Therapy Related Acute Promyelocytic Leukaemia (APML) in a Breast Cancer Survivor: Another Tale of an Ally Turned Adversary
Sujaya Mazumder1, Debdatta Basu2, Biswajit Dubashi3
1 Senior Resident, Department of Pathology, JIPMER, Puducherry, India.
2 Professor, Department of Pathology, JIPMER, Puducherry, India.
3 Professor, Department of Medical Oncology, JIPMER, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sujaya Mazumder, C12, Sreenivasa Towers, Oulgaret, Puducherry-506010, India.
E-mail: suji0206@gmail.com
With an increase in the use of high dose chemotherapeutic regimens, higher cure rates and longer survival periods of cancer patients, the incidence of secondary malignancies are increasing. Therapy related Myeloid Neoplasm (t-MN) is a second malignancy after chemotherapy/radiotherapy given for a prior malignancy. Of the various t-MN Acute Promyelocytic Leukaemia (APML) as a complication of chemo-radiotherapy is very rare. We report a rare case of therapy related APML in a breast cancer survivor.
Secondary, Topoisomerase II inhibitor, Therapy related myeloid neoplasm
Case Report
A 62-year-old lady, presented to our hospital in November 2015 with a lump in the right breast. She was diagnosed as Grade II, Hormonal receptor positive- Infiltrating Ductal carcinoma and was treated with right modified radical mastectomy with a pathological staging of pT2N1aMx. She subsequently received adjuvant chemotherapy containing three cycles of FEC regimen (5-Flurouracil, Epirubicin, Cyclophosphamide) with four cycles of Injection Docetaxel followed by Letrozole therapy. Patient was under regular follow-up during her treatment and her routine blood investigations during the same were within normal limits.
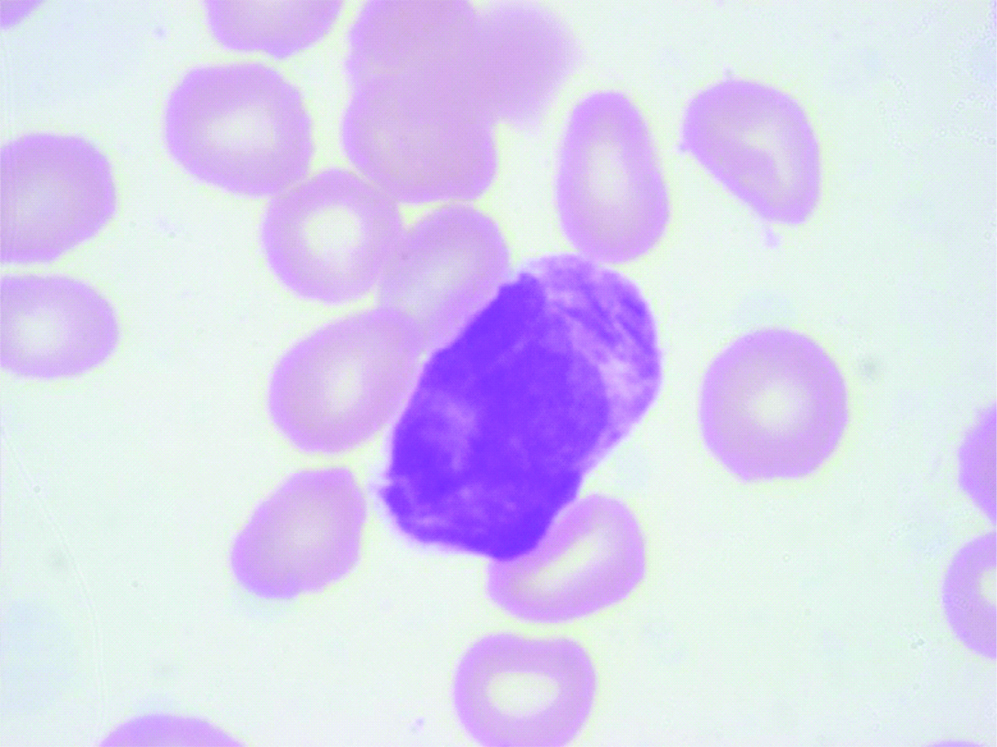
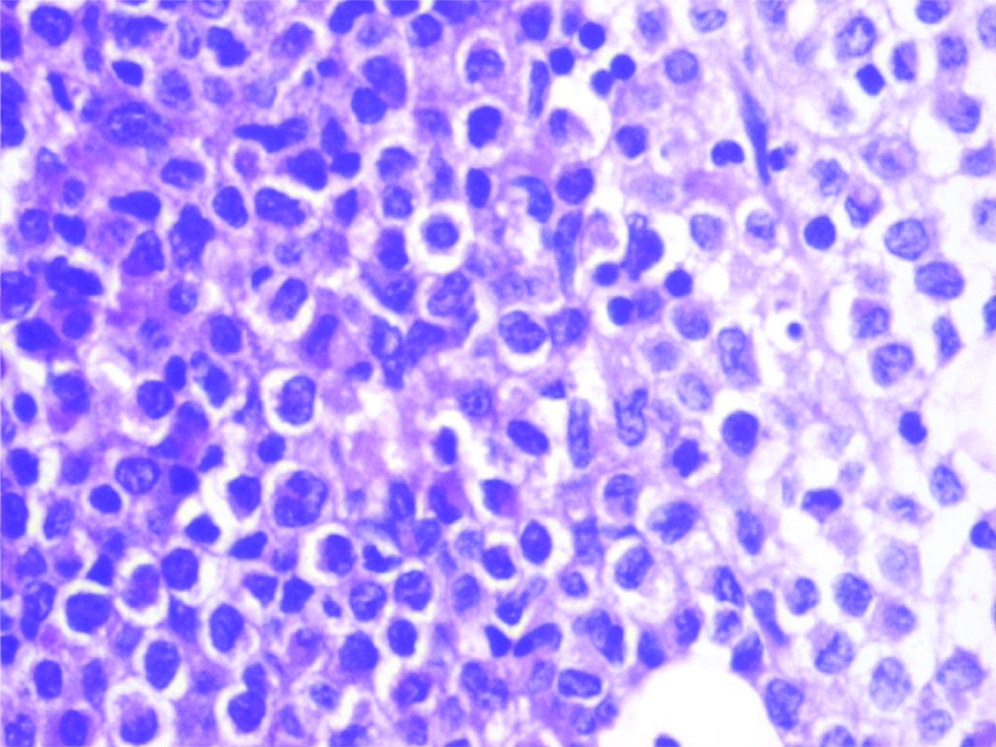
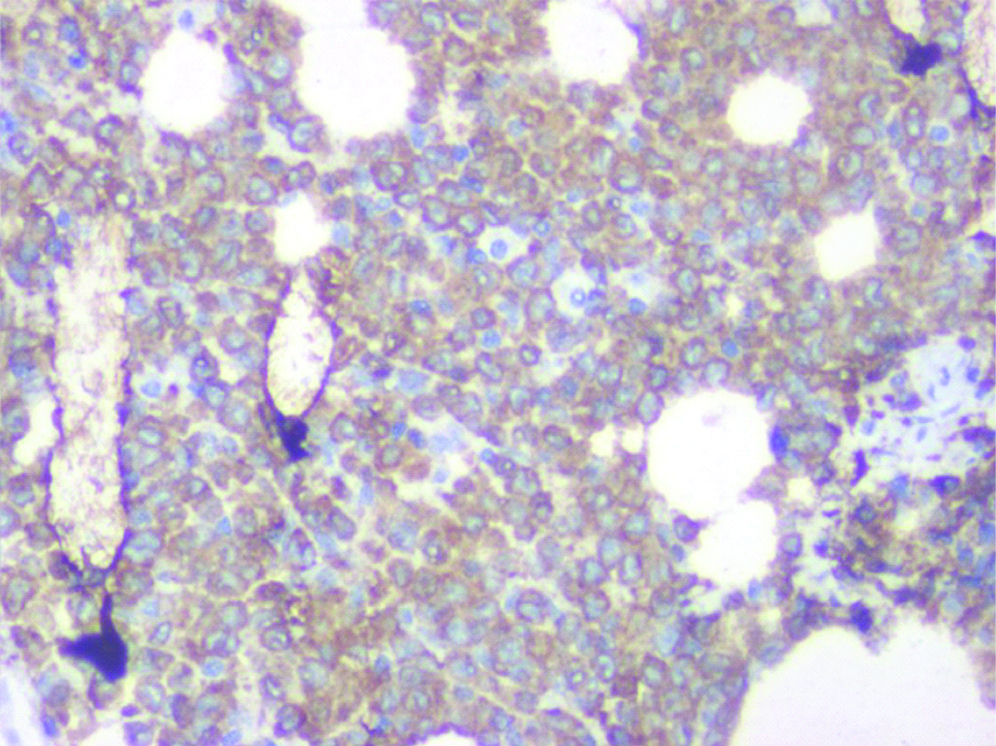
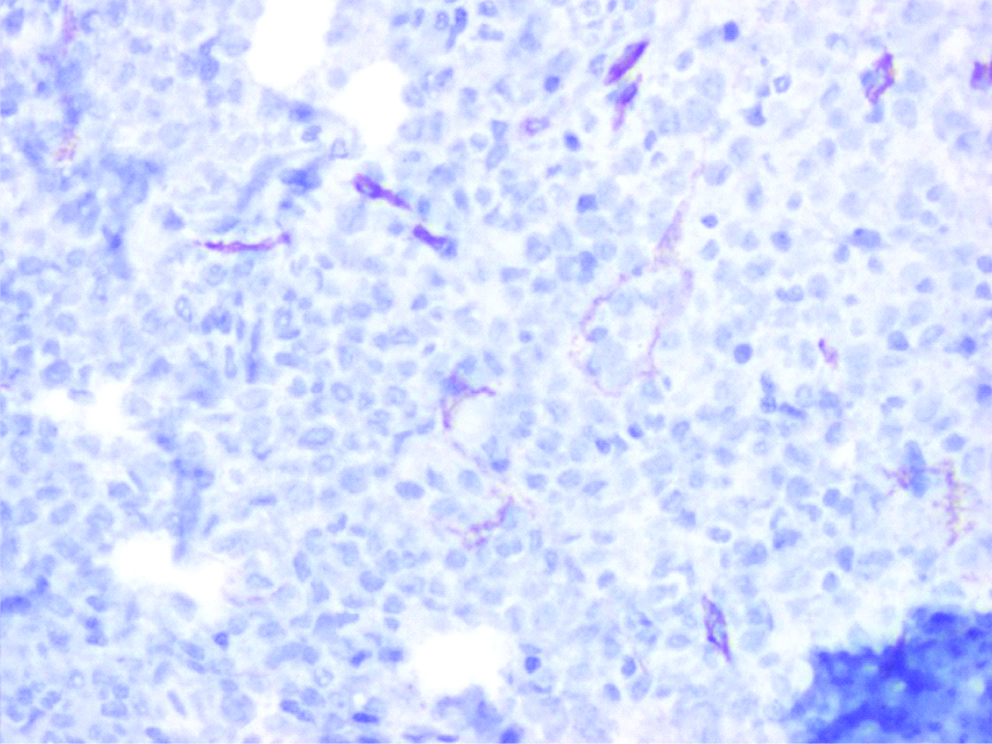
After 18 months of chemotherapy she presented to the casualty with fever of seven days duration and necrotizing gingivitis. Routine blood counts revealed severe pancytopenia with Haemoglobin-5.5 g/dL, White Blood Cell count (WBC)-740/mm3, Absolute Neutrophil Count (ANC)-130/mm3 and Platelet count of 10000/mm3. Bone marrow aspiration and biopsy was performed with a clinical suspicion of metastatic disease or drug induced bone marrow aplasia. The bone marrow aspirate showed atypical promyelocytes characterised by densely packed purple granules with Faggot cells and cells packed with Auer rods [Table/Fig-1]. Based on these findings Acute Promyelocytic Leukaemia (APML) was diagnosed. Bone marrow biopsy showed hypercellularity and was replaced by immature myeloid cells with cytoplasmic granules [Table/Fig-2]. On Immunohistochemistry, these immature cells were strongly positive for Myeloperoxidase (MPO), weakly positive for CD117 and negative for CD34 [Table/Fig-3,4]. Subsequently PML-RARA (t15,17) transcript was detected by Reverse Transcriptase-PCR. Induction with All-trans–retinoic acid and Arsenic tetra oxide was started without further ado following which, count recovery started and bone marrow study on Day 34 post induction was in complete morphological remission.
Bone marrow aspiration showing a promyelocyte packed with auer rod (Giemsa x1000).
Bone marrow biopsy showing immature myeloid cells with cytoplasmic granules (H&Ex400).
Immunohistochemistry on bone marrow biopsy showing strong MPO positivity (IHCx400).
Immunohistochemistry on bone marrow biopsy showing negative CD34 (IHC x400).
Discussion
Therapy related Myeloid Neoplasm (t-MN) is a recognised clinical entity by the World Health Organization, occurring as a complication of the chemo-radiation therapy for primary malignancy [1,2]. Two major clinical subsets of t-MN are described that correlate with the class of the prior therapy. One is the classical t-MN which occurs 5-10 years following exposure to alkylating agents/radiotherapy and often presents with a preleukaemic phase. The second category of t-MN has a latency period of only 1-5 years and follows treatment with Topoisomerase II inhibitors and often presents as overt acute leukaemia without an antecedent Myelodysplastic syndrome [3]. Our case belongs to the second major subset seen in patients who received Topoisomerase II inhibitors.
t-MN accounts for approximately 10-20% of all cases of Acute Myeloid Leukaemia (AML), Myelodysplastic Syndrome (MDS) and Myelodysplastic Syndrome/Myeloproliferative Neoplasm (MDS/MPN) [4]. About 3-13% of all cases of therapy-related Acute Myeloid Leukaemia (t-AML) are t-APML. Though rare, the incidence has been rising worldwide, paralleling the use of Topoisomerase II inhibitors [5]. However, to the best of our knowledge there have been only sporadic case reports of therapy related APML in India. Madabhavi I et al., reported a similar case of APML in a breast cancer survivor post Anthracycline based chemotherapy [6]. Kumar TN et al., reported a case of t-APML in a non seminomatous germ cell tumour following Etoposide therapy [7].
Topoisomerase II inhibitors which includes the Anthracyclins, induces double stranded DNA breaks, causing DNA cleavage and thus is correspondingly linked to leukaemias with balanced translocations [8]. In our case the patient was treated with Epirubicin which could attribute to the (15;17) translocation resulting in APML.
Also another point of discussion would be the fact that only small populations of patients treated with identical protocols actually develop t-MN. This suggests that they may have a heritable predisposition due to mutations in damage sensing genes like BRCA1 and BRCA2 [9]. This may also explain why breast cancer takes the front stand amongst the treated solid tumour to develop second malignancy post chemotherapy [8].
Published literature have shown that t-APML is prognostically better than the other t-AMLs [5,10]. Our patient also responded remarkably to treatment and on regular follow-up is in remission.
Conclusion
In summary, t-APML apart from being the rarest one is also considered the most treatable t-AML. Therefore suspecting and timely diagnosis of the same is of paramount significance.
[1]. Swerdlow, Steven H (Eds). World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. France: IARC Press, Lyon; 2017.585p [Google Scholar]
[2]. Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukaemiaBlood 2016 127:239110.1182/blood-2016-03-64354427069254 [Google Scholar] [CrossRef] [PubMed]
[3]. Godley LA, Larson RA, Therapy-related myeloid leukaemiaSemin Oncol200835(4):418-29.0.1053/j.seminoncol.2008.04.01218692692 [Google Scholar] [CrossRef] [PubMed]
[4]. Granfeldt Ostgard LS, Medeiros BC, Sengeløv H, Norgard M, Anderson MK, Dufva IH, Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukaemia: a national population-based cohort studyJ Clin Oncol 2015 33:364110.1200/JCO.2014.60.089026304885 [Google Scholar] [CrossRef] [PubMed]
[5]. Beaumont M, Sanz M, Carli PM, Maloisel F, Thomas X, Detourmignies L, Therapy-related acute promyelocytic leukaemiaJ Clin Oncol 2003 21:2123-37.10.1200/JCO.2003.09.07212775738 [Google Scholar] [CrossRef] [PubMed]
[6]. Madabhavi I, Modi G, Panchal H, Patel A, Anand A, Parikh S, Treatment related acute promyelocytic leukaemia (t-APML) in breast cancer survivor treated with anthracycline based chemotherapy: Rare case reportInt J Hematol Oncol Stem Cell Res 2015 9(4):215-17. [Google Scholar]
[7]. Kumar TN, Krishnamani , Gandhi LV, Raghunadharao D, Sadashivudu G, Therapy-related acute promyelocytic leukaemia following etoposide-based chemotherapy in non-seminomatous germ cell tumorJ Postgrad Med 2014 60:84-85.10.4103/0022-3859.12882424625948 [Google Scholar] [CrossRef] [PubMed]
[8]. Mistry AR, Felix CA, Whitmarsh RJ, Mason A, Reiter A, Cassinat B, DNA topoisomerase II in therapy-related acute promyelocytic leukaemiaN Engl J Med 2005 352:1529-38.10.1056/NEJMoa04271515829534 [Google Scholar] [CrossRef] [PubMed]
[9]. Schrader KA, Cheng DT, Joseph V, Prasad M, Walsh M, Zehir A, Germline variants in targeted tumor sequencing using matched normal DNAJAMA Oncology 2016 2:104-11.10.1001/jamaoncol.2015.520826556299 [Google Scholar] [CrossRef] [PubMed]
[10]. Pollicardo N, O’Brien S, Estey EH, al-Bitar M, Pierce S, Keating M, Secondary acute promyelocytic leukaemia: characteristics and prognosis of 14 patients from a single institutionLeukaemia 1996 10:27-31. [Google Scholar]