Cataract is one of the leading cause of blindness across the world and is largely sequelae of diabetes. It is one of the most common complications of diabetes in the eye and upto 20% of all cataract procedures are performed for diabetic patients [1]. Diabetic retinopathy is defined as progressive dysfunction of the retinal vasculature caused by chronic hyperglycaemia resulting in structural damage to the neural retina. Microaneurysms are the first ophthalmoscopically demonstrable alteration in diabetic retinopathy and are measured as the hallmark of NPDR [2]. Cataract in patients with diabetes leads to decreased visual acuity and poses difficulty in examination of the retina adequately. Hence, it is advantageous to perform cataract surgery for diagnostic and therapeutic benefits, even if there is possible associated risk of aggravating the retinopathy.
In earlier days, cataract surgery among diabetics was threatened by the accelerated progression of diabetic retinopathy and deterioration of vision due to higher incidence of post-operative complications [3]. According to Kim SJ et al., diabetic eyes have a high incidence of central foveal thickness after cataract surgery [4]. According to some studies, clinicians should continue to sustain vigilance in diabetic patients after cataract extraction even when central macular oedema is not present immediately prior to cataract surgery, particularly in eyes with prior Diabetic Macular Edema (DME) treatment or non-central involved DME that may be at a predominantly high risk for development of central-involved Macular Oedema (ME) after cataract surgery [5,6]. However, this is usually mild and can be adequately treated by photocoagulation.
Current surgical techniques Small Incision cataract surgery (SICS) and phacoemulsification have an advantage over previously followed cataract surgeries that they allow quicker recovery of vision and lesser post-operative inflammation. The modern techniques of cataract surgery have improved results [7,8]. Recent studies have reported favourable visual acuity after cataract surgery in diabetic patients [9-11].
Cataract surgery in diabetes has good results, with high reliability and a slightly higher rate of complications than non-diabetic patients. Causes for poor visual acuity after surgery are poor pre-operative visual acuity, advanced stages of diabetic retinopathy and old age [12].
On measurement of central foveal thickness by OCT after cataract surgery eyes of diabetic patients showed higher macular thickness which led to poorer post-operative visual recovery. However, few studies are of the opinion that macular oedema following cataract surgery in diabetic eyes may take a benign path [4,13,14].
Pre-existing macular oedema in eyes of diabetic patients undergoing cataract surgery usually does not show spontaneous resolution, however, if macular oedema arises post cataract surgery it usually resolves spontaneously, more so in cases of mild non-proliferative diabetic retinopathy.
Debatable is whether implantation of Intra Ocular Lens (IOL) worsens inflammation in the diabetic eye compared to non-diabetic eyes, and also if implantation of IOL in diabetic eyes leads to higher incidence of macular oedema as compared to those left aphakic. Newer studies are in favour of lens implantation in diabetic eyes, as correction of aphakia with spectacle causes further image distortion and constriction of peripheral visual fields [15]. The need for this study is to establish the influence of glycaemic control on visual control to better advice patients before surgery. The aim of this study was evaluation and comparison of visual outcomes after cataract surgery in diabetic and non-diabetic patients: patients with and without diabetic retinopathy; assessment of post-operative complications after cataract surgery in diabetics compared to non-diabetics; and analysis of increment in central foveal thickness using optical coherence tomography, after cataract surgery. Also, through this study, we wanted to determine whether uneventful SICS/phacoemulsification cataract surgery led to adverse visual outcomes in diabetics.
Materials and Methods
This was a progressive analytical observational study, conducted over a study period of 2 years. This study included 150 patients with diabetes mellitus and 150 non-diabetic controls, who came to the Ophthalmology OPD in KMC hospital, Attavar, Mangalore for cataract surgery. A written informed consent was taken from all the patients. Pre-operative parameters were noted glycaemic control-HbA1c (glycosylated haemoglobin) levels, (if less than 6.5 or more than 6.5), type (type 1 or type 2) and duration of diabetes (in years), age and sex, type of medication for diabetes, oral hypoglycemic agents (OHA)/insulin, visual acuity using Snellen chart and intraocular pressure measured by Goldmann’s applanation tonometer, which has a measuring range of 0 to 78 mmHg [Table/Fig-1].
Profile of the patients operated for cataract.
| Age | Diabetics (Males, Females) | Non-diabetics (Males, Females) | Nuclear Cataract (Diabetic, Non-Diabetic) | Cortical Cataract (Diabetic, Non-Diabetic) |
|---|
| 40-49 | 3, 4 | 1, 8 | 3, 2 | 9, 2 |
| 50-59 | 32, 20 | 26, 24 | 29, 33 | 16, 24 |
| 60-69 | 41, 22 | 50, 20 | 48, 48 | 19, 18 |
| 70-79 | 10, 9 | 10, 4 | 8, 9 | 10, 6 |
| ≥80 | 6, 3 | 5, 2 | 5, 7 | 3, 1 |
Institutional Ethics Committee clearance was taken before the start of the study. (Reg.No.ECR/541/Inst/KA/2014) Cataract surgery phacoemulsification/Small Incision Cataract Surgery (SICS) with placement of Posterior Chamber Intra Ocular Lens (PCIOL) was performed. A superior fornix base conjunctival flap is raised and a 6 mm (or 3 mm for phacoemulsification) scleral incision is made after which a corneo-scleral tunnel is created. The nucleus is removed after anterior capsulotomy is done (emulsified by phacoprobe) and IOL is placed. Routine ophthalmological examination was performed pre-operatively and post-operatively on day 1, 2 and 6 weeks after surgery in all patients.
It included the Best Corrected Visual Acquity (BCVA), slit lamp biomicroscopy and fundus examination using direct and indirect ophthalmoscopy. Slit lamp biomicroscopy revealed grade of cataract and fundus examination revealed the grade of diabetic retinopathy if present. The patient is made to be seated comfortable at a slit lamp and asked to focus at a distant point while looking straight ahead. For direct ophthalmoscopy, the patient is seated and asked to look straight ahead. The ophthalmologist uses left eye to examine the left eye of the patient and the right eye to examine the right eye of the patient. For indirect ophthalmoscopy, the patient is made to lie and focus at a distant point while looking straight with pupils fully dilated. An indirect ophthalmoscope is used to get a clearer, more magnified view of the fundus. Uncorrected visual acuity and best corrected visual acuity (BCVA) was measured at all visits with Snellen’s 6 meter charts.
Central foveal thickness using OCT (Optical Coherence Tomography) before and after cataract surgery (6 weeks post-operatively) was measured using optical coherence tomography for 20 diabetics and 20 non-diabetics. Among the diabetics, central foveal thickness was measured for those who met the following criteria: 1) diabetes mellitus diagnosed minimum 1 year before cataract surgery; 2) uneventful surgery, conducted by senior surgeons; 3) if visualization of fundus was hampered by media opacity due to denser cataracts, such cases were excluded; 4) no evidence of proliferative diabetic retinopathy or macular oedema at baseline. This restricted the diabetic spectrum to eyes with no or mild non-proliferative diabetic retinopathy. Diabetics had 89.1% rate of improvement in pre-operative visual acuity.
Statistics
Qualitative data analysis was performed using student’s unpaired t-test. Quantitative data analysis was performed using Chi square test. SPSS Version 17.0 was used for analysis. The p-value less than 0.05 were considered significant.
Spearman rank correlational test was used to assess the relationship between adequate glycemic control, management of diabetic retinopathy and post-operative vision following cataract surgery.
Results
A total of 300 eyes were included in this study, 150 from diabetic and 150 non-diabetic patients. Only 1 eye of each of the diabetic patients was included. Among the 150 diabetics, 21 eyes belonged to type 1 diabetics and 129 eyes from type 2 diabetic patients. There were 114 eyes with mild NPDR, 32 with moderate and 4 with severe NPDR.
The co-morbidities were comparable diseases in both study groups, hypertension being the most commonly associated co-morbidity in the two groups. Over 60% of diabetics with retinopathy changes had hypertension and no other co-morbidities.
Pre-operative glycaemic control was assessed by their glycosylated haemoglobin levels. It was found to be well controlled (HbA1c<7) in 113 patients whereas it was elevated (HbA1c>7) in 37 patients to be operated.
Among the diabetic population, 124 patients (82.6%) were given oral hypoglycaemic agents, 25 patients (16.6%) were on insulin while 1 (0.6%) was only advised diet modification. The age and sex distribution, as well as type of cataract in diabetics and non-diabetics were noted [Table/Fig-1]. IOP was noted in the study population [Table/Fig-2]. The pre-operative BCVA was between 6/24 to 6/60 in majority of eye (203 eyes) [Table/Fig-3].
Intraocular pressure (IOP) in the study population.
| Intraocular pressure range (mmHg) | Number of patients (diabetics) | Number of patients (non-diabetics) |
|---|
| 1-9 | 0 | 0 |
| 10-19 | 148 | 142 |
| 20-40 | 2 | 8 |
Pre-operative visual acuity.
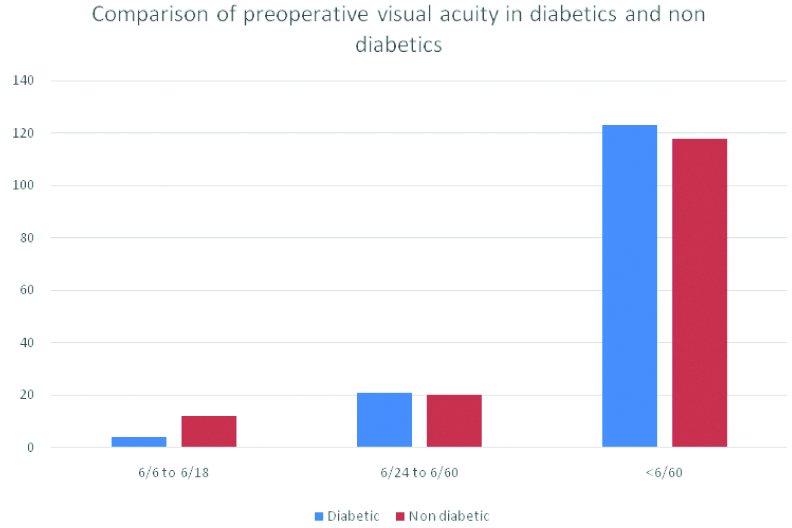
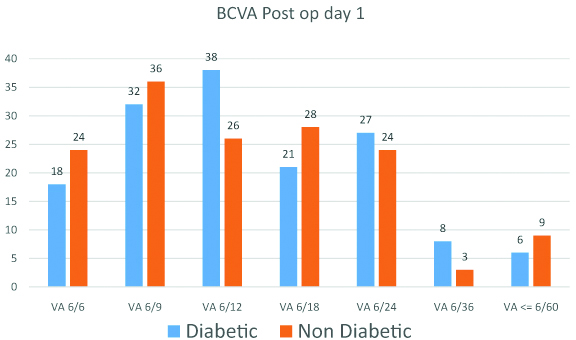
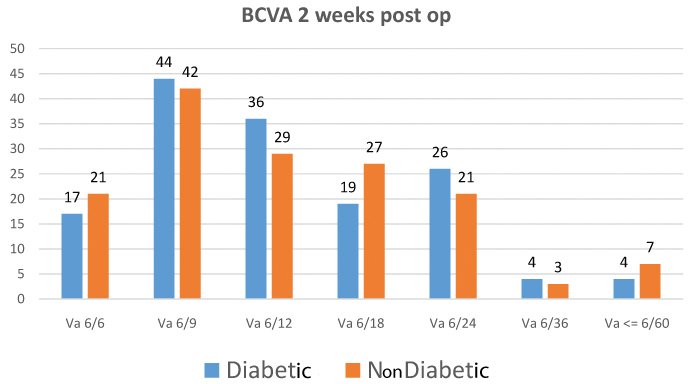
Of the entire study population (N=300), most of the patients (142 among the 150 diabetics and 138 among the 150 non-diabetics) showed improvement of vision post cataract surgery. When compared to pre-operative BCVA status, post-operative BCVA showed significant improvement at the post-operative day 1, 2 weeks and 6 weeks follow-up. (p=0.012) [Table/Fig-4,5 and 6]. BCVA measured two weeks postsurgery was similar to the observed BCVA at the six-week follow-up.
Best Corrected Visual Acuity (BCVA) on post-operative day 1.
Best Corrected Visual Acuity (BCVA) at 2 weeks post-operative.
Best Corrected Visual Acuity (BCVA) at 6 weeks post-operative.
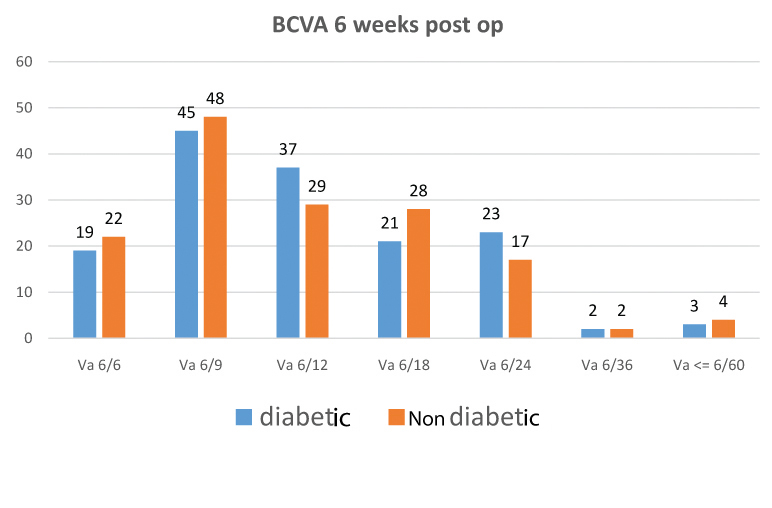
Following cataract surgery, visual acuity at the end of 6 weeks improved in 142 eyes (94.6%), remained the same in 7 (4.5%) and was worse in 1 (0.6%) eye among diabetics while in non-diabetics, visual acuity improved in 138 (92%) and remained stationary 12 (8%) eyes.
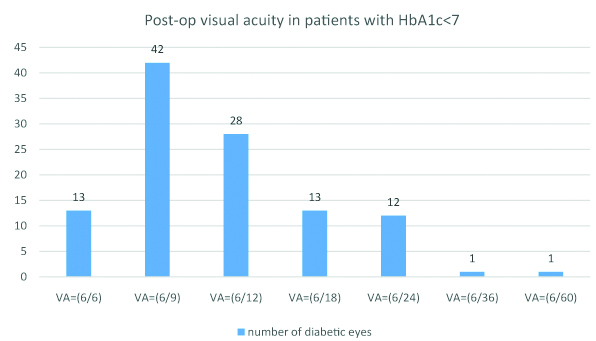
Among the diabetics, uncontrolled baseline glycosylated haemoglobin level was found to be a major offending factor as far as post-op visual recovery was concerned. A total of 55 eyes with low pre-operative glycaemic levels (HbA1c levels less than 7%) showed visual recovery of 6/9 or better [Table/Fig-7].
Post-operative visual acuity in patients who had HbA1c<7.
Complications after cataract surgery were more frequently noted among diabetics; iritis and descemet membrane folds being the most frequent complication, however the difference was not statistically significant (p=0.12) [Table/Fig-8].
Post-operative complications.
| Diabetics | Non Diabetics |
|---|
| Transient Corneal Oedema | 17 | 21 |
| Descemets Membrane Folds | 43 | 37 |
| Hyphaemas | 7 | 5 |
| Iritis | 53 | 61 |
| Misshapen Pupil | 27 | 23 |
| Pigments Deposits on IOL | 9 | 12 |
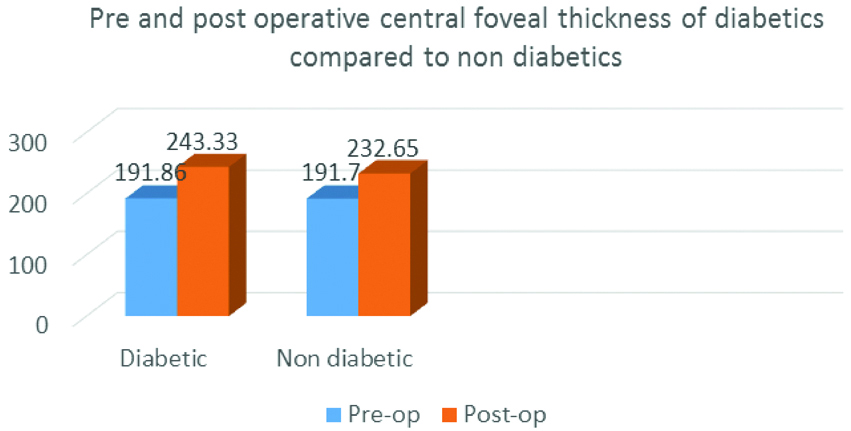
In our study, increase in central foveal thickness was seen in both the groups, 6 weeks after cataract surgery. We observed a minimal average thickening of 51.47 micron among diabetics and 40.95 micron among non-diabetics respectively.
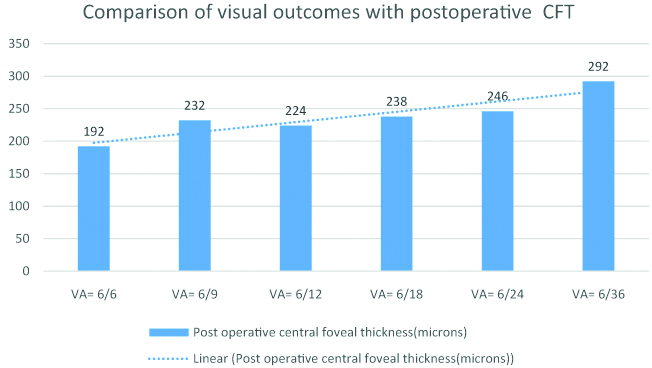
This difference in thickening was compared and was higher among the diabetics, however the data was not significant statistically (p=0.101) [Table/Fig-9]. On further analysis, we found that eyes with higher post-operative CFT were seen to regain lesser post-operative vision when compared to those with CFT in the normal range [Table/Fig-10].
Pre and post operative central foveal thickness (microns).
Comparison of visual outcomes with post-operative central foveal thickness.
Discussion
The sex ratio in our study was male:female (1.6:1), while it was 1.5:1 in the Wisconsin Epidemiologic Study of Diabetic Retinopathy [16]. The higher number of male cohort could be due to low general turn out of female patients to hospitals in this part of the world. Age and sex do not seem to have any influence on the post-operative visual outcomes or complication ratio after surgery in our study.
The average interval between the onset of diabetes and cataract operation was 9.2 years. Most (86%) patients had Type 2 diabetes. Duration of diabetes was directly proportional to the frequency of baseline diabetic retinopathy at presentation. In this study, there were 114 patients with diabetes for 0 to 5 years, 30 patients with diabetes for 6 to 9 years and 6 patients with diabetes for more than 10 years. In the Chennai Urban Rural Epidemiology Study (CURES) Eye Study [17], it has been reported that there is high prevalence of Diabetic Retinopathy (DR) in those with more than 15 years of DM. Some other studies have also shown similar results [18].
Among the diabetic population, 124 patients (82.6%) were given oral hypoglycemic agents, 25 patients (16.6%) were on insulin while 1 (0.6%) was only advised diet modification.
Glycosylated Haemoglobin (HbA1c) being a metabolic marker of diabetic control, its values were correlated with pre-operative diabetic retinopathy status. It was noted that diabetic retinopathy grade was significantly higher in patients with glycosylated haemoglobin >7%, as compared to diabetics with good metabolic control (glycosylated Hb <7%). The immediate pre-operative glycemic control was good (HbA1c <7) in (75.3%) 113, while 24.7% 37cases had HbA1c >7. Many other studies have emphasised on the benefits of good metabolic control by reducing HbA1c levels, in reducing the incidence of complications [12].
Another study reported that the microvascular complication rate decreased by around 25% with improved control of pre-operative glycaemic levels [3]. In Diabetic Control and Complications Trialthe overall risk of retinopathy reduced by around 76% with intensive glucose control in type 1 diabetics. Decelerating the rate of progression of diabetic retinopathy with strict glycaemic control led to decreased morbidity, lesser interventions and better visual outcomes[19].
The present study concluded that diabetic patients regardless of the stage of diabetic retinopathy can expect improved visual outcome following cataract surgery. This holds good for patients with advanced stages of diabetic retinopathy also. The present study population included 300 eyes that underwent cataract surgery. None of the diabetics had proliferative diabetic retinopathy pre-operatively or clinically significant macular oedema at baseline. In our study, post-operative visual improvement was seen in 142 eyes (94.6%), remained stationary in 7 (4.5%) and worsened in 1(0.6%) patient among diabetics whereas visual acuity improved in 138 (92%), remained stationary in 12 (8%) among non-diabetics. Pre-operative visual acuity was directly proportional and diabetic retinopathy stage was inversely proportional to post-operative visual outcomes.
The present study indicated that good visual acuity could be expected after cataract surgery in patients with good pre-operative visual acuity and early stages of diabetic retinopathy.
Previous studies have shown similar results concluding the pre-operative diabetic retinopathy status to be the most important prognostic factor following cataract extraction surgery in diabetics [7,10].
In a similar study, Dowler JG et al., reported that if macular oedema is present at the time of cataract surgery, it would adversely influence post-operative visual outcomes [10], however none of the diabetic patients in this study cohort had macular oedema at the time of cataract surgery; hence this potential correlation could not be studied.
The co-morbidities were comparable diseases in both study groups, hypertension being the most commonly associated co-morbidity in the two groups. Over 60% of diabetics with retinopathy changes had hypertension. Similar results were seen by many other studies among diabetics showing significant association between hypertension and the incidence of diabetic retinopathy [17,18].
Squirrell D et al., found that progression of diabetic retinopathy or macular oedema following cataract surgery were not affected by the diabetic status. In both the study and control groups, the progression of diabetic retinopathy was determined by pre-operative glycaemic control (HbA1c) [7].
In our study, increase in central foveal thickness was seen in both the groups 6 weeks after cataract surgery. We observed a minimal average thickening of 51.47 mm among diabetics and 40.95 mm among non-diabetics respectively. This difference in thickening was correlated and was higher among the diabetics, however the data was not significant statistically (p=0.101).
Hence, based on our results, better visual outcomes can be expected and there is a lower risk of progression of macular oedema post-surgery, therefore surgeons should not hesitate in operating diabetic cataracts, given that untreated macular oedema or proliferative diabetic retinopathy are not present pre-operatively.
Hence, it can be concluded that even though macular oedema is seen following cataract extraction surgery, it can take a benign course and in majority of the patients, onset of diabetic macular oedema after surgery could represent the natural course of the disease itself, and is unlikely to be a direct consequence of the surgery.
Limitation
The limitation of this study was the small sample size and a short period of follow-up. The study could be improved by increasing the duration of follow-up.
Conclusion
Cataract surgery with intraocular lens placement shows good results in diabetics. Good post-operative visual acuity was seen in non-diabetics compared to diabetics. But the difference was not significant statistically throughout the study duration.
Complications after cataract surgery were more frequently noted among diabetics; iritis and descemets membrane folds being the most frequent complication, however the difference was not statistically significant. Poor glycaemic control and preexisting diabetic retinopathy were correlated with a significant decrease of the visual outcomes, accounting for 37% among diabetics, and higher rate of post-operative complications.
Diabetic eyes had a marginally higher increment of central foveal thickness on OCT following cataract extraction surgery, however visual acuity following cataract surgery was found to be at par in diabetics compared to non-diabetics.
To conclude, pre-operative diabetic retinopathy status is a major determinant of post-operative visual recovery. Monitoring post-operative progression of diabetic retinopathy severity after uneventful intraocular lens implantation may enhance visual outcome.