Does Training of Sensory Processing Helps in Improving Motor Execution in Children with Cerebral Palsy?
Kovela Rakesh Krishna1, Ajay Thakur2, HS Sunjyoth3
1 Associate Professor, Department of Physiotherapy, Vikas College of Physiotherapy, Mangaluru, Karnataka, India.
2 Professor and Principal, Department of Physiotherapy, Vikas College of Physiotherapy, Mangaluru, Karnataka, India.
3 Lecturer, Department of Physiotherapy, Vikas College of Physiotherapy, Mangaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kovela Rakesh Krishna, Vikas College of Physiotherapy, Mary Hill, Mangaluru-575008, Karnataka, India.
E-mail: rakeshkrishna.pt@gmail.com
Dear Editor,
We are pleased to share with you an interesting case which came to our department eight weeks back. The patient was a 13-year-old boy, diagnosed with mild hypotonic Cerebral palsy when he was 18-month-old. He was at GMFCS level II. Motor development was delayed. He started to walk at the age of eight years.
He presented with complaints of difficulty in balancing and maintaining posture on his own while standing and walking. He was able to communicate in mother tongue and respond to commands. He was an 8th standard student and was going to a normal school, with help of parents and friends and not a special school as parents do not want to send him to special school. He was able to play indoor games in school but was not able to play any outdoor games because of his disability. Parents tried to train him at home with some exercises insisted by a paediatrician. Their relatives told them about the importance of Physiotherapy and referred them to our department.
On assessment, we observed Sensory Processing disturbances in him [1]. He had issues with performing coordinated activities involving upper limbs, difficulty in transitioning from sitting to standing position, difficulty in standing unsupported. The greatest ability of the child was to be able to walk with the support of one person. Problems in posture control, motor planning and coordination made us assess his sensory processing, concentrating on proprioception, vestibular system and tactile sensation. He was sometimes over-active and avoidant of tactile experience; we felt it was a predisposing factor for irregular emotional tone. He was bumping into objects and used to slap his feet while walking, this made us think about his proprioceptive hyposensitive nature. He was very cautious and slow moving while walking, uncomfortable while climbing stairs and while sitting on Physio ball. This made us think about his vestibular system. With our assessment we found him to be tactile hypersensitive, proprioceptive hyposensitive and vestibular hypersensitive child [2].
We confirmed the findings by assessing through sensory profile care giver questionnaire [3] duly filled by mother who knows English fluently. Permission was obtained from the author to use the tool.
The development of both gross and fine motor skills depends heavily on the somatosensory system [4]. Proprioceptive and Vestibular issues in the child are the main reason behind difficulty in performing activities involving motor skill. He faced difficulty in eye hand coordination and integrating his both sides in playful activities, which requires sequencing of events. This helped us to visualise the child as suffering from Somatodyspraxia and bilateral integration and sequencing disorder. Thus, we analysed the child to have findings similar to sensory based motor disorder by considering his postural and tonal abnormalities. We aimed at improving his tactile, proprioceptive and vestibular sensations and thereby correcting his motor issues.
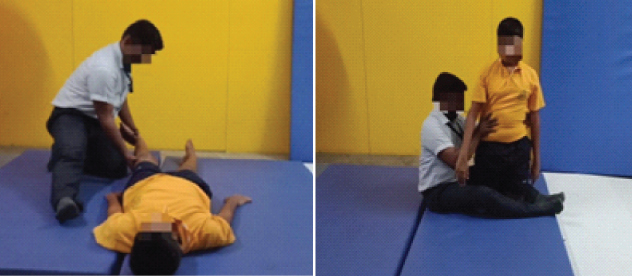
We used low mats and bolsters instead of balls to enhance his optimal vestibular function. We tried to use superficial touch as much as possible in the early sessions as he was avoiding tactile inputs, to facilitate task oriented training to improve his motor planning. Once the child started appreciating the tactile sensations, we started using Proprioceptive Neuromuscular Facilitation (PNF) techniques [Table/Fig-1a,b], mainly dynamic reversals, rhythmic initiation and rhythmic stabilisation to improve strength of lower limb musculature [5].
a) PNF strengthening of lower limb; b) Transitioning training using PNF Techniques.
Treatment was scheduled for one hour in every session, five times a week for eight weeks from September 2018 to November 2018 and post treatment we took sensory profile and assessed child while transitioning on low mat [Table/Fig-2]. We found tremendous improvement in the child in terms of appreciating various sensations and utilising them in his activities of daily life. He became comfortable with movable surfaces, climbing stairs and decreased stamping of the foot on ground while walking.
Section raw score of sensory profile pre and post treatment.
| Section | Section raw score total (Pre) | Section raw score total (post) |
|---|
| Touch Processing | 50/90 | 70/90 |
| Vestibular Processing | 32/55 | 46/55 |
| Multisensory Processing | 20/35 | 29/35 |
| Modulation related to body position and movement | 26/50 | 39/50 |
Thorough clinical examination and utilisation of appropriate sensory inputs helped the child to gain benefits in his motor planning and execution. Thus, we conclude by stating that we should also look into sensory processing while managing motor disorders as it will help us to address the problem at its root level. Presently, the child visits for follow-up twice in a week, since past two months where we are evaluating his functional activities mainly transitions and gait. We found that he is maintaining the benefits which he got in his eight weeks of treatment.
[1]. Ayres AJ, Sensory Integration and the Child 1979 Los Angeles, CAWestern Psychological Services [Google Scholar]
[2]. Pavao SL, Rocha NACF, Sensory processing disorders in children with cerebral palsyInfant BehavDev 2017 46:01-06.10.1016/j.infbeh.2016.10.00727866043 [Google Scholar] [CrossRef] [PubMed]
[3]. Dunn W, The impact of sensory processing abilities on the daily lives of young children and their families: a conceptual modelInfants and Young Children 1997 9(4):23-35.10.1097/00001163-199704000-00005 [Google Scholar] [CrossRef]
[4]. Cascio CJ, Somatosensory processing in neurodevelopmental disordersJ NeurodevelopDisord 2010 2:62-69.10.1007/s11689-010-9046-3 [Google Scholar] [CrossRef]
[5]. Kumar C, Ostwal P, comparison between tasks oriented training and proprioceptive neuromuscular facilitation exercises on lower extremity function in cerebral palsy-a randomized clinical trialJ Nov Physiother 2016 6(2):01-09.10.4172/2165-7025.1000291 [Google Scholar] [CrossRef]