Supraclavicular brachial plexus blockade is an effective and reliable alternative to general anaesthesia for upper arm surgeries with minimal side-effects [1,2]. The brachial plexus is formed by the ventral rami of C5-T1, occasionally with small contributions by C4 and T2 [3]. Ultrasound provides more success and decreases tissue injury. It also decreases the anaesthetic volume and systemic toxicity. It helps for better visualisation and localisation of brachial plexus [4-6].
Various adjuvants with local anaesthetic agents decrease onset of time and prolong the duration of peripheral nerve blocks. Bupivacaine is a long-acting local anaesthetic, which decreases pain by inhibiting the transmission of pain signals to dorsal horn of the spinal cord. Bupivacaine inhibits the sodium influx by binding with sodium channels and thus nerve depolarization is blocked [7]. Opioids blocks nociception at the spinal cord and central nervous system level. Opioids depress neurotransmitter release and hyperpolarise neuronal membranes thus making the neuron less responsive to pain signal [8]. Fentanyl, a μ-opioid receptor agonist used for pain controls with other anaesthetic medications, which is associated with side-effects like nausea, vomiting, constipation, dry mouth [9].
Nalbuphine is a mixed k-agonist and μ-antagonist opioid used as adjuvant to local anaesthetic for various regional anaesthetic techniques due to its affinity to κ-opioid receptors (KOR) to enhance the duration of analgesia [1,10]. Specifically, it acts as a moderate-efficacy formerly classified as μ-opioid (MOP) receptor antagonists and as a high-efficacy partial agonist of the KOR, whereas it has relatively low affinity for the δ-Opioid Receptor (DOR) and sigma receptors. It is extensively studied as an adjuvant to local anaesthetics in central neuraxial techniques by caudal, epidural and intrathecal routes [11]. Nalbuphine, 10 mg and 20 mg of nalbuphine hydrochloride/mL contain 1.26% citric acid anhydrous, 0.94% sodium citrate hydrous, 0.1% sodium metabisulfite, and 0.2% of a 9:1 mixture of methylparaben and propylparaben as preservatives. Nalbuphine has various side effects of Nalbuphine which include nausea, vomiting, dry mouth, headache, dizziness and vertigo. Unlike other opioids, it causes minimal or no respiratory depression [12].
Studies so far conducted were between bupivacaine with fentanyl and normal saline [13]. Similarly, studies have been done between nalbuphine and bupivacaine with normal saline [1]. To the best of authors knowledge, no similar study has been done to compare efficacy of adding fentanyl and nalbuphine as adjuvant with bupivacaine. Therefore, in the present study, authors compared the efficacy of fentanyl and nalbuphine with bupivacaine (0.5%) on onset and duration of sensory and motor block with requirement of analgesia in ultrasound guided supraclavicular brachial plexus block.
Materials and Methods
This prospective double-blind study was performed after obtaining the approval of the Institutional Ethical Committee (ref. code 89th ECM II BThesis/P23) during the period for September, 2017 to August, 2018 in the Department of Anaesthesiology, King George’s Medical University, Lucknow, Uttar Pradesh, India. A total 60 American Society of Anaesthesiologists (ASA) I and II patients of either sex in the age group of 18 to 60 years weighing 50 to 90 kg, undergoing upper limb surgeries (below mid humerus) under Supraclavicular brachial plexus block under USG guidance were included in this study. Sample size was calculated on the basis of alpha error of 0.05 with 80% power and 95% confidence limit. Assuming a 5% drop out rate, total 32 patients enrolled in each group, the final sample size was determined to retain 30 patients in each group. Written informed consent was obtained from each participant. Patients were randomised into two groups (n=30 in each group) using a computer-generated random number table.
Supraclavicular brachial plexus blockade was performed under ultrasound guidance. Group A: Patient received 20 mL of 0.5% bupivacaine with 2 mL (100 μgm) fentanyl and 10 mL normal saline. Group B: Patient received 20 mL of 0.5% bupivacaine with 2 mL (20 mg) nalbuphine and 10 mL normal saline.
A day before surgery, patients were admitted and at least six hours fasting was ensured. The lactated ringer solution was infused (6-8 mL/kg) and intravenous access was established. The non-invasive Electrocardiogram (ECG), heart rate, blood pressure, and pulse oximetry (SpO2) were recorded. A transportable ultrasound system (SonoSite MicroMax; SonoSite Inc., Bothell, WA, USA) was used to perform the supraclavicular brachial plexus block. Images of brachial plexus were obtained in the transverse and longitudinal planes using 38 mm, 8-13 MHz linear High-Frequency Transducer (HFL-38).
All procedures were performed under aseptic conditions. The ultrasound transducer was used to visualise the brachial plexus. Authors used 23-G needle to localise and perform brachial plexus block.
One of the investigators prepared 32 mL of study drug with either 100 microgram fentanyl or 20 mg nalbuphine. The patient received brachial plexus block through supraclavicular approach by an experienced anaesthesiologist who was blinded to the contents of the drug given.
Firstly, authors localised brachial plexus by ultrasound imaging then after negative aspiration and injected 32 mL of drugs to avoid accidental intravascular administration. Authors observed the expansion of brachial plexus sheath as a positive sign of block.
Primary outcome of the study was to evaluate efficacy of fentanyl and nalbuphine with bupivacaine (0.5%) in supraclavicular brachial plexus block. Secondary outcome of the study was to evaluate the haemodynamic stability and side-effects of the drugs.
Pinprick (25-G needle) method was used for assessment of onset of sensory block by 3-point pain scale (0-no pain, 1-blunt pain and 2-sharp pain) and compared it to contralateral arm. Authors considered onset of sensory block from completion of drug injection to loss of pinprick sensation in dermatome (C5-T1). The post-operative analgesia duration was taken as the time between administrations of local anaesthetic and need of first rescue analgesic drug.
Modified Bromage scale was used to assess motor weakness by hand grip and movement at the elbow, wrist, and fingers. Motor block was assessed by thumb adduction (ulnar nerve), thumb abduction (radial nerve) and thumb opposition (median nerve). Duration of motor block was taken from onset of motor block to complete recovery of full muscle power and was determined by asking the patients to note the time when they could first move their fingers of blocked limb. The criteria for quality of block were based on the complaint from the patients: Excellent (Grade 4)=No complaint, Good (Grade 3)=Negligible complaint with no requirement for supplemental analgesics, Moderate (Grade 2)=Complaint, needed supplemental analgesics and Unsuccessful (Grade 1)=General anaesthesia required [14].
Post-operative pain was assessed using 10-point VAS, 0-no pain to 10-worst pain at one hour interval till demand of rescue analgesia (VAS≥3). Injection diclofenac sodium 1 mg/kg intramuscular was administered. Sedation was assessed using Ramsay sedation score. Drugs side-effects such as nausea, vomiting, skin rashes, tachycardia, hypertension and respiratory depression, bradycardia were also recorded.
Statistical Analysis
The data were presented as mean, standard deviation and percentage. The data were analysed using SPSS 15.0. Student’s t-test, chi-square test, and Mann-Whitney U-test were used for statistical analysis. The p-value <0.05 was considered significant.
Results
Demographic characteristics such as age, gender, height and weight were comparable in between Group A and Group B [Table/Fig-1]. The mean age of the selected patients for Group A was 34.13±10.22 years with 60% male while for the patients of Group B the mean age was 34.13±9.28 years with 66.7% males. The mean height and weight patients were 164.80±10.38 cm and 71.33±10.89 kg in Group A and 163.63±9.13 cm and 69.63±9.88 kg Group B, respectively.
Demographic characteristics of the patients.
| Variables | Group A | Group B | p-value |
|---|
| Age (years) | 34.13±10.22 | 34.13±9.28 | 1.00 |
| Height (cm) | 164.80±10.38 | 163.63±9.13 | 0.646 |
| Weight (kg) | 71.33±10.89 | 69.63±9.88 | 0.529 |
| Gender |
| Female | 12 (40.0%) | 10 (33.3%) | 0.592 |
| Male | 18 (60.0%) | 20 (66.7%) | |
| ASA Grade |
| Grade-I | 19 (63.3%) | 18 (60.0%) | 0.791 |
| Grade-II | 11 (36.7%) | 12 (40.0%) | |
| Quality of block |
| Excellent | 22 (73.3%) | 21 (70.0%) | 0.774 |
| Good | 8 (26.7%) | 9 (30.0%) | |
Data are represented as mean±SD, and n (%) SD=Standard deviation
Total 63.3% of patients have ASA Grade I and 36.7% have Grade II in Group A whereas 60.0% and 40.0% in Group B, respectively. The ASA grade was not significantly different in between Group A and Group B [Table/Fig-1].
The quality of block (based on complaint from the patient and need for supplemental analgesics) was excellent in 73.3% of cases of Group A and 70.0% cases of Group B, while the quality was good in 26.7% cases of Group A and 30.0% cases of Group B. No significant difference was found in proportion of various quality levels between the two groups [Table/Fig-1].
The mean onset time of sensory block was 12.07±1.08 minutes and 8.20±1.32 minutes in between Group A and Group B, respectively. The mean duration of sensory block was 466.87±39.84 minutes and 719.23±19.45 minutes in between Group A and Group B, respectively. The onset time of sensory and mean duration of sensory block was significantly different in between Group A and Group B [Table/Fig-2]. The mean onset time of motor block was 16.80±1.27 minutes and 14.03±1.22 in between Group A and Group B, respectively. The mean duration of motor block was 362.20±34.31 minutes and 415.97±16.97 minutes in between Group A and Group B, respectively. The onset time of motor and mean duration of motor block was significantly different in between Group A and Group B [Table/Fig-2]. The mean duration of analgesia was 660.67±31.77 minutes and 836.13±25.74 minutes in between Group A and Group B and the difference was significant statistically [Table/Fig-2].
Block characteristics of supraclavicular brachial plexus block in Group A and Group B.
| Group A | Group B | p-value |
|---|
| Onset of sensory block (minutes) | 12.07±1.08 | 8.20±1.32 | <0.001** |
| Duration of sensory block (minutes) | 466.87±39.84 | 719.23±19.45 | <0.001** |
| Onset of motor block (minutes) | 16.80±1.27 | 14.03±1.22 | <0.001** |
| Duration of motor block (minutes) | 362.20±34.31 | 415.97±16.97 | <0.001** |
| Duration of analgesia (min) | 660.67±31.77 | 836.13±25.74 | <0.001** |
**=Significant (p<0.001)
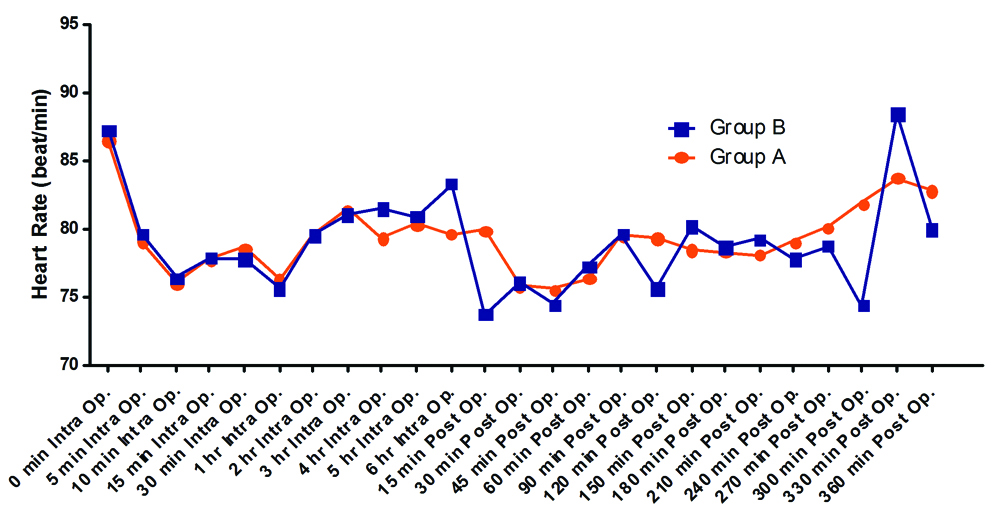
The mean heart rate was not significantly different in between Group A and Group B at baseline. The heart rates were comparable in between Group A and Group B intraoperatively and post-operatively except 15 minutes and 300 minutes [Table/Fig-3].
Heart Rate (beats/minute).
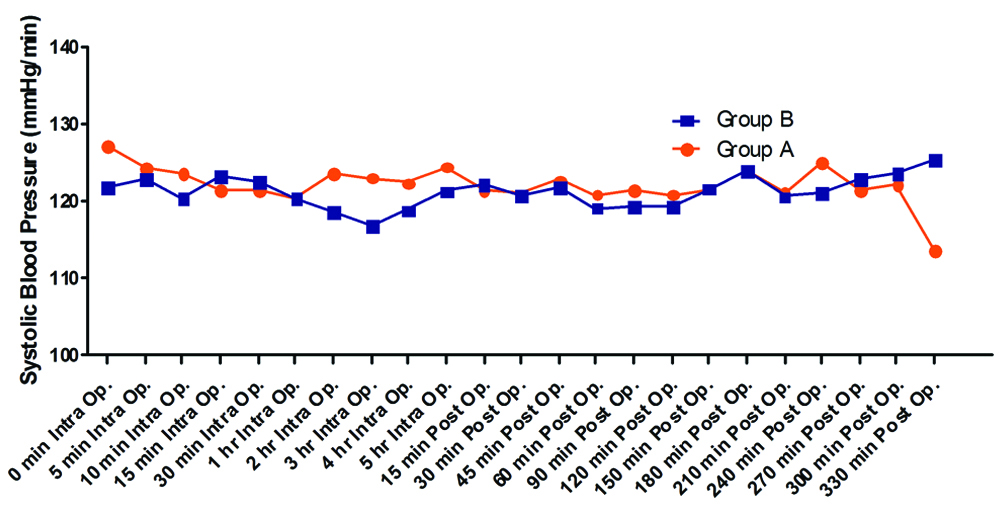
The mean SBP was comparable in between Group A (127.30±12.67 mmHg) and Group B (121.87±13.18 mmHg) at baseline. The mean SBP were not significantly different in between Group A and Group B intraoperatively and postoperatively except at 2 hours, 3 hours and 330 minutes (p<0.05) [Table/Fig-4].
Systolic blood pressure (mmHg).
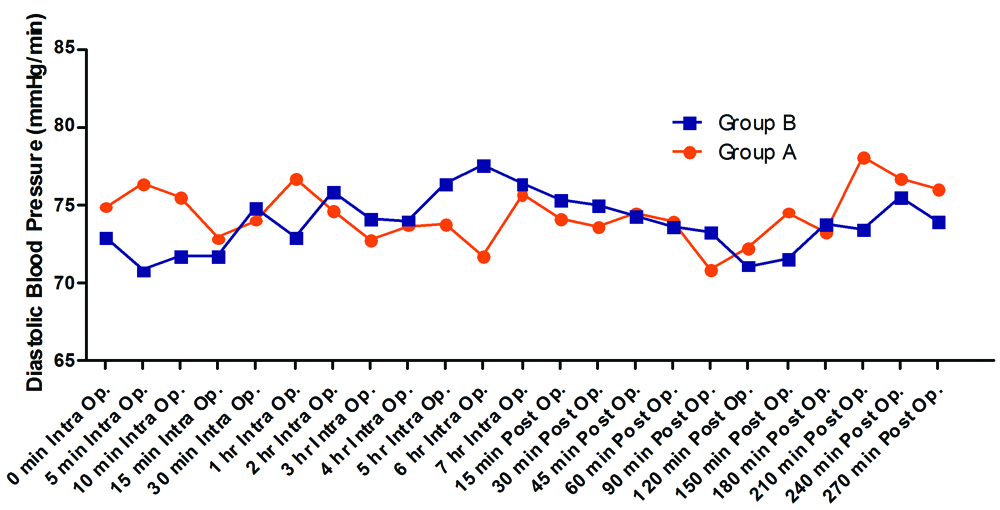
The mean DBP was comparable in between Group A (74.87±10.03 mmHg) and Group B (72.97±8.34 mmHg) at baseline. The mean DBP were not significantly different in between Group A and Group B intraoperatively and postoperatively except 5 minutes, 10 minutes 90 minutes and 210 minutes (p<0.05) [Table/Fig-5].
Diastolic blood pressure (mmHg).
The VAS score were recorded at every hour post-operative in Group A and Group B patients. There was no pain observed in both Group At 1-8 hours. Pain was observed in Group A at nine hours (mean VAS 0.17), 10 hours (mean VAS 2.0), 11 hours (mean VAS 3.63), and 12 hours (mean VAS 4). Whereas, there was no pain observed in Group B at nine hours, 10 hours, 11 hours, and 12 hours (mean VAS 0). The mean VAS score were significantly different at each recorded time after 8 hours (p<0.05). The RSS score were observed at 0 minute to 90 minutes. The mean RSS score (2.0) were found to be similar (p=1.00) in both Group A and Group B at each time interval.
In present study, nausea was found in 3.3% cases of Group A and 10.0% cases of Group B. Vomiting, skin rashes, tachycardia, hypertension and respiratory depression were not found in any case in the two groups [Table/Fig-6]. Bradycardia was found in 3.3% cases of Group A and 10.0% cases of Group B. Hypotension was found in 6.7% cases of group-A and 10.0% cases of Group B. Sedation was found only in 3.3% cases of Group B. The side-effects were not significantly different in between Group A and Group B [Table/Fig-6].
Side-effects in Group A and Group B.
| Side-effects | Group A | Group B | p-value |
|---|
| Nausea | 1 (3.3%) | 3 (10.0%) | 0.301 |
| Vomiting | 0 | 0 | - |
| Skin rashes | 0 | 0 | - |
| Tachycardia | 0 | 0 | - |
| Bradycardia | 1 (3.3%) | 3 (10.0%) | 0.301 |
| Hypotension | 2 (6.7%) | 3 (10.0%) | 0.640 |
| Hypertension | 0 | 0 | - |
| Sedation | 0 | 1 (3.3%) | 0.313 |
| Respiratory depression | 0 | 0 | - |
Discussion
In the present study, authors have compared fentanyl and nalbuphine as adjuvant to bupivacaine in terms of onset of sensory and motor blockade, duration of sensory and motor blockade, and duration of analgesia.
The rationale of choosing 0.5% bupivacaine in the present study for supraclavicular block is supported by Ilham C et al., who found that for supraclavicular brachial plexus block 0.5% bupivacaine leads to faster motor and sensory block onset compared to 0.5% levobupivacaine however similar duration of post-operative analgesia [15].
Authors used fentanyl in dose 100 microgram. This was based on the previous study conducted by Gohiya S and Gohiya VT, in which 100 μg fentanyl with 38 mL 0.5% bupivacaine was compared with control group [16]. Nalbuphine dose of 20 mg was chosen as per recommendation in the textbook as well as previous researches [1].
In the present study, the onset of sensory block was significantly earlier in nalbuphine Group as compared to fentanyl group. Moreover, the onset of motor block was also significantly earlier in nalbuphine Group as compared to fentanyl group. Kaniyil S et al., also found a delay in onset of both sensory and motor blockade on addition of fentanyl to local anaesthetics [17]. This effect could have resulted from slower penetration of nerve membrane by local anaesthetics as a result of the change in pH of the anaesthetic solution. Studies have shown that alkalinization of local anaesthetic agents in nerve block improves onset, quality and duration of analgesia. Nishikawa K et al., concluded that addition of 100 μg of fentanyl resulted in slower onset of analgesia which may be due to decrease in pH of lignocaine from 6.2 to 5.2 [18]. In 2018, Hamed MA et al., conducted a study to compare the effect of fentanyl and normal saline with 0.5% bupivacaine as an adjuvant. In their study, the onset of the sensory block time was (11.8±3.3 minutes) in fentanyl group whereas it was (16.3±4.8 minutes) in control group [19]. Also, the motor block onset time was (13.7±3.3 minutes) in fentanyl group whereas it was (18.4±5.2 minutes) in control group which is comparable to the present study. Gupta K et al., Nazir N and Jain S, and Das A et al., reported that the use of nalbuphine caused early onset of sensory and motor block as intrathecal fentanyl for orthopaedic surgery of lower limbs under subarachnoid block [1,20,21]. Similarly, Abdelhaq MM et al., reported that the adding of 20 mg nalbuphine to bupivacaine in supraclavicular brachial plexus block results in early onset of sensory block (8.64±0.717 minutes) and also early onset in motor block (17.4±1.14 minutes) as compared to control group [22].
In the present study, authors found that duration of sensory block and motor block were significantly higher in nalbuphine group as compared to fentanyl group. Moreover, the duration of analgesia was higher in nalbuphine group as compared to fentanyl group. The present results are supported by similar findings of previous studies by Hamed MA et al., and Chavan SG et al., who found that the duration of sensory block and motor block in fentanyl group which was significantly longer than control [19,13]. Marashi SM et al., added 100 μg fentanyl to 30 mL bupivacaine for supraclavicular brachial plexus block and showed the duration of sensory block (11.3±1.7 hours) and motor block (4.56±1.0 hours) in control group where as duration of sensory block was (12.8±3.3 hours) and motor block (5.1±2.0 hours) in fentanyl group which is similar to the present study [23]. The present findings are supported by the studies of Hamed MA et al., Nazir N and Jain S, Das A et al., and Abdelhaq MM et al., who reported that the nalbuphine as adjuvant to bupivacaine for supraclavicular brachial plexus block prolongs the duration of sensory block and motor block (412.59±8.63 minutes) as well as duration of analgesia [19-22].
Gupta K et al., also showed that addition of nalbuphine to bupivacaine increases the duration of sensory and motor blockade, and also duration of analgesia [1]. The addition of nalbuphine to hyperbaric bupivacaine prolongs the duration of analgesia as compared to fentanyl with hyperbaric bupivacaine in caesarian section [24,25].
In the present study, the decline in heart rate was observed during intraoperative period and post-operative period from its baseline values at all the periods of observation in both groups. However, the decline in heart rate was not found to be statistically significant. Similarly, Chavan SG et al., and Hamed MA et al., observed that the heart rate was lower in fentanyl group but the difference was not statistically significant [13,19]. In their study, bradycardia and hypotension were observed but not significantly different. Incidence of nausea and vomiting were recorded in fentanyl group. In this study, the SBP and DBP were found to be lower than its baseline at all the periods of observation in both groups. However, in both the groups the changes were not found to be statistically significant at any period of observation. Mukherjee A et al., administered nalbuphine intrathecally for orthopedic surgery and found that few side-effects such as nausea, hypotension and bradycardia were exclusively associated with the highest dose of nalbuphine (0.8 mg/kg body weight) [26].
In the present study, sedation in one patient was observed in nalbuphine group whereas no sedation was observed in fentanyl group. The present study is supported by Chiruvella S et al., who explained sedation by nalbuphine on the basis of some amount of systemic absorption of drugs [27]. Das A et al., also showed the sedative-effect of nalbuphine in their study [21].
In present study, the side-effects were not found to be statistically significant between groups. In spite of findings that fentanyl causes less side-effects, authors would like to suggest that nalbuphine is better alternative as compared to fentanyl with local anaesthetics in peripheral nerve blocks. It also hastens onset of block and prolongs duration of block with clinically manageable minimal side-effects like bradycardia and hypotension.
Limitation
The present study was single-centric, a not multi-centric study should be conducted in future. The ultrasound guided block could have significantly decreased the total volume of the local anaesthetics.
Conclusion
Authors found that nalbuphine 20 mg is a better adjuvant as compared to fentanyl 100 μgm with bupivacaine 0.5% in supraclavicular brachial plexus block as it hastens onset time and increases the duration of sensory and motor blocks. It also delays time for rescue analgesic requirement in post-operative period. There was no major complications with both drugs but nalbuphine was associated with slightly more side-effects as compared to fentanyl mainly bradycardia and hypotension.
Data are represented as mean±SD, and n (%) SD=Standard deviation
**=Significant (p<0.001)