Case Report
A 73-year-old female presented to our rheumatologic clinic, with the complaint of painful Intense swelling in the left parotid region since two years. Cranial nerve assessment was performed and the patient was unable to wrinkle her forehead, close her eye and raise the corner of mouth on the left side. Right sided function was normal. The other parts of the neurological exam revealed no abnormalities. Except for hypertension and hypoparathyroidism, her past medical history was unremarkable. Her drug history since three years ago was positive for propranolol (10 mg, BD), nortriptyline (25 mg, daily), alendronate (70 mg, weekly), levothyroxine (50 mcg, daily) and losartan (50 mg, BD).
She was initially referred to the Ear-Nose-Throat (ENT) department with the same main complaint two years ago. Based on American Society of Anesthesiologists (ASA) criteria, the patient’s operative risk was grade two.
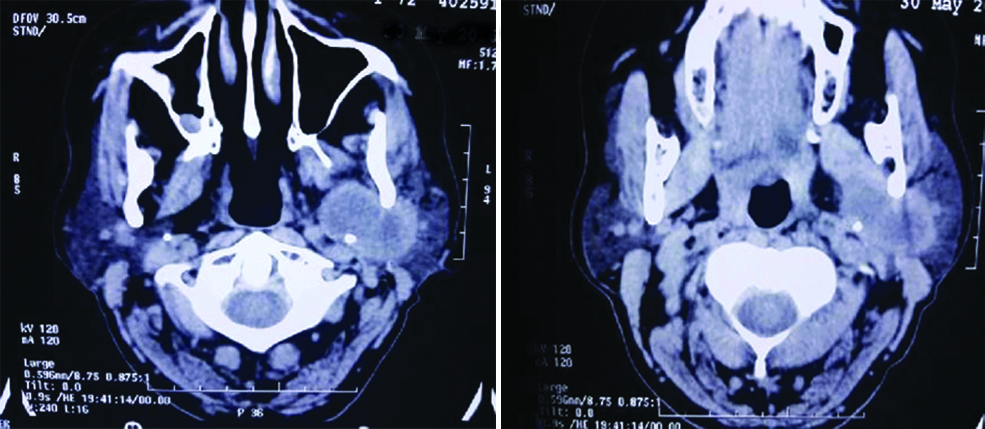
Computed Tomography (CT) scan showed a moderate peripheral enhancing solid mass lesion, measuring 4×3.5 mm in the left parotid gland, with retromandibular and medial extension into deep portion of parotid gland [Table/Fig-1].
CT scan showing a solid mass lesion measuring 4×3.5 mm in the left parotid gland, with retromandibular and medial extension into deep portion of parotid gland.
Resection surgery of the mass and left upper jugular lymph node was performed. Facial nerve function on the postoperative clinical examination was completely normal. The pathological evaluation of resected mass revealed an acute on chronic inflammation with fibrosis and chronic sialadenitis.
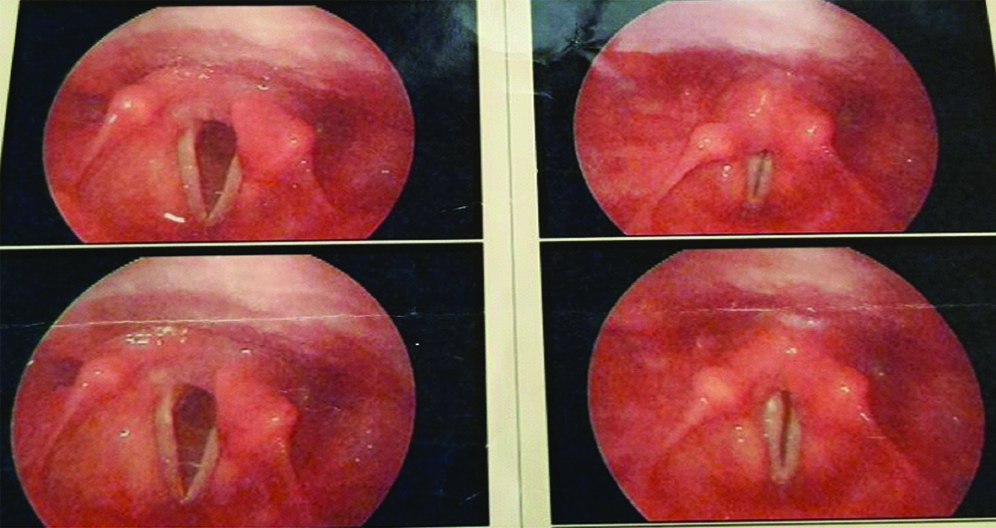
The patient was under observation. One month after the first surgery, she was referred with facial paralysis, hoarseness, dacriocystitis, and a purulent discharge from the surgical site. [Table/Fig-2].
Facial paralysis and a purulent discharge from the surgical site.

Magnetic Resonance Imaging (MRI) of head and neck revealed large ill-defined abnormal intensity component in the site of resected left parotid gland extending massively to left parapharyngeal space with homogeneous enhancement. Brain MRI was normal. The patient returned three months after the initial surgery with a history of frequent food aspiration and bad general condition, and left vocal fold paresis was detected with stroboscopy [Table/Fig-3].
Vocal fold paresis in stroboscopy.
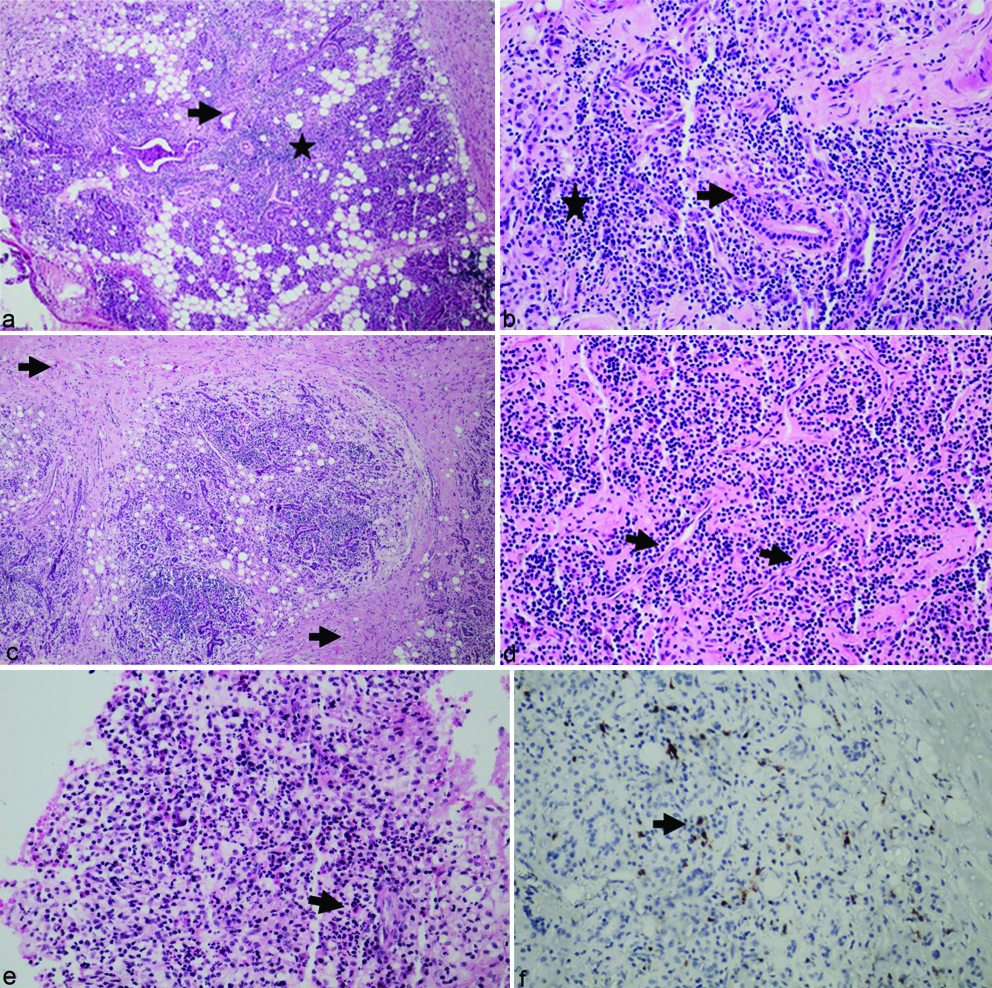
Therefore, spreading of the parotid tumour was suspected and second resection surgery was performed for patient. The surgical pathology report was significant for the chronic inflammatory pseudotumour, with marked fibrosis and eosinophilic microabscess formation. Immunohistochemical staining of the lesion revealed up to 30 IgG4 positive plasma cells in HPF, with IgG4 to IgG positive cell ratio of 40% [Table/Fig-4]. Serum IgG4 level was elevated up to 270 mg/dL. These findings were strongly suggestive for IgG4-RD. Therefore, she was referred to our rheumatology department for further evaluation and management.
(a and b) Histopathologic evaluation showing salivary gland with Lymphoplasmacytic rich infiltration (astrix) and gland destruction, decreased in gland number (black arrow) in comparison with normal salivary gland (magnification x100 in 4a; and X400 in 4b H/E staining); (c) Showing fibrosis (black arrow) in salivary gland (x100 H/E staining); (d) Showing infiltration of few Eosinophil and Phlebitis marked with black arrow (X400 H/E staining); (e) Show Eosinophilic (black arrow) infiltration (X400 H/E stain); (f) IHC examination revealed increased IgG4 positive plasma cells (black arrow) (X400).
First, a thorough physical examination was performed which revealed tenderness and mass at the site of the left parotid gland, dacryocystitis, hoarseness, and left facial nerve palsy. Her laboratory data (Complete Blood Count (CBC), liver function tests, Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP), viral markers, Antinuclear Antibodies (ANA), Rheumatoid Factors (RF), Anti-Neutrophil Cytoplasm Antibodies (ANCAs), Rapid Plasma Regain (RPR), Angiotensin-Converting Enzyme (ACE), Anti-Cyclic Citrullinated Peptide (anti-CCP), and urine analysis were all normal. The patient was treated with prednisolone 60 mg/day and then gradually tapered to 15 mg/day over four months. At the same time, rituximab 500 mg was also administrated weekly for four courses. One week after treatment of her purulent skin discharge, dacryocystitis and tumour-like lesion improved completely. The hoarseness was reduced after three months, but only a partial improvement of facial paralysis was achieved.
Discussion
In this article, we presented a rare case of immunoglobulin G4- related disease (IgG4-RD) with facial and recurrent laryngeal nerve palsies that was successfully treated with corticosteroids and rituximab. IgG4-RD is a rare immune-mediated disease which may affect any organ and mostly occur in middle-aged and elderly patients, with a male predominance [1]. According to a study conducted in 2010, IgG4-RD is more frequent in Asia [2]. The estimated incidence of 0.2 to 1/100000 in Japan and no available incidence data in occidental countries was reported [3]. The annual incidence of IgG4-RD was estimated at 0.28-1.08/100,000. A prevalence of ~62 patients per million inhabitants were expected in Japan in 2009 [4].
The IgG4-RD usually affects individuals of middle to upper age, with an onset at 50–70 years [5-7] although rare pediatric cases have also been described [8]. Most studies report an overall predilection for the male sex [4-6], especially for IgG4-related pancreatitis with a M:F ratio of 3:7 [9]. However, IgG4-related sialadenitis and dacryoadenitis may occur more frequently among females [5].
Although the pathogenesis of the disease is not well-known, pathologic findings include lymphoplasmacytic tissue infiltrations, richness of IgG4-positive plasma cells and lymphocytes, storiform fibrosis, obliterative phlebitis and tissue eosinophilia and IgG4 specific staining [10]. Serum IgG4 levels are elevated in the majority of cases [1,11]. Measurement of IgG4 level is necessary but it is not diagnostic [11], and confirmation of the diagnosis with biopsy is important to exclude malignancy and other disorders that may have the same signs as IgG4-RD. Diagnostic criteria for IgG4-RD are as follows: 1) serum IgG4 concentration >135 mg/dL; and (2) >40% of IgG+ plasma cells being IgG4+ and >10 cells/high powered field of biopsy sample [12]. In our case, the diagnosis was confirmed by biopsy and exclusion of malignancy and other disorders that may mimic IgG4-RD.
The disease usually presents as psudotumour or tumefactive lesions predominantly seen in head and neck segments. Major salivary and lacrimal glands are commonly involved in IgG4-RD [13]. Similar to our study, successful regression of parotid mass and dacryoadenitis following treatment was reported in some previous studies [13,14]. Kakuchi Y et al., described a 60-year-old man with swollen parotid and lacrimal glands and itchy cutaneous nodules who was later diagnosed with IgG4-RD [14]. Prompt improvement after administration of oral prednisolone 20 mg/day was observed. However, the symptoms deteriorated following steroid tapering and improved again with increasing the dosage [14].
Although neurological involvement in IgG4-RD is rare, both central and peripheral nervous systems can be involved [15]. Hypertrophic pachymeningitis and hypophysitis are the most common manifestations of CNS involvement in these patients [16,17]. Cranial nerve palsies are the extremely rare presentation of IgG4-RD reported only in few previous cases [18,19]. Wick CC et al., reported a 61-year-old female with IgG4-RD with right middle ear mass and multiple cranial nerves (II, VI, and VII) involvement. High dose intravenous dexamethasone was initiated and the patient was discharged with prednisone 40 mg daily [18]. Complete improvement of facial weakness and significant recovery of optic nerve palsy was observed [18].
To the best of our knowledge, this is the first case of IgG4-RD with simultaneous facial and recurrent laryngeal nerves palsies reported. The causes of recurrent laryngeal nerve palsy are the tumours of the base of the skull, neck and thorax that cause tumours (both cancerous and non-cancerous) to grow around the nerves and compress them, leading to various forms of paralysis [20]. In our case, unilateral vocal fold paralysis has occurred due to dysfunction of the recurrent laryngeal nerve as well as due to, the mass compression effect leading to hoarseness.
There is no agreement on the ideal treatment associated with IgG4. Because of its rarity, treatment of neurological disease secondary to IgG4-RD is based on available evidence and result of previous articles. In accordance with International Consensus Statement on the treatment of IgG4-RD, all symptomatic patients require treatment [21]. So, we started administration of oral prednisolone for induction for one month, and then this dose was gradually tapered. Our patient required prolong treatment with glucocorticoid, while it was expensive, azathioprine was administrated as glucocorticoid-sparing therapy. Symptoms of the disease in patient decreased but hoarseness and facial paralysis were not completely recovered.
In any patient with organ-threatening or refractory disease or whom treatment with immunomodulatory drugs was unsuccessful, treatment with rituximab is recommended [22]. In our case, treatment with rituximab began and its first dose led to a decrease in her symptoms. The prolonged interval between initiation of neurological signs and diagnosis seemed to have created permanent complications that were resistant to conventional treatments.
Conclusion
In this case report, we introduced other possible complications of IgG4-RD. Practitioners should be aware of challenging manifestations of the disease such as cranial nerve palsies. A novel treatment approach applied in this case may guide future researchers to develop consensus guidelines for successful management of IgG4-RD.
Ethical Approval
All procedures conducted in this study were in accordance with the ethical standards of research committee of Tehran University of Medical Sciences.
Informed Consent
Informed consent was obtained from the patient participated in the study. Written permission from the patient was taken for publication of this work with her photo.
Authors Contribution
MR made substantial contributions to conception and design, and/or acquisition of data, and/or analysis and interpretation of data; SA participated in drafting the article or revising it critically for important intellectual content; and SA gave the final approval of the version to be submitted and any revised version.
[1]. Chen G, Cheuk W, Chan JK, IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entityChinese Journal of Pathology 2010 39(12):851-68. [Google Scholar]
[2]. Nishioka H, Shibuya M, Haraoka J, Immunohistochemical study for IgG4-positive plasmacytes in pituitary inflammatory lesionsEndocrine Pathology 2010 21(4):236-41.10.1007/s12022-010-9128-520635226 [Google Scholar] [CrossRef] [PubMed]
[3]. Palazzo E, Palazzo C, Palazzo M, IgG4-related diseaseJoint Bone Spine 2014 81(1):27-31.10.1016/j.jbspin.2013.06.00123849464 [Google Scholar] [CrossRef] [PubMed]
[4]. Uchida K, Masamune A, Shimosegawa T, Okazaki K, Prevalence of IgG4-related disease in Japan based on Nationwide Survey in 2009Int J Rheumatol 2012 2012:35837110.1155/2012/35837122899936 [Google Scholar] [CrossRef] [PubMed]
[5]. Inoue D, Yoshida K, Yoneda N, Ozaki K, Matsubara T, Nagai K, IgG4-related disease: dataset of 235 consecutive patientsMedicine (Baltimore) 2015 94(15):e68010.1097/MD.000000000000068025881845 [Google Scholar] [CrossRef] [PubMed]
[6]. Brito-Zerón P, Ramos-Casals M, Bosch X, Stone JH, The clinical spectrum of IgG4-related diseaseAutoimmun Rev 2014 13(12):1203-10.[PubMed]10.1016/j.autrev.2014.08.01325151972 [Google Scholar] [CrossRef] [PubMed]
[7]. Wallace ZS, Deshpande V, Mattoo H, Mahajan VS, Kulikova M, Pillai S, IgG4-related disease: clinical and laboratory features in one hundred twenty-five patientsArthritis Rheumatol 2015 67(9):2466-75.10.1002/art.3920525988916 [Google Scholar] [CrossRef] [PubMed]
[8]. Griepentrog GJ, Vickers RW, Karesh JW, Azari AA, Albert DM, Bukat CN, A clinicopathologic case study of two patients with pediatric orbital IgG4-related diseaseOrbit 2013 32(6):389-91.10.3109/01676830.2013.82289923957841 [Google Scholar] [CrossRef] [PubMed]
[9]. Kanno A, Nishimori I, Masamune A, Kikuta K, Hirota M, Kuriyama S, Tsuji I, Research Committee on Intractable Diseases of Pancreas Nationwide epidemiological survey of autoimmune pancreatitis in JapanPancreas 2012 41(6):835-39.10.1097/MPA.0b013e3182480c9922466167 [Google Scholar] [CrossRef] [PubMed]
[10]. Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, Consensus statement on the pathology of IgG4-related diseaseModern Pathology: An Official Journal of The United States and Canadian Academy of Pathology, Inc 2012 25(9):1181-92.10.1038/modpathol.2012.7222596100 [Google Scholar] [CrossRef] [PubMed]
[11]. Carruthers MN, Khosroshahi A, Augustin T, Deshpande V, Stone JH, The diagnostic utility of serum IgG4 concentrations in IgG4-related diseaseAnnals of the Rheumatic Diseases 2015 74(1):14-18.10.1136/annrheumdis-2013-20490724651618 [Google Scholar] [CrossRef] [PubMed]
[12]. Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011Modern Rheumatology 2012 22(1):21-30.10.3109/s10165-011-0571-z22218969 [Google Scholar] [CrossRef] [PubMed]
[13]. Geyer JT, Deshpande V, IgG4-associated sialadenitisCurrent Opinion in Rheumatology 2011 23(1):95-101.10.1097/BOR.0b013e328341301121124091 [Google Scholar] [CrossRef] [PubMed]
[14]. Kakuchi Y, Yamada K, Suzuki Y, Ito N, Yagi K, Matsumura M, IgG4-related skin lesions in a patient with IgG4-related chronic sclerosing dacryoadenitis and sialoadenitisInternal Medicine (Tokyo, Japan) 2011 50(14):1465-69.10.2169/internalmedicine.50.523921757831 [Google Scholar] [CrossRef] [PubMed]
[15]. Baptista B, Casian A, Gunawardena H, D’Cruz D, Rice CM, Neurological Manifestations of IgG4-Related DiseaseCurrent Treatment Options in Neurology 2017 19(4):1410.1007/s11940-017-0450-928374231 [Google Scholar] [CrossRef] [PubMed]
[16]. Shimatsu A, Oki Y, Fujisawa I, Sano T, Pituitary and stalk lesions (infundibulo-hypophysitis) associated with immunoglobulin G4-related systemic disease: an emerging clinical entityEndocrine Journal 2009 56(9):1033-41.10.1507/endocrj.K09E-27719926920 [Google Scholar] [CrossRef] [PubMed]
[17]. Campochiaro C, Ramirez GA, Bozzolo EP, Lanzillotta M, Berti A, Baldissera E, IgG4-related disease in Italy: clinical features and outcomes of a large cohort of patientsScandinavian Journal of Rheumatology 2016 45(2):135-45.10.3109/03009742.2015.105579626398142 [Google Scholar] [CrossRef] [PubMed]
[18]. Wick CC, Zachariah J, Manjila S, Brown WC, Malla P, Katirji B, IgG4-related disease causing facial nerve and optic nerve palsies: Case report and literature reviewAmerican Journal of Otolaryngology 2016 37(6):567-71.10.1016/j.amjoto.2016.08.00527609186 [Google Scholar] [CrossRef] [PubMed]
[19]. Takahashi Y, Kitamura A, Kakizaki H, Bilateral optic nerve involvement in immunoglobulin G4-related ophthalmic diseaseJournal of neuro-ophthalmology: the official journal of the North American Neuro-Ophthalmology Society 2014 34(1):16-19.10.1097/WNO.0b013e3182a304f424531317 [Google Scholar] [CrossRef] [PubMed]
[20]. Mendez Garrido S, Ocete Perez RF, Causes and imaging manifestations of paralysis of the recurrent laryngeal nerveRadiologia 2016 58(3):225-34.10.1016/j.rx.2016.02.00827066920 [Google Scholar] [CrossRef] [PubMed]
[21]. Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, International Consensus Guidance Statement on the Management and Treatment of IgG4-Related DiseaseArthritis & rheumatology (Hoboken, NJ) 2015 67(7):1688-99.10.1002/art.3913225809420 [Google Scholar] [CrossRef] [PubMed]
[22]. Sandanayake NS, Church NI, Chapman MH, Johnson GJ, Dhar DK, Amin Z, Presentation and management of post-treatment relapse in autoimmune pancreatitis/immunoglobulin G4-associated cholangitisClinical Gastroenterology and Hepatology 2009 7(10):1089-96.10.1016/j.cgh.2009.03.02119345283 [Google Scholar] [CrossRef] [PubMed]