Spinal anaesthesia is the preferred technique for most of the lower abdominal surgeries. It is more advantageous than general anaesthesia i.e., minimum haemodynamic disturbances with minimum stress response, optimal operative conditions and less chance of post-operative morbidity [1]. For spinal anaesthesia lignocaine was the local anaesthetic agent of choice for decades, due to its rapid onset of action, good motor block and good muscle relaxation [2]. Advantage of bupivacaine over lignocaine is 3-4 times more potent with longer duration of action while disadvantages are a slow onset of action and decreased motor block [2]. Hyperbaric bupivacaine 0.5% is widely used in spinal anaesthesia. Main disadvantage of spinal anaesthesia with bupivacaine 0.5% is it won’t prolong duration of post-operative analgesia [2]. Therefore, research for a drug that may decrease the severity of post-operative pain with minimal side effects seems mandatory. A number of adjuvants have been used to improve post-operative analgesia, along with the bupivacaine. These are opioids, epinephrine, clonidine, dexmedetomidine, midazolam, neostigmine and ketamine [3].
Ketamine is a non-competitive antagonist of NMDA receptors. It became a valuable drug for neuraxial administration in wide clinical situations due to its spectrum of actions [4,5]. Ketamine can be used for post-operative analgesia, chronic pain and surgical anaesthesia [3]. According to existing literature Intrathecal ketamine with bupivacaine has minimal cardiovascular disturbance.
Authors undertook this study to investigate the hypothesis that intrathecal ketamine as an adjuvant increases the duration of post-operative analgesia along with better haemodynamic stability.
The present primary outcome was to assess the duration of post-operative analgesia between two groups i.e., bupivacaine alone and bupivacaine with ketamine, and secondary outcome were to assess the intraoperative and post-operative haemodynamic stability, onset and duration of sensory as well as motor block, side-effects of injection ketamine when given intrathecally as an adjuvant with injection bupivacaine.
Materials and Methods
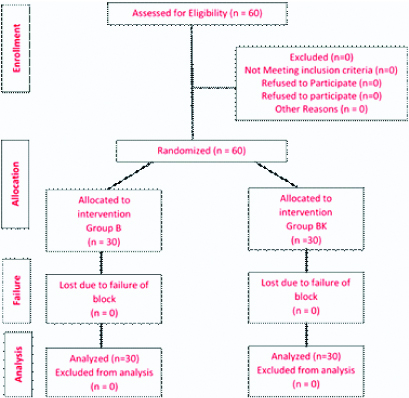
The present randomised comparative study was carried out after the approval of Ethics and Screening Committee; Reference number: DMIMS(DU)/IEC/2017-2018/6635 and written informed consent of the patients. The study was conducted from October 2017 to September 2018. Sixty patients from both sexes aged between 20-60 years with ASA Grade I and II who were scheduled for lower abdominal surgeries like hysterectomies, herniorrhaphy and appendicectomies under subarachnoid block, were selected randomly [Table/Fig-1].
CONSORT FLOW diagram for patient allotment.
Patient’s refusal, patients with spinal abnormality, bleeding diathesis or neurological diseases and head injury cases were excluded from the study.
As a result of the power analysis, it was decided that each group should have at least a minimum of 28 cases (80% power and 0.05% α error). Considering possible data loss due to technical reasons, both groups were admitted 30 patients. Sixty patients were divided randomly into two groups of 30 each by using computer-generated random number table. Group B i.e., Bupivacaine received intrathecal bupivacaine 12.5 mg (2.5 mL)+1.0 mL normal saline (total volume of 3.5 mL) whereas Group BK i.e., Bupivacaine+Ketamine received intrathecal bupivacaine 12.5 mg (2.5 mL)+1 mL (50 mg) Ketamine (total volume of 3.5 mL).
All patients were preloaded with Lactated Ringer’s solution 500 mL. Under aseptic precautions, lumbar puncture was done in sitting or lateral position by midline approach by using disposable Quinkes spinal needle (25 G) at L3-L4 intervertebral space and the study drug according to group was administered. After, Subarachnoid block, oxygen (4 mL/minute) by Hudson mask was given. Fluid therapy was maintained with Lactated Ringers Solution (2 mL/kg/hour) or Normal saline (2 mL/kg/hour). HR, SBP and DBP monitored at 0, 1, 3, 5 minutes and at an interval of five minutes till 30 minutes and at 45, 60,120 and 180 minutes till patient requires first rescue analgesia.
The following parameters were noted: The onset of sensory block was tested by pinprick using a hypodermic needle. The time of onset was taken from the time of injection of drug into subarachnoid space to loss of pinprick sensation till T10 level. The highest level of dermatomal segment was noted. Time for two segment regressions from highest level of sensory block was achieved was noted. The duration of sensory blockade was taken as time taken for four dermatomal segments regression from highest level of sensory blockade achieved.
Onset of motor block was assessed by Bromage scale [6] (Grade 0- Full flexion of knees and feet, Grade 1- Just able to flex knees, full flexion of feet, Grade 2- unable to flex knees, but some flexion of feet possible, Grade 3- Unable to move legs or feet). Time interval between injections of drug into subarachnoid space to the achievement of Bromage Grade 3 is taken as onset of motor block. The duration of motor block was taken from the time of intrathecal injection of drug into sub-arachnoid space to achievement of Bromage Grade 0. Duration of analgesia was taken as time taken for the first pain medication was noted (i.e., when VAS >4). Side-effects like nausea, vomiting, urinary retention, nystagmus and emergence delirium were noted and treated accordingly. Neurological examination was done to rule out any neurological deficits at discharge.
Statistical Analysis
Statistical analysis was done by using descriptive and inferential statistics using chi-square test and Student’s t-test. Software used in the analysis was SPSS version 17.0 and p<0.05 is considered as level of significance.
Results
Sixty patients were evaluated, 30 patients in each group and no patient was excluded at any stage of the study. The demographic data regarding age, gender distribution in study patients, weight, height and duration of surgery were similar in both the study groups [Table/Fig-2].
| Patients characteristics | Group B | Group BK | p-value |
|---|
| Age (years) | 40.3±7.5 | 43.4±7.8 | t=1.56;p=0.12, NS |
| Gender (male/ female) | 14/16 | 11/19 | χ2=0.60;p=0.43, NS |
| Height (cm) | 157.5±6.2 | 158.2±7.4 | t=0.39;p=0.69, NS |
| Weight (kilograms) | 53.2±6.0 | 54.5±5.8 | t=0.85;p=0.39, NS |
| Duration of surgery | 90±22.4 | 88±20.5 | t=0.36p=0.71, NS |
The mean onset of sensory block was faster in Group BK (3.46±0.84 minutes) compared to Group B (4.7±0.7 minutes), which was statistically significant (p≤0.001). The mean onset of motor block was clinically faster in Group BK (5.10±0.1 minutes) compared to Group B (5.18±0.1 minutes) but it was no statistically significant difference in both groups. (p=0.99) [Table/Fig-3].
Block characteristics and duration of analgesia.
| Block characteristics | Group B | Group BK | t-value | p-value |
|---|
| Onset of Sensory block (min) | 4.7±0.7 | 3.46±0.84 | 7.05 | <0.001, S |
| Onset of Motor block (min) | 5.18±0.1 | 5.10±0.1 | 3.10 | 0.99, NS |
| T6 sensory block achieved | n=27 (90%) | n=28 (93.3%) | χ2=0.21 | 0.64, NS |
| Time for Two segment Regression (min) | 59.2±16 | 63.2±11.3 | 1.11 | 0.26, NS |
| Duration of Motor block (min) | 161.9±8.2 | 162.8±8.4 | 0.41 | 0.67, NS |
| Duration of Sensory block (min) | 216.8±12.9 | 303.3±30.2 | 14.42 | <0.001, S |
| Total Duration of Analgesia (min) | 227.8±13.9 | 326.3±32.1 | 15.42 | <0.001, S |
Maximum patients in the present study achieved T6 level with no statistically significant difference in both groups. (p=0.64) The mean time for 2 segment regression in Group BK was 63.2±11.3 minutes whereas, in Group B it was 59.2±16 minutes with no statistically significant difference in both the groups (p=0.26) [Table/Fig-4].
The mean duration of motor block in Group BK was 162.8±8.4 minutes and in Group B it was 161.9±8.2 minutes which was statistically not significant (p=0.67). The mean duration of sensory block was more in Group BK (303.3±30.2 minutes) compared to Group B (216.8±12.9 minutes), which was statistically significant (p=0.001). Mean duration of analgesia is more in group BK (326.3±32.1 min) compared to Group B (227.8±13.9), which was statistically significant (p=0.001) [Table/Fig-3].
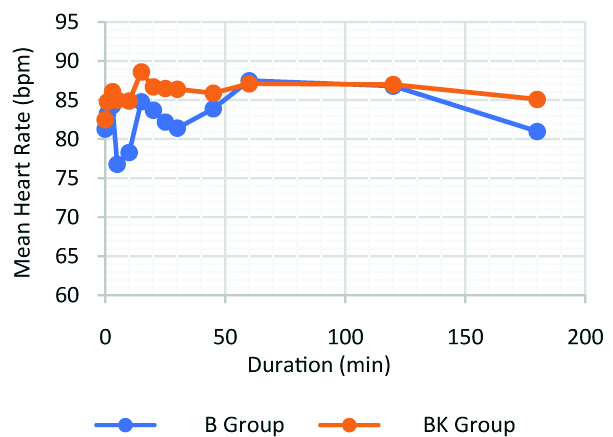
Both the groups were comparable throughout the study period with respect to mean heart rate except at five minutes and 10 minutes there was a significant decrease in mean heart rate in patients belonging to Group B compared to Group BK (p<0.05). This indicates that patients belonging to Group BK where more stable during 1st 10 minutes after spinal anaesthesia as per heart rate [Table/Fig-4].
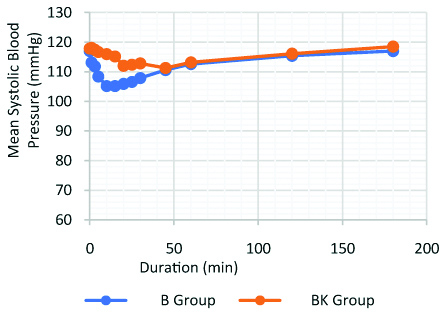
After inducing each patient with spinal anaesthesia, decrease in mean systolic blood pressure was observed in group B for first 30 minutes whereas in group BK there was no significant decrease in mean SBP. This indicates that patients belonging to group BK were haemodynamically more stable with respect to mean systolic blood pressure. From 30 minutes to the end of the study, systolic blood pressure came to its baseline value in Group B. Compared with the Group B, Group BK showed more stable mean systolic blood pressure through the study period [Table/Fig-5].
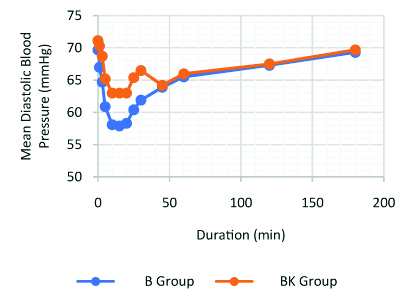
Similar trends were observed in the mean diastolic blood pressure when compared with the mean systolic blood pressure. Compared to Group B, Group BK showed more stable mean diastolic blood pressure throughout the study period [Table/Fig-6].
Diastolic blood pressure.
There was no statistically significant difference between the two groups with respect to side-effects. In Group B, four patients experienced nausea and vomiting and two patients had urinary retention whereas in group BK, two patients had nystagmus and two patients had emergence delirium. Nausea and vomiting was treated by giving inj. Ondansetron 0.1 mg/kg. Emergence delirium was treated by giving inj. Midazolam 0.05 mg/kg [Table/Fig-7].
| Side effect | B Group (n=30) | BK Group (n=30) | p-value |
|---|
| Nausea/Vomiting | 4 (13.3%) | 0 (0%) | χ2=0.52;p=0.46, NS |
| Nystagmus | 0 (0%) | 2 (6.6%) |
| Emergence delirium | 0 (0%) | 2 (6.6%) |
| Urinary retention | 2 (6.6%) | 0 (0%) |
| Neurological deficit | 0 (0%) | 0 (0%) |
Discussion
The present study design consisted of 60 patients aged between 20-60 years, ASA Physical Status I, II undergoing elective lower abdominal surgeries under spinal anaesthesia and were randomly divided into two groups with each group having 30 patients. Mean duration of onset of sensory block was faster in Group BK compared to Group B, which was statistically significant. These findings correlate with the study done by Togal T et al., in which they found that there was more rapid onset of sensory block in bupivacaine+ketamine group which was 3.4 minutes than bupivacaine alone group which was 4.7 minutes, this was statistically significant as p-value was 0.008 [7]. Similar results were cited by other researchers also comparable with the results of the present study [8-10].
Onset of motor block was clinically faster in Group BK compared to Group B but there was no statistically significant difference in both groups. Similar results were obtained by Kathirvel S et al., where they found that onset of motor block in bupivacaine group was 6.5±1.5 minutes and bupivacaine+ketamine group was 5.6±0.7 minutes, but it was statistically not significant [11]. Patients were comparable in both the groups with respect to highest level of sensory block and the time taken for two segment regressions [Table/Fig-3]. The mean duration of motor block in Group BK was shorter than Group B with no statistical significance. Similar study was conducted by Togal T et al., and found that the duration of motor blockade was shorter in bupivacaine+ketamine group i.e., it was 114 minutes whereas it was 130 minutes in bupivacaine group [7]. This was statistically not significant.
The mean duration of sensory block is more in Group BK compared to Group B, which was statistically significant. Similar results obtained by Sivatharshini P et al., also found that the mean duration of sensory block was longer in group bupivacaine+ketamine group with 306.8 minutes compared to the group bupivacaine with 211.4 minutes which was statistically significant [12]. Similar results were also obtained by previous studies [Table/Fig-8] [9,12-15]. The mean duration of analgesia was more in ketamine Group BK compared to Group B, which was statistically significant.
A comparative table on duration of analgesia [9,12,14,15].
| Studies | Drugs used | Duration of analgesia |
|---|
| Krishna TM et al., [14] | Bupivacaine 3 mL | 331.5±89.8 minutes |
| Bupivacaine 3 mL+ketamine 0.1 mg/kg | 369.7±124.2 minutes |
| Patel I et al., [15] | Bupivacaine 1.8 mL+0.5 mL normal saline | 2.19±0.15 hours |
| Bupivacaine1.8 mL+ketamine 25 mg | 3.50±2.1 hours |
| Hemanth N et al., [9] | Bupivacaine 3 mL+0.5 mL normal saline | 127.8±12.8 minutes |
| Bupivacaine 3 mL+ketamine 0.1 mg/kg | 150.8±11.7 minutes |
| Sivatharshini P et al., [12] | Bupivacaine 2.5 mL+0.5 mL normal saline | 222.7±15.6 minutes |
| bupivacaine 2.5 mL+ketamine 25 mg | 322.8±29.4 minutes |
Mechanism of action of ketamine with respect to analgesic effect: Ketamine’s primary site of CNS action is the thalamocortical projection system. It selectively depresses neuronal function in parts of the cortex while stimulating parts of limbic system. Ketamine produces a dose dependent effect on pain processing by decreasing activation of the secondary somatosensory cortex, insula and anterior cingulate cortex. It also occupies the opiate receptors in the brain and spinal cord which is responsible for analgesia. The spinal cord analgesic effect of ketamine is postulated to be due to inhibition of dorsal horn [16].
The patients belonging to group BK were more stable during 1st 10 minutes after spinal anaesthesia as per heart rate. This inference was concurrent with the study done by Kathirvel S et al., Hussain AM et al., and Jamadar NP et al., wherein they observed heart rate on higher side in ketamine group [Table/Fig-4] [11,17,18]. Compared with the Group B, Group BK showed more stable mean systolic and diastolic blood pressure. Similar results were obtained by Bion JF, and Basuni AS, wherein they found that addition of intrathecal ketamine to bupivacaine provided more haemodynamic stability in mean systolic and diastolic blood pressure compared to bupivacaine alone [Table/Fig-5,6] [19,20].
There were no statistically significant side-effects in both the groups [Table/Fig-7]. Ketamine is associated with unpleasant side-effect i.e., emergence delirium, it is generally regarded as being mediated through ketamine’s agonistic effect on the dopamine DA-2 receptor. Two patients in Group BK had emergence delirium in post-operative period, which was treated with intravenous dose of 5 mg of haloperidol as haloperidol has been documented to have a strong antagonistic effect on the DA-2 receptor [21]. From the above findings, authors can suggest that routine use of intrathecal ketamine as an adjuvant to hyperbaric bupivacaine for subarachnoid block in patients posted for various lower abdominal surgeries as it provides better haemodynamic stability and longer duration of post-operative analgesia.
Limitation
A limitation of the present study is all patients were either ASA physical status I or II, results cannot be generalised to ASA physical status III and IV patients.
Conclusion
On basis of the present clinical comparative study, authors can conclude that the addition of 1 mL (50 mg) ketamine to 0.5% hyperbaric bupivacaine 12.5 mg (2.5 mL) in spinal anaesthesia decreases onset of sensory block, and prolongs the duration of sensory blockade. It also prolongs the duration of analgesia and improves with better haemodynamic stability as compared to bupivacaine alone. It can be used as a beneficial additive for prolonging spinal anaesthesia.