Primary Squamous Cell Carcinoma of the Renal Pelvis: Unexpected Diagnosis of an Uncommon Malignancy- A Case Report
Matteo Ferrari1, Jessica Barizzi2, Julien Renard3
1 Clinic of Urology, Regional Hospital of Bellinzona, Ente Ospedaliero Cantonale, Bellinzona, Switzerland.
2 MD, Cantonal Institute of Pathology, Locarno, Switzerland.
3 Clinic of Urology, Regional Hospital of Bellinzona, Ente Ospedaliero Cantonale, Bellinzona, Switzerland; Division of Urology, University Hospital Geneva, Geneva, Switzerland.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Matteo Ferrari, Regional Hospital of Bellinzona, Via Ospedale-6500, Bellinzona, Switzerland.
E-mail: matteo.ferrari@eoc.ch
Squamous Cell Carcinoma (SCC) of the renal pelvis represents a rare malignancy associated with nephrolithiasis. The aim of this report is to describe an unexpected diagnosis of renal pelvis SCC. We report a case of an 82-year-old female who came to our attention for onset of hematuria and left flank pain. A computed tomography scan showed a mass of 8×7 cm involving the middle and upper third of the left kidney associated with hilar lymphadenopathy. Patient underwent radical nephrectomy with para-aortic lymphadenectomy. Histopathological examination of the kidney showed a SCC arising from the renal pelvis, involving the renal parenchyma and perirenal fat, with emboli in the renal vein and lymph node invasion. No postoperative surgical complications were recorded and at follow-up no signs of clinical recurrence were found. However, the patient’s clinical condition declined progressively until death occurred three months later. In addition to being a very rare entity, this case demonstrates that renal pelvis SCC can also develop in the absence of predisposing risk factors. Moreover, renal pelvis SCC has no specific clinical presentation and often being diagnosed at an advanced stage.
Hydronephrosis, Kidney, Squamocellular cancer
Case Report
An 82-year-old lady presented with persistent hematuria and left flank pain. Medical history included chronic renal failure, cerebrovascular disease, coronary artery bypass, aortic valve prosthesis placement and metabolic syndrome including diabetes, obesity (body mass index 30 kg/m2), hyperlipidemia and hypertension. Urological history was unremarkable. Blood tests showed anemia (8.5 g/L) and hypercalcaemia (2.75 mmol/L), treated with blood transfusion and pamidronic acid. Urine cytology was negative for malignancy.
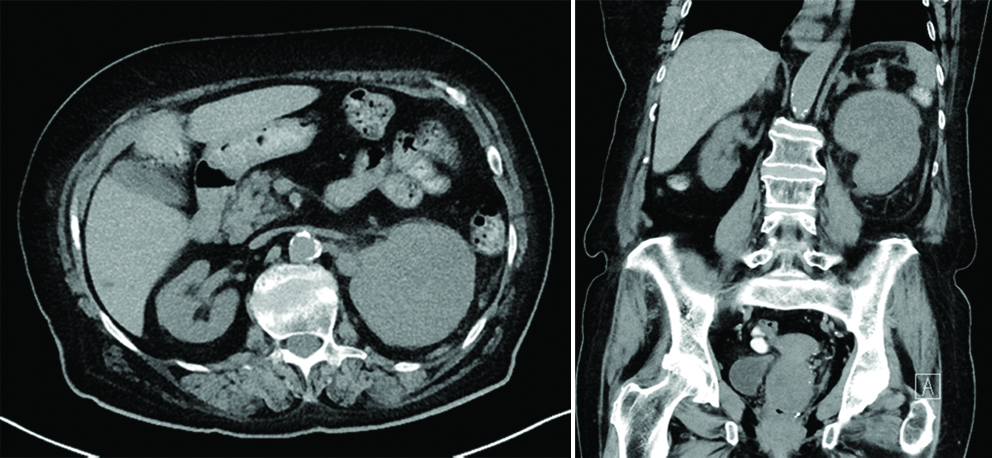
A Computed Tomography (CT) scan showed a mass of 8x7 cm involving the middle and upper third of the left kidney associated with hilar lymphadenopathy. Magnetic resonance imaging and ecocolor doppler test showed patency of the renal arteries, inferior cava and portal veins. There were no metastatic lesions in abdomen; thorax and bone scan [Table/Fig-1,2].
Axial (1) and coronal (2) Computed Tomography (CT) image showing the large mass involving the left kidney.
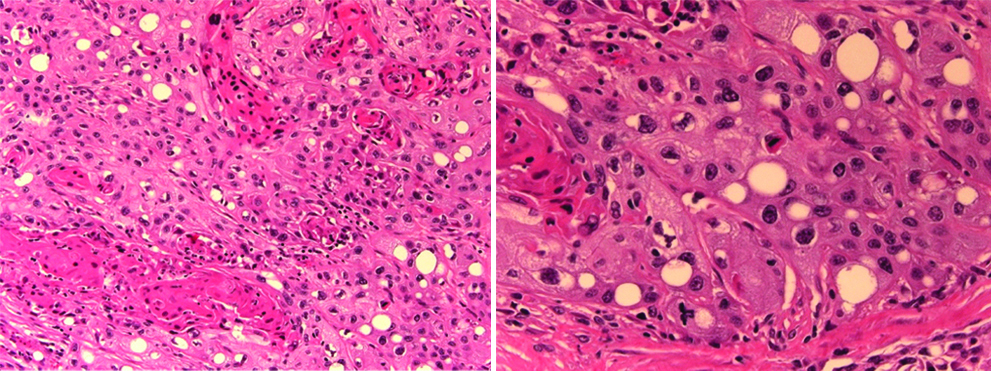
Patient underwent left radical nephrectomy with para-aortic lymphadenectomy through a left subcostal lumbar approach. On gross examination, the kidney showed a solid and yellowish mass with grayish necrotic areas (measuring 10×9×7 cm) which involved the adipose tissue of the renal pelvis and the perirenal fat. The renal vein showed intraluminal neoplastic emboli. Histologically, the neoplasm was described as pure squamous cell phenotype and displayed a wide range of differentiation, from well differentiated areas with keratinisation, prominent intercellular bridges and minimal nucleocytoplasmic atypia, to moderately differentiated areas with moderate nucleocytoplasmic atypia and only focal evidence of squamous differentiation [Table/Fig-3,4].
3) Microscopic images of invasive squamous cell carcinoma moderately differentiated with keratinisation areas (H and E, 20x). 4) High magnification (H and E, 40x) showing cells with moderate nucleo-cytoplasmic atypia, keratinisation areas, dyskeratocyte and atypical mitosis figure.
The definitive histologic diagnosis was locally advanced SCC of renal pelvis, metastatic to the ipsilateral adrenal and multiple para-aortic lymph nodes. No postoperative surgical complications were recorded and renal function remained unaltered without the need for dialysis. At follow-up, no signs of clinical recurrence were found. However, the patient’s clinical condition declined progressively until death occurred three months later for causes not related to urological malignancy.
Discussion
Tumours of the upper urinary tract are the least common of renal tumours. Among these tumours, Squamous Cell Carcinoma (SCC) of the renal pelvis represents a rare histological entity [1]. This malignancy is very aggressive and associated with a poor prognosis [1]. The main recognised risk factor in the few case reported in literature is nephrolithiasis [2]. The aim of this report is to describe an unexpected diagnosis of renal pelvis SCC.
Among upper urinary tract tumours, SCC of the renal pelvis is a rare variant accounting for 10% of all pyelocaliceal tumours, with a six times lower incidence in the ureter [1]. SCC diagnosis is generally reported in older adults and its aetiology has been recognised in a condition of chronic inflammation that leads to a squamous metaplasia of urothelial cells [2]. The development of SCC has been shown to be strongly associated with chronic inflammatory and chronic bacterial infection diseases of renal pelvis arising from urolithiasis and obstruction [2]. This has led some authors to propose preventive lithiasis treatment or periodic urine cytology, contrast imaging and biopsy if needed to rule out SCC in chronic nephrolithiasis patients for early detection [3].
An increased risk for induction of squamous metaplasia and consequent carcinoma seems to be derived from exposure to cyclophosphamide and alkylating agents, from vitamin A deficiency and hormonal imbalance [4].
The case reported appears unrelated to the recognised aetiological factors mentioned. Our patient did not have any history of urolithiasis or pyelonephritis. Preoperative imaging did not show renal calculi and urine culture was negative. The family history did not include other cases of carcinoma of the urinary tract and the patient had not been apparently in contact with recognised carcinogenic substances associated with SCC nor presented signs of vitamin A deficiency. The only habit of interest was the patient being a smoker.
In the literature, few other cases of renal pelvis SCC not associated with recognised risk factors have been described [5,6]. Our case may confirm the need for further studies on pathogenic processes and unknown risk factors that determine the development of this rare and aggressive histological variant.
The only laboratory abnormalities were anemia due to hematuria and hypercalcaemia, the latter being a sign of paraneoplastic syndrome that may be associated with SCC as reported in other cases [3]. Cytological examination of the urine was negative indicating the limited diagnostic specificity of this test.
An important limitation for our patient was the impossibility to perform a contrast examination because of severe renal insufficiency; the size of the mass found on the basal CT scan, among the largest reported in renal pelvis SCC literature [5] were at least indicative of the neoplastic nature of the lesion. Lee TY et al., described a different prognosis of SCC according to tumour location in the renal pelvis, worse in the case of tumours of central origin; in our case the dimensions and the invasiveness make it difficult to establish its origin based on this classification [7].
Histopathological analysis revealed high grade SCC involving the renal parenchyma, the perirenal fat and the adrenal gland with vascular invasion and lymph nodes metastasis. All these histological parameters are associated with a negative prognosis [2].
To date, surgery is the only viable option in patients with renal pelvis SCC, despite poor oncologic outcome [2]. A retrospective study, Makino T et al., reported that median survival was much shorter for surgically treated patients with SCC compared to those with urothelial carcinoma (7 vs 50 months) and the execution of a cisplatin-based neo-adjuvant chemotherapy (although not feasible in our case) showed no significant differences in clinical specific survival rates [8].
Conclusion
In addition to being a very rare entity, this case demonstrates that renal pelvis SCC can grow also in the absence of predisposing risk factors. Moreover, renal pelvis SCC confirms not having a specific presentation and often being diagnosed at an advanced stage. Although the poor oncologic outcome. Radical surgery remains the foremost treatment, not only for diagnosis but also for palliative control of symptoms, as alternative treatment options are of limited efficacy.
Declarations: Ethics approval and consent to participate: Data collection was done following the principles outlined in the Declaration of Helsinki.
Authors’ contributions: M.F. and J.R. analysed and interpreted the patient data and were the major contributors in writing the manuscript. J.B. performed the histological examination. All authors read and approved the final manuscript.
[1]. Busby JE, Brown GA, Tamboli P, Kamat AM, Dinney CP, Grossman HB, Upper urinary tract tumours with nontransitional histology: a single-center experienceUrology 2006 67:518-23.10.1016/j.urology.2005.09.01016527570 [Google Scholar] [CrossRef] [PubMed]
[2]. Bhaijee F, Squamous cell carcinoma of the renal pelvisAnn Diagn Pathol 2012 16:124-27.10.1016/j.anndiagpath.2011.08.00922192451 [Google Scholar] [CrossRef] [PubMed]
[3]. Nachiappan M, Litake MM, Paravatraj VG, Sharma N, Narasimhan A, Squamous cell carcinoma of the renalpelvis; a raresite for a commonly known malignancyJ Clin Diagn Res 2016 10:4-6.10.7860/JCDR/2016/17846.708126894122 [Google Scholar] [CrossRef] [PubMed]
[4]. Tyagi N, Sharma S, Tyagi SP, Maheshwari V, Nath P, Ashraf SM, A histomorphologic and ultrastructural study of the malignant tumours of the renal pelvisJ Postgrad Med 1993 39:197-201. [Google Scholar]
[5]. Attalla K, Haines K, Labow D, Mehrazin R, Squamous cell carcinoma of the renal pelvis: atypical presentation of a rare malignancyUrology Case Reports 2017 13:137-39.10.1016/j.eucr.2017.04.00728567328 [Google Scholar] [CrossRef] [PubMed]
[6]. Bandyopadhyay R, Biswas S, Nag D, Ghosh AK, Squamous cell carcinoma of the renal pelvis presenting as hydronephrosisJ Cancer Res Ther 2010 6:537-39.10.4103/0973-1482.7706021358095 [Google Scholar] [CrossRef] [PubMed]
[7]. Lee TY, Ko SF, Wan YL, Cheng YF, Yang BY, Huang DL, Renal squamous cell carcinoma: CT findings and clinical significanceAbdom Imaging 1998 23:203-8.10.1007/s0026199003249516518 [Google Scholar] [CrossRef] [PubMed]
[8]. Makino T, Izumi K, Natsagdorj A, Iwamoto H, Kadomoto S, Naito R, Significance of perioperative chemotherapy in squamous cell carcinoma of the upper and lower urinary tractAnticancer Res 2018 38:2241-45.10.21873/anticanres.12467 [Google Scholar] [CrossRef]