pre (p-value) | Post (p-value) |
|---|
| BMI | 0.359 | 0.475 |
| SCI-QoL | 0.319 | 0.015 |
| SCIM | 0.432 | 0.069 |
| MEDS | 0.847 | <0.001 |
Independent Sample t-Test was used to analyse between the group differences in Continuous Variables
The outcome measures that were positively correlated with age in males of IYP group are BMI (r=.63, p<0.05), CRP (p<0.001), SCI-QoL Index (r=.087, p=0.532) ASIA (r=1, p<0.05), and SCIM (r=0.458, p<0.001). However, MEDS (r=-0.046, p=0.744) and BMI (r=-0.074, p=0.596) were found to be negatively correlated with age, using Pearson’s correlation. The outcome measures that were positively correlated with age in females of IYP group are CRP (r=0.385, p=-0.347), SCI-QoL Index (r=.096, p=0.821), MEDS (r=0.113, p=0.789). However, ASIA (r=-0.342, p=-0.406), BMI (r=-0.304, p=0.464), SCIM (r=-0.312, p=0.452), were found to be negatively correlated with age, using Pearson’s correlation.
The outcome measures that were positively correlated with age in males of PT group are SCI-QoL Index (r=0.513, p<0.001), MEDS (r=0.244, p=0.078) and SCIM (r=0.604, p<0.001). However, ASIA (r=-0.233, p=0.093), BMI (r=-0.159, p=0.255), CRP (r=-0.034, p=0.809), and BMI (r=-0.159, p=0.255) were found to be negatively correlated with age, using Pearson’s correlation.
The outcome measures that were positively correlated with age in females of PT group are CRP (r=-0.059, p=0.871), SCI-QoL Index (r=0.811, p=0.004), MEDS (r=0.626, p=0.053), and SCIM (r=0.845, p=0.002). However, BMI (r=-0.304, p=0.464), ASIA (r=-0.326, p=-0.358), were found to be negatively correlated with age, using Pearson’s correlation.
Discussion
This is the first randomised control trial of yoga in SCI which was done to compare the effect of IYP to PT in the management of SCI patients on ASIA score, functional independence, distress, an inflammatory marker, quality of life and BMI. The strength of the study is its study design and the large sample size. The percentage change in the post scores of ASIA, BMI, SCI-Qol, SCIM, MEDS and CRP is higher in IYP than the PT group, when compared with pre-scores. Similarly, between groups comparison showed IYP group had significantly better improvement in SCI-QoL, MEDS and CRP, than PT group which suggest that yoga therapy could be a feasible, cost-effective, easy-to-accomplish, non-pharmacological intervention aiding rehabilitation of paraplegics.
The non-pharmacological approach of yoga therapy [28,29] which encompass a combination of physical postures, voluntary breathing practices, cleansing techniques, concentration and relaxation techniques [30]. As observed in the outcomes, the positive changes in the IYP group compared to PT group may be due to psychological benefits; calming effect, increasing awareness, attention span, acceptance, adaptability and a sense of security resulting from the practice of yoga therapy [31]. The process adopted during the yoga program included stimulation and successively followed by relaxation might have helped in breaking the loop of the uncontrolled speed of thoughts (stress) [32] and better psychological health resulting from stress reduction [33] through slowly gaining mastery over the mind [34]. Increase in thalamic GABA levels, improvement in mood and anxiety levels, and a decrease in depressive symptoms has been demonstrated by 12 weeks of yoga practice, in two recent studies [35,36]. A possible mechanism is explored hereunder.
There is strong evidence showing an association of raised CRP with chronic SCI which is mainly due to prevailing systemic inflammation and not due to any infection condition [8,37,38]. As per the study protocol, authors wanted to observe whether the add-on of yoga therapy does improve chronic systemic inflammation in patients who have already undergone their primary rehabilitation. The reduction in CRP scores indicates a significant reduction in systemic inflammation in IYP group in comparison to the PT group. Reduction in inflammation can be directly attributed to a significant decrease in stress in the IYP group. Yoga has a beneficial impact on reducing stress than simple exercises, as shown in previous studies [39]. Relaxation and calming effect is unique to yoga which in turn helps to modulates Hypothalamus-Pituitary-Adrenal-Axis (HPA-axis) and resulted in reducing inflammation [40]. It is likely that yoga practice improves immune function [41] and this could add to bring a significant change in the parameters measured.
The present study reported the functional improvement (in areas such as self-care, respiration, sphincter management and mobility) is better in IYP group (% change=17.35%) as indicated by SCIM scores as compared to PT group (% change=5.64%), though no significant differences were observed in between the two groups. This finding aligns with the results of another clinical trial on paraplegics where there was a highly significant improvement in spasticity and gait after receiving yoga therapy [42].
Emotional distress is well managed by yoga which is reflected in the reduction of symptoms score of MEDS. Improvement in emotional distress results in decreased sympathetic activity and may be attributed to better autonomic modulation. The function of the Autonomic Nervous System (ANS) becomes more specific resulting in a tilt in balance in favour of the Parasympathetic Nervous System (PNS), in turn resulting in emotional stability and distress reduction [11]. Previous studies have shown that yogic practices handle anxiety and depression well, resulting in enhanced self-esteem and betterment in performances of Activities of Daily Living (ADL) [43]. A six-week specialised yoga program has shown similar results where there have been significant improvements in depressive symptoms, mindfulness and self-compassion in yoga group compared to control [13]. Thus, improvement in SCI-QoL Index can be attributed to improvement in psychological states due to yogic practices.
Yoga postures (asanas) are targeted to extend the spine in controlled measure and also to twist the spine gently. These asanas could increase blood flow in the spinal arteries and thus bring improved oxygen with increased healing possibilities, as demonstrated by a previous study [15]. Neural tissue plasticity can be promoted by several factors including neurotrophic factors, neurotransmitters, endocrines, cytoskeleton proteins and neuronal electrical activity to name a few [16]. The practice of yoga can enhance the above mentioned factors and could have possibly increased the production of neurotrophic factors (e.g., -BDNF, VEGF, IGF-1 etc.,) that would have mediated neurogenesis and neuroplasticity [44,45]. This, in turn, is likely to improve sensory, motor and autonomic function in SCI patients. Hence, the current study clearly showed that because of add-on of yoga therapy, improvements in IYP group was better than the PT group [Table/Fig-8].
Summarises possible mechanism for add-on yoga module in improving patient outcomes in SCI.
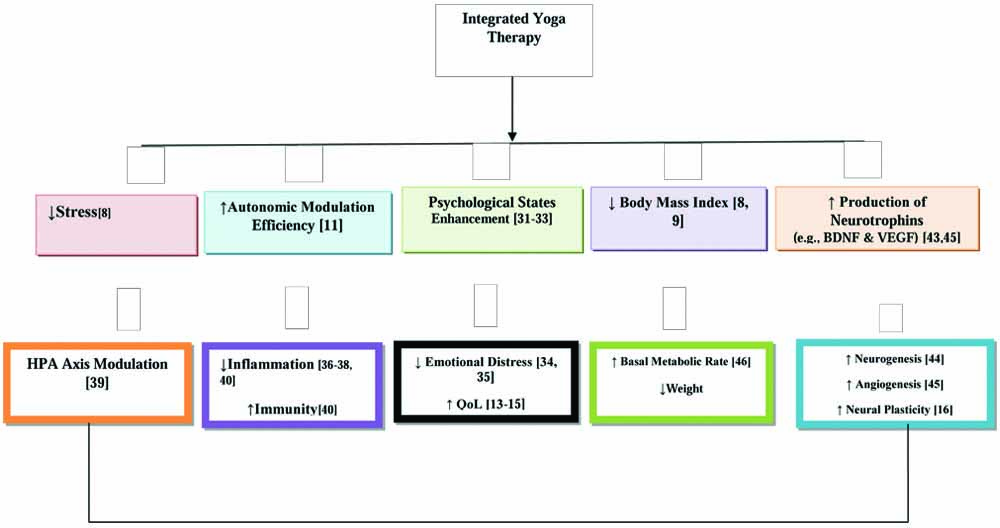
Though both groups (IYP and PT) showed improvements in the scores of BMI and ASIA, the magnitude of change was higher in participants of IYP group compared to participants of the PT group. This indicates that add-on of yoga therapy with physiotherapy, increases basal metabolic rate, enhancing metabolism and more fat oxidation [46]. Therefore, better metabolic regulation has resulted in weight reduction and improvement in sensory and motor function leading to better mobility.
Limitation
The main limitation of the study was that it was conducted on paraplegia patients belonging to one rehabilitation centre and the results were not able to rule out the effect of other rehabilitation activities such as vocational training and occupational therapy. Hence more studies are needed including more centres.
Conclusion
Authors conclude that improvements in stress resulted in a decrease in inflammation and enhanced emotional stability resulting from better autonomic modulation. Improvement in psychological states resulted in better QoL, and reduction in BMI increased Basal Metabolic Rate (BMR), leading to significant improvement in overall functional independence. The study might be improvised in design by further conducting a multi-centric trial and including radiological investigations for a better understanding of the underlying processes involved.