Statistics show that of the 56 million global deaths in 2012, 68% were due to non-communicable diseases [1]. It is like an incessant and murky pool where the number of people, families and communities afflicted are increasing. WHO typically refers to four major risk factors for NCDs: poor diet, physical inactivity, tobacco use, and harmful alcohol use [2]. The relationship of cancer, cardiovascular diseases and respiratory diseases with smoking had been proven a long time ago. Excessive alcohol intake, unhealthy diet, physical inactivity and obesity have been deemed as a very important risk factor for most non-communicable diseases mentioned in the article [3]. When it comes to oral diseases, the burden of oral diseases still remains a predicament in many parts of the world and there remains a wide lacuna for improvement in the oral healthcare setups [4]. Dental caries is a disease of multifactorial etiology. Its prevalence is influenced by a number of factors like age, ethnicity, gender, dietary patterns and oral hygiene practices to name a few [5]. Various risk factors like smoking, excessive alcohol consumption, low socioeconomic status, stress levels, diabetes mellitus type 2, presence of certain microorganisms like P gingivalis, T forsythia and A. Actinomycetemcomitans contribute to periodontitis [6]. The significant role of socio-behavioural and environmental factors in oral diseases is evidenced in an extensive number of epidemiological surveys [7]. Hence, modification of socio-behavioural risk factors is the best line of action to combat this problem. Thus, both these conditions (NCDs and oral diseases), are largely caused by a cluster of risk factors like tobacco, unhealthy diet, physical inactivity and harmful use of alcohol [3].
Standalone studies have been attempted to link NCDs like diabetes and periodontitis [11], but the results seem inconclusive and fragmented. As it is not pertinent enough to affect a policy change of achieving a paradigm shift of placing oral health strategies under the NCDs umbrella, additional evidence is required. There seems to be a dearth of pressing evidence to substantiate its claims of common risk factors between the oral diseases and communicable diseases. Hence, this study was designed to ascertain evidence on the risk factors being common to both NCDs and oral diseases and thus, empirically prove the statements put forward regarding shared risk factors. This study will be able to fill epidemiological gap of quantification of the common risk factors, which would in turn might assist in placing the ‘oral health’ under NCDs prevention. Furthermore, it could encourage the oral diseases to be included under the NCDs programs. Hence, the integration of both oral diseases and NCDs would be an appropriate action for combating factors at a lower cost, greater efficiency and effectiveness than disease specific approaches. A ‘horizontal approach’ by integrating all NCDs and oral disease is proposed.
Materials and Methods
Study design and study type: Observational, cross-sectional.
Study setting: The study was conducted at two tertiary care hospitals in Cochin, Kerala, India.
Study duration: A pilot study was done in December 2014. The data collection was done from January 2015 to October 2015.
Ethical approval for the study was obtained by Institutional Ethical Committee: SRC/MDS/ASD/14-15/024.
Study population: Patients diagnosed within a month with non-communicable diseases like Diabetes Mellitus type 2, Myocardial Infarction, Hypertension, Asthma, Chronic Obstructive Pulmonary Diseases (COPD) and Stroke were selected from hospitals. They were already on the medication for the condition they were diagnosed. The study participants did not have any comorbidities like infectious diseases or other diseases other than the non-communicable diseases taken into consideration. The 280 patients (70 from each NCDs) were selected from the departments of Endocrinology, Pulmonology, Cardiology and Neurology, based on their recent diagnosis and the consulting physicians’ advice.
Data collection of risk factors: The assessment of risk factors of the NCDs and oral diseases (dental caries and periodontal disease) were carried out by three methods; patient interview, data from their medical records and interview of the consulting physician.
A validated structured questionnaire for enumerating the risk factors was devised for the interview and the questionnaire consisted of two sections. The first section comprised of the demographic characteristics of the study participant and the risk factors of the non-communicable disease in question. The interview was carried out by the Principal Investigator. The patient was interviewed for nearly 15-20 minutes, where all the relevant questions regarding their exposure to the stipulated risk factors were assessed. The patients’ medical records were accessed to obtain the missing information, validate the details provided by the patient and to obtain the values of blood pressure, lipid and blood glucose levels. After patient interview, the consulting physician was interviewed to discuss the case and recount the possible risk factors. The second section comprised of the oral disease diagnosis, risk factors of oral diseases (dental caries and periodontal disease) and clinical oral examination including DMFT index, Simplified Oral Hygiene Index (OHI-S) and Community Periodontal Index (CPI) with Loss of Attachment (LoA).
Validity of questionnaire: The content validity of the questionnaire was done by three experts each in the field of dentistry, endocrinology, pulmonology, cardiology and neurology using Content Validity Index (CVI). The CVI of the scale was 0.94 (oral diseases), 0.83 (diabetes), 0.86 (hypertension), 0.86 (myocardial infarction), 0.89 (stroke), 0.95 (asthma) and 0.80 (COPD). The absence of a similar study warranted pre-testing the developed questionnaire on a random sample of 15 patients with any of the above said non-communicable diseases to assess practicability, validity, cogency and interpretation of responses. The assessments of this pilot study were utilised for the planning and execution of the main study and to finalise the proforma/interview template to be used for data collection.
Informed consent: The proposal to the study was submitted and approved by the Institutional Ethical Committee. Written informed consent was obtained from all the willing participants prior to the interview. Confidentiality was ensured about patient details.
Bias: In this study, selection bias was controlled by selecting only physician diagnosed patients as study participants. The information bias was controlled by validating the risk factors obtained from the patient interview by cross checking with the patient records and consultation with the treating physician. The patient recruitment was done exclusively based on the NCD diagnosis irrespective of the presence or absence of any oral diseases in the patient. This also helped eliminate selection bias. Confounders were controlled by the stringent inclusion and exclusion criteria followed in the study.
Sample size: Sample size was calculated with 95% confidence interval and 5% absolute error. The formula n=4pq/L2 was used for the sample size calculation. The prevalence of periodontitis in type 2 diabetic patients in India (86%) was used to calculate the sample size as this was the most frequently prevalent relationship between an oral and a non-communicable disease [12]. Thus the sample size was calculated to be 192, rounded up to 200 and was divided equally among all the four groups of NCDs (50 each). In order to account for missing data from patient records, patient recall bias, chances of non-response and withdrawal from the study; a 40% addition to samples were considered which accounted in a final sample size of 70 patients in each group of NCDs making the total of 280.
Statistical Analysis
Data analyses were done using Statistical Package for Social Sciences (SPSS) for Windows package version 17. The data obtained was tabulated and analysed using descriptive statistics and risk factors were expressed as percentages. Bivariate analysis using Cohen’s Kappa was done to assess the degree of agreement of the common risk factors with the oral diseases and the NCDs. A 2×2 table was obtained to calculate the degree of agreement, which were also expressed in percentages.
Results
[Table/Fig-1] outlines the demographic characteristics of the six study cohorts. [Table/Fig-2] shows the degree of agreement (Kappa values) of the common risk factors with all the NCDs included in the study and oral diseases separately and cumulatively. When the oral diseases (dental caries, periodontitis and edentulism) were considered cumulatively, there was only 4% degree of agreement for hypertension as a common risk factor between stroke and oral diseases. Atrial fibrillation had 2% degree of agreement and oral contraceptives use had a good 23% degree of agreement between strok and oral diseases. Among dental caries and hypertension, genetic predisposition was seen as the most common risk factor accounting for 12% of the people. It was observed that, smoking had 15% degree of agreement in patients with COPD as a common risk factor between COPD and dental caries. In case of periodontitis, it was 7% and when all the oral diseases (dental caries, periodontitis and edentulism) were seen cumulatively, smoking had 10% degree of agreement.
Demographic details of the study population.
| Variables | Diabetes mellitus type 2 | Stroke | MI | Hypertension | COPD | Asthma |
|---|
| Mean age | 60 (±9.1) years | 57.40 (±13) years | 62 (±9) years | 63 (±11) years | 60 (±13) years | 45 (±19.7) years |
| Gender | Male | n=36 | n=42 | n=28 | n=21 | n=26 | n=15 |
| 51.4% | 60% | 80% | 60% | 74% | 43% |
| Females | n=34 | n=28 | n=07 | n=14 | n=09 | n=20 |
| 48.6% | 40% | 20% | 40% | 26% | 57% |
Degree of agreement (Kappa values) of all the risk factors being common to both the NCDs and oral diseases.
| NCD+Oral diseases kappa values | Risk Factors |
|---|
| Blood pressure | Smoking | Obesity | Family history | Cholesterol | Diabetes | Atrial fibrillation/cardiac valve problems | Alcoholism | Oral contraceptives |
|---|
| DM+DC | 0.05 | 0.15 | 0.02 | 0.14 | 0.07 | - | - | - | - |
| DM+PD | 0.00 | 0.14 | 0.02 | 0.14 | 0.08 | - | - | - | - |
| DM+OD | 0.03 | 0.03 | 0.03 | 0.03 | 0.04 | - | - | - | - |
| ST+DC | 0.02 | 0.03 | - | 0.18 | 0.08 | 0.18 | 0.31 | 0.04 | 0.01 |
| ST+PD | 0.00 | 0.14 | - | 0.05 | 0.04 | 0.06 | 0.13 | 0.02 | 0.15 |
| ST+OD | 0.04 | 0.00 | - | 0.00 | 0.01 | 0.01 | 0.02 | 0.00 | 0.23 |
| MI+DC | 0.18 | 0.06 | 0.01 | 0.04 | 0.07 | 0.44 | - | 0.13 | - |
| MI+PD | 0.08 | 0.11 | 0.15 | 0.14 | 0.23 | 0.17 | - | 0.06 | - |
| MI+OD | 0.05 | 0.05 | 0.01 | 0.06 | 0.05 | 0.03 | - | 0.01 | - |
| HT+DC | - | 0.00 | 0.09 | 0.12 | - | 0.00 | - | 0.13 | - |
| HT+PD | - | 0.01 | 0.07 | 0.24 | - | 0.11 | - | 0.13 | - |
| HT+OD | - | 0.05 | 0.01 | 0.05 | - | 0.05 | - | 0.05 | - |
| COPD+DC | - | 0.15 | - | - | - | - | - | - | - |
| COPD+PD | - | 0.07 | - | - | - | - | - | - | - |
| COPD+OD | - | 0.01 | - | - | - | - | - | - | - |
| AST+DC | - | 0.04 | 0.01 | 0.14 | - | - | - | - | - |
| AST+PD | - | 0.28 | 0.23 | 0.05 | - | - | - | - | - |
| AST+OD | - | 0.03 | 0.03 | 0.05 | - | - | - | - | - |
DM: Diabetes mellitus type 2; ST: Stroke; MI: Myocardial infarction; HT: Hypertension; COPD: Chronic obstructive pulmonary disease; AST: Asthma; DC: Dental caries; PD: Periodontal disease; OD: Oral diseases (dental caries+periodontal disease+edentulism)
It was observed that obesity had only 1% degree of agreement as a common risk factor between dental caries and asthma, 23% agreement as a common risk factor between periodontitis and asthma and 3% degree of agreement as a common risk factor between oral diseases collectively and asthma.
Discussion
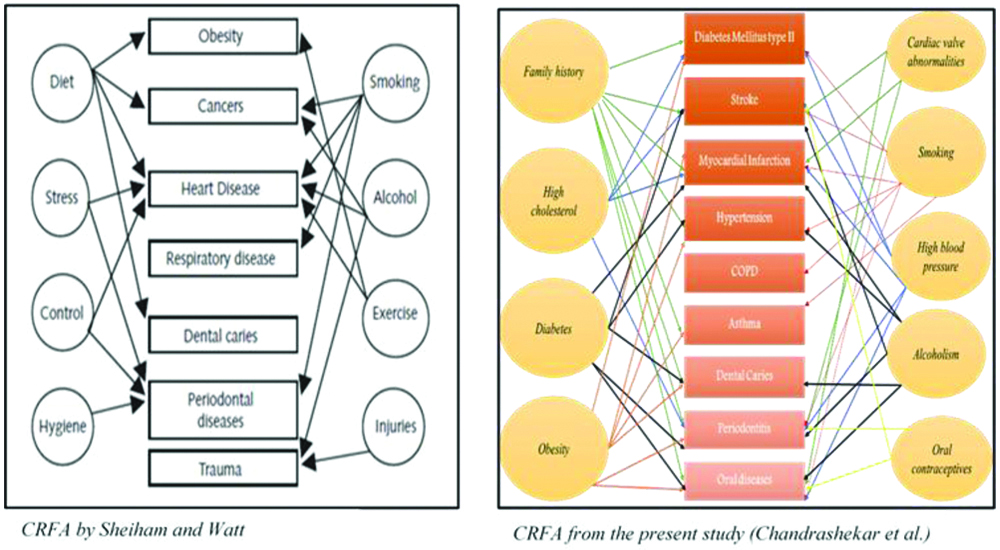
The common risk factor approach model proposed earlier by Sheiham A et al., lacked many of the risk factors we have identified in the present study [Table/Fig-3] [9]. Although, the present study could establish the ‘Common Risk Factor Approach’ by Sheiham and Watt with evidence backed information, the key concept underlying the integrated common risk approach was the same. It reinforced the fact that, controlling a small number of risk factors may have a major impact on many diseases at a lower cost, greater efficiency and effectiveness than disease specific approaches.
Comparison of the Common Risk Factor Approach (CRFA) model proposed by Sheiham A E et al., and the model conceptualised from the present study [9].
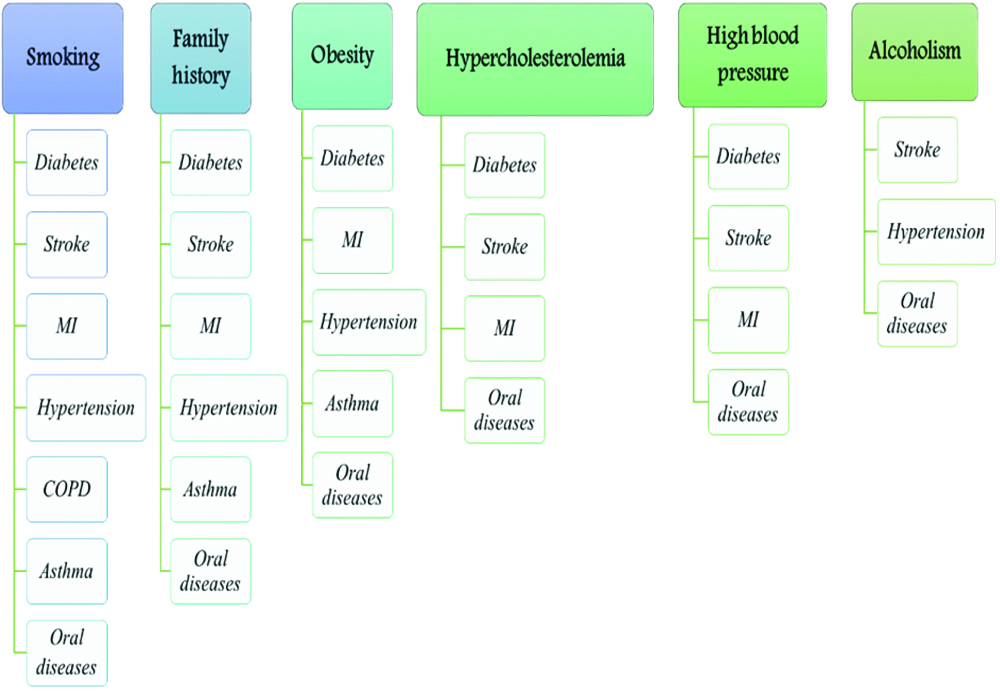
Smoking was the most prevalent and frequent risk factor isolated from this study [Table/Fig-4]. It is a modifiable risk factor and preventive strategies should encompass anti-smoking propagandas since, the elimination of smoking can drastically reduce almost all the non-communicable diseases including oral diseases. The second most common risk factor observed was family history which is a non-modifiable risk factor. Obesity, another modifiable risk factor, was common to diabetes, MI, hypertension, asthma and oral diseases. Hypercholesterolemia, high blood pressure and alcoholism were also appreciated as common risk factors. Though not as rampant across all the NCDs compared to smoking or obesity, it abetted diseases like diabetes, stroke, MI and oral diseases.
Risk factors observed in the present study.
In our study, smoking was a common risk factor between dental caries and diabetes and also; periodontitis and diabetes. Smoking has been identified in many studies as a major preventable risk factor for periodontal disease and tooth loss in the general population with diabetes [13]. In another study, tobacco consumption was seen as a risk factor for both dental caries as well as periodontitis [14]. The exact mechanism of how smoking increases the risk of diabetes and deteriorates glucose homeostasis has not been fully elucidated but it is understood that, smoking increases inflammation and oxidative stress, which directly damages the β-cell and endothelial function [15]. In a prospective study, shepherded by the American Diabetes Association, it was observed that the incidence of diabetes increased in people with pack years more than 20 (p=0.001) [16]. Thus, as anticipated, in the present study, the highest pack years recorded was 60 and there was a significant proportion of people with pack years >20. Smoking is said to exert a substantial destructive effect on the periodontal tissues and increases the rate of periodontal disease progression and tobacco smoking modifies the host response to the challenge of bacteria in microbial dental plaque [17]. The present study did not show a strong association for high cholesterol and high blood pressure as a common risk factors between oral diseases (both separately and collectively) and diabetes. It is observed that a common link between patients with both heart conditions and periodontal disease may be elevated levels of C-reactive protein (CRP), a marker for the inflammatory response [18].
Obesity individually is a major risk factor and is associated with various comorbidities including Hypertension (HTN), type 2 diabetes mellitus, dyslipidaemia, obstructive sleep apnoea, certain cancers, major cardiovascular diseases like MI and numerous oral diseases [19-24]. In the present study, it was observed that there was a 3% agreement when obesity was assessed as a common risk factor between diabetes and oral diseases. Saito T et al., clearly elucidates, how obesity is related to visceral fat accumulation, which increases the risk of type 2 diabetes. The same study also showed that obesity was directly related to periodontitis after adjustment of known risk factors [25]. The World Health Organisation also says that obesity is an independent risk factor in many oral diseases [26].
In the present study, the family history/genetics as a common risk factor between diabetes and oral diseases was not very significant, even though, studies quote that ‘Common genetic factors may be involved in the susceptibility for diabetes and periodontitis [27]. In the present study, there was 31% degree of agreement of cardiovascular abnormalities contributing to both stroke and dental caries. A Swedish study concluded that, children with complex heart diseases had more caries in the primary dentition than healthy age and gender matched controls in spite of intensive preventive efforts [28]. The authors say, it could be because, the children on cardiac medications can have lower salivary secretion which in turn could contribute to increased risk of dental caries [28]. Furthermore, Scannapieco et al., in a systematic review showed that moderate degree of evidence exists to support an association between periodontal disease and cardiac abnormalities [29].
People with diabetes are at a two fold increased chance of having stroke [30]. Diabetes also acts as a direct and indirect risk factor for dental caries [31]. One theory in support of this relationship says that, it could be because, in diabetic patients, xerostomia may occur due to pronounced polyuria, which further aggravates the chances of dental caries [31]. Smoking, is a prominent risk factor in causing stroke [32]. Literature shows that, the plausible mechanisms by which tobacco smoke exposure can increase the risk of stroke are numerous. It includes blood related conditions like carboxyhemoglobinemia, increased platelet aggregation, amplified fibrinogen levels and reduced HDL-cholesterol [33]. It is also seen that smoking precipitates dental caries [34] and periodontitis [35] individually; but as a common risk factor between stroke and the oral diseases, the present study found that it had a degree of agreement of only 3% and 14%, respectively.
Although, the present study only showed a 7% degree of agreement between cholesterol as a common risk factor between MI and dental caries, other studies have shown high cholesterol is an independent risk factor for MI [36]. From another study, there is also evidence of a relationship between dental caries and high cholesterol [37]. Although, there is no literature available enough to prove the direct relationship between the two, it is assumed that cholesterol has an indirect relationship with dental caries; since, sugary and fatty food causes dental caries [38] and the same fatty and unhealthy food causes high cholesterol [39]. There was 23% degree of agreement with high cholesterol as a possible common risk factor between periodontitis and MI. Katz J et al., says that even though a temporal relationship could not be established between high cholesterol and periodontitis, periodontitis was positively associated with total cholesterol and LDL cholesterol [40].
Diabetes is a major and independent risk factor for MI [41], diabetes also causes several oral diseases like periodontitis and dental caries [42,43]. In the study, the risk assessment of diabetes led to a 43% prevalence of diabetes in MI patients and 37% prevalence of diabetes in patients with oral diseases. When, the role of diabetes as a common risk factor between oral diseases and MI was assessed, there was a degree of agreement of 44%. It has been proven beyond doubt that, cigarette smokers have a higher chance of developing cardiovascular diseases [44]. Tobacco decreases the amount of oxygen the blood can carry and increases the tendency for blood to clot. Blood clots form within arteries causing a range of heart diseases [45]. With regard to the oral cavity, studies have shown that, smoking accounts for periodontitis, tooth loss and dental caries [46]. Smoking is said to exert a substantial destructive effect on the periodontal tissues and increases the rate of periodontal disease progression by modifying the host response of bacteria in microbial dental plaque [17]. Even though individually smoking was a prominent risk factor in cardiovascular and oral diseases, when it was assessed as a common risk factor between MI and oral diseases, it showed a degree of agreement of 11% only. This can be attributed to the small sample size. Alcohol acts by activating the adrenergic nervous system, thus causing constriction of blood vessels and simultaneous increase in blood flow and heart rate [47]. Excessive alcoholism is said to be an independent risk factor in oral diseases; especially periodontitis [48]. As a common risk factor between oral diseases and hypertension, alcohol had a 13% degree of agreement.
Limitation
The sample size was calculated for the most prevalent variables (oral disease in NCD, which was periodontitis in type 2 diabetic patients) and the obtained number was divided equally among all the NCDs. But, had we calculated the sample size separately for each NCD based on their individual prevalence, the results probably would have been more generalisable and significant but these studies were not available for estimation. Furthermore, as some diseases like MI and hypertension had a strong male predilection and other conditions like adult asthma was seen more among the females, gender matching could not be carried out. This study is vast and the results and ramifications are innumerable. But due to word constraints in the publication, we have not included many findings, author’s observations and discussions. We are anticipating, [Table/Fig-2] gives a bird’s eye view of the study outcome.
Conclusion
The most prevalent oral disease risk factors seen in our study cohort were; not visiting the dentist every six months, not undergoing oral prophylaxis in the past few months, unhealthy diet, brushing their teeth only once daily and positive family history predisposing to oral diseases. Not surprisingly, smoking was the most common risk factor across the oral diseases and all the six NCDs included in the study. The other common risk factors spanning across most NCDs and oral diseases were positive family history and obesity. Furthermore, alcohol abuse was also a frequently observed risk factor, especially in stroke, hypertension and oral diseases.
This study has to be validated in other populations. A cross country study, assessing the risk factors of NCDs and oral diseases across different ethnic backgrounds or geographically diverse populations is recommended. Since, NCDs are life style related diseases, having a cluster of modifiable and non-modifiable risk factors, it is advisable to conduct this same study in a culturally different population with varied lifestyles or habits. Studies with a cohort study design is recommended.
Policy Recommendations
Since, the present study was able to obtain an agreement with most risk factors being common to both NCDs and oral diseases, we were able to prove that NCDs shares certain risk factors with oral diseases. Hence, an integrated surveillance of the risk factors is proposed. The present day health promotion activities or preventive measures, aimed at isolated diseases will not bear any fruits. A more horizontal approach encompassing all the NCDs and oral diseases by integrating NCDs with oral diseases could avail positive results. Clinically, both the dentists and physicians can work in tandem to help alleviate the risk factors. Dentists can assess the presence of the common risk factors, counsel the patient and refer to the concerned physician. Government policies can also be designed to have a collaborative and collective approach by the dentists and physician.
Source of funding: The study was funded by Colgate Palmolive Ltd.
Ethical clearance: SRC/MDS/ASD/14-15/024
DM: Diabetes mellitus type 2; ST: Stroke; MI: Myocardial infarction; HT: Hypertension; COPD: Chronic obstructive pulmonary disease; AST: Asthma; DC: Dental caries; PD: Periodontal disease; OD: Oral diseases (dental caries+periodontal disease+edentulism)