Introduction
Structural immaturity of muscular system in Preterm Infants (PTI) results in maturation related hypotonia which is found to be influenced by risk factors present at the time of birth. Low muscle tone can lead to lower extremity malalignment, abnormal positioning and loading resulting in musculoskeletal problems that could have an impact on motor development which is not well established.
Aim
This study was carried out to analyse the risk factors associated with low muscle tone in PTI and the impact of common musculoskeletal problems on motor development of PTI at 1 year of corrected age.
Materials and Methods
This Cross sectional study was carried out in 36 PTI and 36 Full Term Infants (FTI) who were recruited from Child Development unit and the details of risk factors were obtained from the records. Infants were assessed for muscle tone using Amiel Tison Angles (ATA) and Hyperextension of knee (HEK) was measured using goniometer. Foot prints were obtained and assessed for the level of Pes planus by Foot Arch Index (FAI) and Calcaneovalgus by Staheli index (SI). Peabody Developmental Motor Scale 2 (PDMS 2) was used to evaluate motor development. Backward multiple regression, Chi-square test Pearson’s correlation were used for data analysis.
Results
Backward multiple regression analysis showed statistically significant association of Birth weight, Gestational Age, and Apgar score with low muscle tone in PTI (p<0.05). Chi-square test was used to compare the muscle tone of PTI and FTI which showed that ATA of PTI was significantly higher than FTI but within physiological limits (p<0.05). Pearson’s correlation coefficient showed that there is statistically significant positive correlation between muscle tone and musculoskeletal problems and a negative correlation between musculoskeletal problems and Gross Motor Quotient (GMQ) of PDMS 2 in PTI at 1 year of corrected age (p<0.05).
Conclusion
Maturation related hypotonia carried during the first year of life brings about musculoskeletal problems which have an impact on motor development in PTI. The result accentuates that clinicians should address the subtle tonal deviations at an early age to prevent musculoskeletal problems and intervene if required when they are affecting the motor development of PTI.
Amiel tison angles, Maturation related hypotonia, Peabody developmental motor scale 2, Preterm infants
Introduction
Preterm birth is a significant public health problem across the world which is associated with neonatal mortality, short and long-term morbidity and disability in later life [1]. According to World Health Organisation (WHO), infants who are delivered at less than 37 weeks of gestational age are considered as PTI [2]. Preterm birth is an important determinant of child health as it is associated with an increased risk of deaths. 15 million infants are born preterm every year across the world out of which 1 million infants die due to direct complications and PTI who survive face long term adverse outcomes impairing neurodevelopmental functions. [3].
Neonatal complications that are associated with preterm birth such as hypoglycaemia, hypothermia, apnoea, respiratory distress syndrome, sepsis, hyperbilirubinemia, and seizures [4] demands close monitoring during the immediate neonatal period and during the first year of life. The increased risk of complications in PTI often arise from immature organ system. Increased demands to support a functional transition from intrauterine to extrauterine life can have an impact on neurodevelopmental outcomes when compared with FTI [5].
PTI have underdeveloped lungs and are more likely to have impaired respiratory function due to which they do not tolerate labour as like FTI leading to a low Apgar score, sepsis and prolonged hospitalisation [6]. Immature thermoregulatory system makes the infant vulnerable to infections and incomplete nephrogenesis becomes the potential cause of neonatal hyperbilirubinemia which results in challenges like behavioural, learning and motor skill development problems [7,8].
The first year of an infant life is the critical period of brain development as the cerebral maturation brings about the maturation of autonomic system, tactile, vestibular, hearing and vision [9]. The structural neuronal differentiation, glial cell growth, myelination, axonal and dendritic growth of the central nervous system occurs rapidly between 23 and 32 weeks of gestational age. PTI spend long periods in neonatal intensive care resulting in alterations to brain development caused by exposure to the extrauterine environment during critical periods which causes the PTI to adapt less flexed posture and more extended posture than FTI [10]. As a result, their muscles appear to be floppy and weak in the first few weeks after birth resulting in impaired motor development [11].
Structural immaturity of the muscular system in PTI results in maturation related hypotonia which leads to reduced force production by the muscles against gravity [12]. In order to achieve optimal muscle tone which is the ability to resist passive stretch, muscles should be able to sustain a continuous and passive partial contraction [13]. If opportunities for this essential movement driven development are restricted, the risk of developing low muscle tone is increased in PTI.
The low toned muscles cannot fully contract before they relax and do not attain their full potential for initiating and sustaining a muscle contraction on movement which makes the infant contract the muscles very slowly in response to stimulus [14]. Hypotonia along with ligamentous laxity may lead to lower extremity malalignment and recognising problems related to these musculoskeletal structures and their interactions with that of the motor development is important for evaluation and treatment planning [15].
The musculoskeletal problems found in PTI are calcaneovalgus, flexible flat foot followed by metatarsus adductus [16]. The Pes planus along with calcaneovalgus are commonly seen in children up to the age of 5 years and they result in problems on the static and dynamic alignment of ankle and foot [17]. Therefore, more precise and periodic assessments of these musculoskeletal problems should be addressed at an early age to prevent problems in motor development.
A delay in a skill becomes evident only at the age when a specific developmental milestone expected is not achieved. Hence, it is challenging to distinguish between the isolated deformities and from those that might result from low muscle tone in PTI which could result in disability. This study intends to find the association of various risk factors to low muscle tone and the impact of musculoskeletal problems which could emerge due to low muscle tone on the motor development at 1 year of life in PTI.
Materials and Methods
This Cross sectional Study was approved by the Ethics committee (CSP/17/OCT/61/264) of Sri Ramachandra Institute of Higher Education and Research. The study was conducted over a period of eight months from October 2017 to May 2018 and subjects were recruited from the Child development unit when the PTI returned back for the neurodevelopmental assessment at 1 year of corrected age. 36 PTI of both genders at one year of corrected age with normal cranial ultrasonography findings and 36 FTI of both genders were included in the study. Subjects who had neurological impairments, congenital deformities, hearing and vision impairment were excluded from the study.
Instrumentation
The Peabody Developmental Motor Scales-Second Edition (PDMS-2)
PDMS-2 is a paid paediatric tool commonly used to assess motor development in children from age 0-72 months [Table/Fig-1]. It consists of 6 subscales (Reflex, Stationary, Locomotion, Object manipulation, Grasping, Visual motor integration) of which summation of scores from 4 subscales gives a Gross Motor Quotient (GMQ) [18]. The test was conducted based on the instructions provided in the manual. The standard scores, age equivalent, quotient scores were obtained from raw scores. The standard scores were converted into GMQ scores which are interpreted as poor, below average, average, above average and superior level of gross motor development based on the GMQ scores.
Peabody developmental motor scale-2.

Goniometer
The universal standard goniometer is an apparatus designed to measure the joint angle between the axis of two articulating bones with high reliability Intraclass Correlation Coefficients (ICC=0.87) [19]. The stationary arm is aligned parallel to the proximal body part and movable arm is aligned along the axis of distal body part [Table/Fig-2]. The universal goniometer showed high reliability with ICC=0.87. In this study Goniometer is used to measure the ATA.

Foot Print Analysis
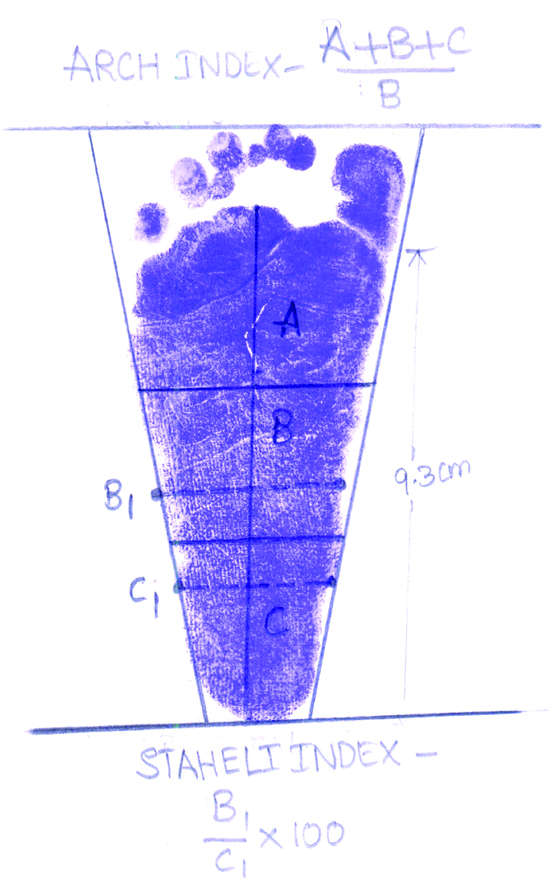
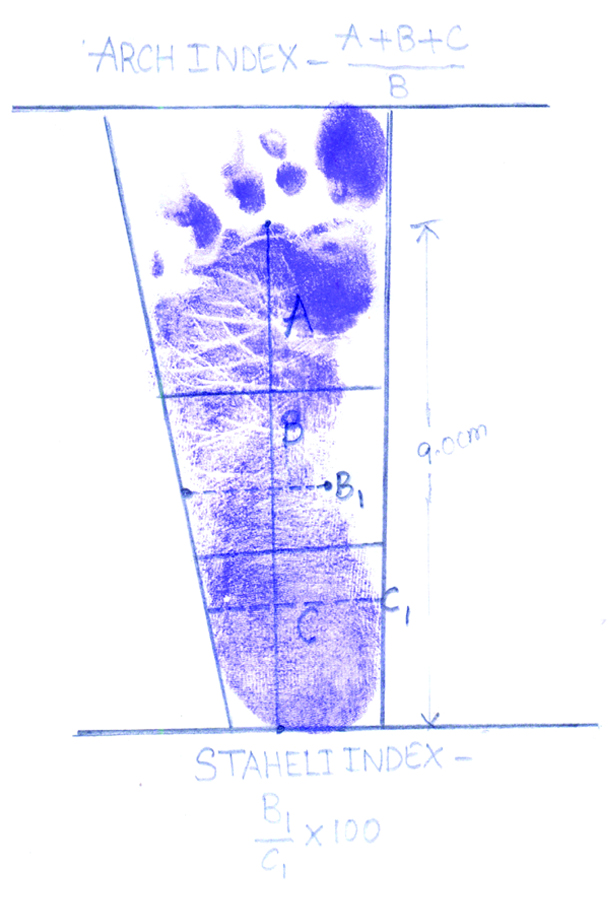
The footprint analysis is used as a tool to assess the arch index by using stamp pad with the child in supported standing position [20]. The length of the foot (excluding the toes) is equally divided into mid foot, forefoot and hind foot by using inch tape. The FAI is then calculated by dividing the mid foot region (B) by the entire truncated foot area (i.e., Arch index=B/{A+B+C}) with higher ratio indicating flat foot. This measure has been shown to exhibit excellent reproducibility in child and adolescent populations and has been validated against radiographs of the foot [21].
The SI is the ratio obtained by dividing narrowest area of the mid foot to the widest area of the hind foot (B1/C1×100) by using inch tape. This index represents as one of the most considered for the description of footprint deformities like valgus and for the detection of flat foot [Table/Fig-3,4].
Procedure
PTI at 1 year of corrected age who met the inclusion criteria were taken as the subjects for the study after obtaining informed consent from the care taker. The details of risk factors (Gestational age, Birth weight, Apgar score, NICU stay, Sepsis, Neonatal Hyperbilirubinemia and Hypoglycaemia) were collected from the birth records. Muscle tone was assessed using ATA (Adductor, Popliteal, Dorsiflexion and Heel to ear) with a goniometer. Infants were evaluated for foot posture by foot print analysis in supported standing. Two measurements - FAI and SI were calculated from the foot print by using inch tape. The Hyperextension of Knee (HEK) was measured using a goniometer. The PDMS-2 was used to evaluate motor development in PTI at 1 year of corrected age. FTI were assessed with same outcome measures at one year chronological age
Method of Measuring the ATA [22,23]
Adductor angle was measured with the infant positioned in supine, both hip and knee in vertical with the trunk and by gently abducting the lower extremities. The angle is measured by placing the fulcrum of goniometer at symphysis pubis and both the arms in parallel to the inner aspect of femur.
Heel-to-ear angle was measured placing the child in supine with both legs extended and the legs are moved as a whole toward the vertex. The goniometer is placed at back of the leg near greater trochanter with one arm parallel to the femur and another arm parallel to the couch. The angle that the lower extremities make with the couch is measured.
Popliteal angle was measured with the infant in supine. With the hands placed over the child’s knees, the thighs are flexed laterally and the knees are extended from flexed position. The angle is determined based on the measurement between the thigh and calf. Both legs are measured simultaneously.
Dorsiflexion angle was obtained with infant placed in supine. The fulcrum of the goniometer is placed along lateral malleolus, the stationary arm along the fibula, and the movable arm parallel to the fifth metatarsal bone. The ankle is moved from neutral to dorsiflexion position and the angle measured is documented.
Statistical Analysis
Statistical analysis was performed using SPSS version 17.0. Backward multiple Regression was used to find out the association of risk factors with low muscle tone. Chi square analysis was used to compare muscle tone of PTI and FTI and Pearson Correlation was used to correlate ATA and musculoskeletal deviations which included FAI, SI, and HEK in PTI at 1 year of corrected age. The p-value of <0.05 was considered significant.
Results
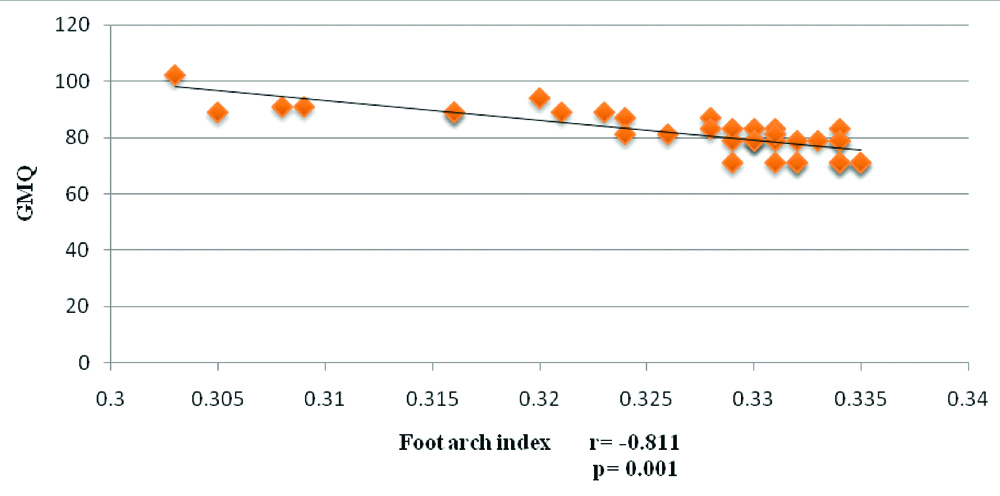
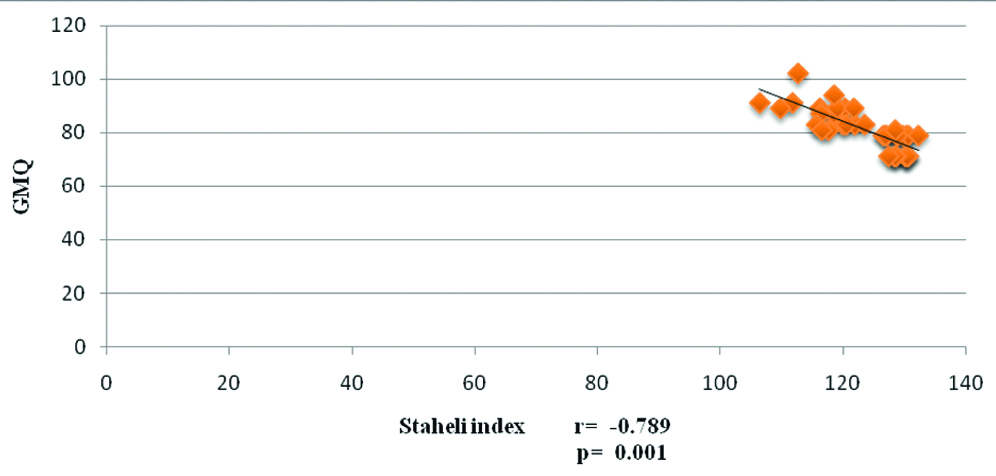
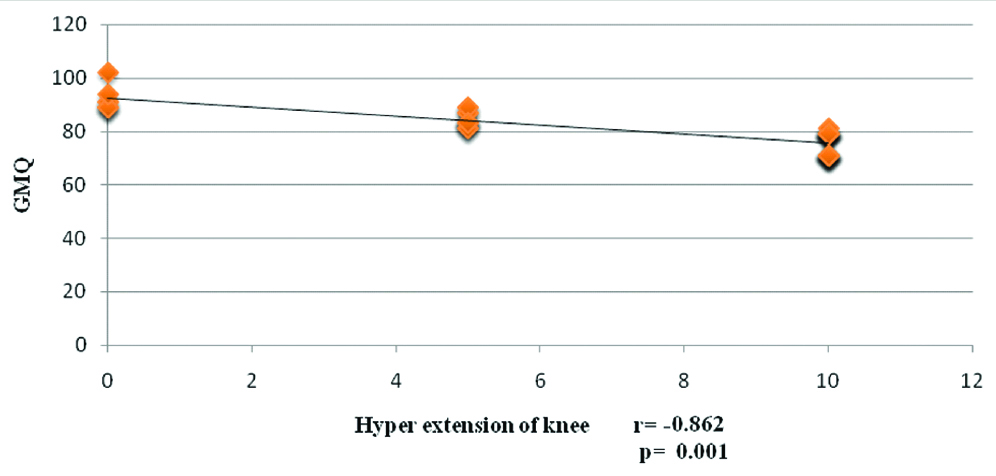
Total of 36 FTI and PTI at one year of corrected age participated in this study which included 21 male and 15 female PTI and 22 male and 14 female FTI. [Table/Fig-5] shows the baseline values of the risk factors and association of risk factors with low muscle tone showed that birth weight, gestational age and Apgar score were significantly associated with p<0.05 [Table/Fig-6]. Chi-square analysis showed that ATA of PTI are at higher range which conveys that PTI have low muscle tone when compared to FTI with statistically significant p<0.05 [Table/Fig-7]. Musculoskeletal Problems and GMQ in PTI and FTI is shown in [Table/Fig-8]. Correlation of ATA and musculoskeletal deviations in PTI at 1 year of corrected age shows a statistically significant strong positive correlation with r>0.07 and p<0.05 [Table/Fig-9]. A strong negative correlation of FAI, SI, HEK and GMQ of PDMS 2 of PTI is seen at 1 year of corrected age with statistically significant r > -0.07 and p<0.05 [Table/Fig-10].
| Variables | PTI (N=36) | SD | FTI (N=36) | SD |
|---|
| Gestational age (weeks) | 31.11 | 1.6 | 38.3 | 1.2 |
| Birth weight (grams) | 1344.75 | 446.2 | 3136.25 | 121.0 |
| Apgar score | 7.13 | 0.83 | 8.74 | 0.23 |
| NICU stay (days) | 11.83 | 7.3 | 5 | 0.42 |
| Hyperbilirubinaemia No present/36 | 12 | | 5 | |
| Hypoglycaemia No present/36 | 8 | | 2 | |
| Sepsis No present/36 | 7 | | 4 | |
Backward multiple regression. *Significant p<0.05.
| Dependent variable | Model | Unstandardised Coefficients | Standardised Coefficients | t-value | p-value |
|---|
| B | Std. Error | Beta |
|---|
| Adductor angle | (Constant) | 223.80 | 19.91 | | 11.24 | 0.001* |
| Birth weight | -0.01 | 0.00 | -0.75 | -7.23 | 0.001* |
| GA | -2.95 | 0.90 | -0.52 | -3.26 | 0.001* |
| Apgar Score | 5.17 | 1.53 | 0.47 | 3.37 | 0.001* |
| Popliteal angle | (Constant) | 253.60 | 25.11 | | 10.09 | 0.001* |
| Birth weight | -0.01 | 0.00 | -0.77 | -7.01 | 0.001* |
| GA | -3.44 | 0.97 | -0.70 | -3.54 | 0.001* |
| Apgar Score | 4.82 | 1.42 | 0.50 | 3.38 | 0.001* |
| Heel-Ear angle | (Constant) | 248.50 | 17.00 | | 14.61 | 0.001* |
| Birth weight | -0.01 | 0.00 | -0.65 | -7.22 | 0.001* |
| GA | -3.44 | 0.77 | -0.63 | -4.45 | 0.001* |
| Apgar Score | 4.28 | 1.30 | 0.40 | 3.27 | 0.03* |
| Dorsiflexion angle | (Constant) | 125.08 | 19.79 | | 6.32 | 0.001* |
| Birth weight | -0.01 | 0.00 | -0.70 | -5.68 | 0.001* |
| GA | -2.33 | 0.92 | -0.48 | -2.52 | 0.01* |
| Apgar Score | 3.36 | 1.58 | 0.35 | 2.11 | 0.04* |
Comparison of Muscle Tone (ATA) Between PTI and FTI.
| ATA angles | PTI (n=36) | FTI (n=36) | χ2 | p-value |
|---|
| Adductor |
| 130-144 | 4 (11.1%) | 24 (66.6%) | 23.38a | 0.001* |
| 145-160 | 32 (88.9%) | 12 (33.3%) | 0.001* |
| Popliteal |
| 130-149 | 4 (11.1%) | 28 (77.86%) | 32.40a | 0.001* |
| 150-170 | 32 (88.9%) | 8 (22.2%) | 0.001* |
| Heel-Ear |
| 130-149 | 4 (11.1%) | 28 (77.86%) | 32.40a | 0.001* |
| 150-170 | 32 (88.9%) | 8 (22.2%) | 0.001* |
| Dorsiflexion |
| 40-54 | 8 (22.2%) | 28 (77.8%) | 22.22a | 0.001* |
| 55-70 | 28 (77.8%) | 8 (22.2%) | 0.001* |
Chi-square test *Significant p<0.05
Musculoskeletal problems and GMQ in PTI and FTI.
| Variables | | PTI mean (SD) | FTI mean (SD) |
|---|
| FAI | Right | 0.32 (0.00) | 0.29 (0.00) |
| Left | 0.32 (0.00) | 0.29 (0.00) |
| SI | Right | 123.17 (6.97) | 95.93 (3.10) |
| Left | 123.84 (6.54) | 95.64 (3.68) |
| HEK | Right | 6.53 (3.93) | 1.25 (2.50) |
| Left | 6.67 (3.78) | 1.25 (2.50) |
| GMQ | 81.50 (7.65) | 106.17 (2.84) |
Correlation of ATA and musculoskeletal problems in PTI.
| Variables | Mean (SD) | Pearson correlation (r) | p-value |
|---|
| (n=36) | Right | Left |
|---|
| Adductor | 153.83 (9.16) | | | |
| FAI | | 0.94 | 0.94 | 0.001* |
| SI | 0.84 | 0.82 | 0.001* |
| HEK | 0.78 | 0.80 | 0.001* |
| Popliteal | 159.36 (8.01) | | | |
| FAI | | 0.94 | 0.95 | 0.001* |
| SI | 0.79 | 0.79 | 0.001* |
| HEK | 0.8 | 0.81 | 0.001* |
| Heel to ear | 158.42 (8.91) | | | |
| FAI | | 0.9 | 0.91 | 0.001* |
| SI | 0.85 | 0.82 | 0.001* |
| HEK | 0.81 | 0.81 | 0.001* |
| Dorsiflexion | 59.47 (7.95) | | | |
| FAI | | 0.91 | 0.92 | 0.001* |
| SI | 0.79 | 0.77 | 0.001* |
| HEK | 0.83 | 0.84 | 0.001* |
Pearson’s correlation *Significant p<0.05
Correlation of musculoskeletal problems and GMQ in PTI.
| Variables | Pearson correlation (r) | p-value |
|---|
| Gross motor quotient (n=36) | |
|---|
| FAI | Right | -0.811 | 0.001* |
| Left | -0.770 | 0.001* |
| SI | Right | -0.798 | 0.001* |
| Left | -0.862 | 0.001* |
| HEK | Right | -0.862 | 0.001* |
| Left | -0.86 | 0.001* |
Pearson’s correlation *Significant p<0.05
Discussion
The integrity of neuromuscular and musculoskeletal system is important for the normal motor development of infants. The growth and maturity of the musculoskeletal system occur rapidly from 7 to 18 months resulting in many biomechanical changes as the child attains a bipedal stance with a decreased base of support and increased demands in muscle work to maintain adequate posture and balance. Muscle tone forms the basis of movement and postural stability to maintain upright posture against gravity and disturbances to muscle tone may affect the movement performance and posture [24]. Muscle tone in PTI is less compared to FTI which could have an impact on the biomechanical transference of weight resulting in musculoskeletal deviations in PTI.
Low Birth Weight, Gestational Age and Apgar score had greater association with decreased muscle tone. A study done by Gajdosik R et al., showed that number of contractile and non-contractile protein of the sarcomere cytoskeleton determines the resistance to passive lengthening [25]. Decreased birth weight could result in decreased sarcomeres which could bring about low muscle tone as subsequent weight gain of an infant in the first year of life depends on the birth weight which significantly affects the motor development as evident in the later stages of growth of infants [26].
Gestational age refers to level of growth and maturity of various systems at birth. Prematurity is found to be an indicator of newborn muscle tone as shown by Silva E et al., which is in concordance with the current study showing significant association even when the infants were assessed with correction of age [27]. Schonhaut L et al., showed that gestational age and risk of developmental disability had linear inverse relationship which could be due to decreased motor efficiency of low toned muscles as evident by the significant association in this study [Table/Fig-7] [28].
Muscle tone of PTI at 1 year corrected age is found to be significantly lower than FTI though they fall into the normal physiological range [Table/Fig-8]. This implies that maturation related hypotonia is carried even at 1 year of age which is similar with the study done by Vungarala P et al., where low muscle tone was found to be decreased at 8 months of corrected age affecting the motor development in PTI [29].
Presence of fat pad causes medial longitudinal arch to disappear resulting in physiological flatfoot and greater hindfoot motion in term infants at 1 year of age making the entire foot come in contact with the ground during weight bearing [30]. FAI and SI were significantly higher in PTI than FTI in the current study reflecting the fact that flat foot and valgus were higher than physiological range in PTI [Table/Fig-9]. Pes planus, calcaneovalgus, and hyperextension of knee showed a strong positive correlation with ATA which convey that low muscle tone is the major contributing factor for musculoskeletal deviations in PTI [Table/Fig-10]. The resting length of the muscle is greater than average causing hypermobility of joints in children with low muscle tone which along with increased laxity of ligaments and joint capsule leads to decreased proprioception and brings about musculoskeletal deviations in weight bearing position [31].
The joint instability contributes to non-optimal musculoskeletal alignment and is not only influenced by ligament laxity but also influenced by the decreased muscle tone and reduced co-contraction around the joint as shown by Atun-Einy O et al., which could result in predisposition to biomechanical disadvantage of foot, ankle and knee complex of these children [32]. In a closed kinematic chain, the stability of proximal joints depends on the stability of distal joints which are significantly interrelated to contribute for overall stability of trunk and lower extremities [33]. Therefore foot deviations definitely impact the stability of trunk which results in delayed standing and influences the gross motor development of PTI than FTI which is evident by showing strong negative correlation of musculoskeletal problems and GMQ [Table/Fig-11,12 and 13]. Fine motor performance was comparatively better than gross motor performance in PTI conveying the fact that maturation related hypotonia impacts more in the lower limb due to weight bearing and weight transference demands of gross motor activities resulting in musculoskeletal deviations. So, early identification and addressing hypotonia might prevent gross motor delay in PTI.
Correlation of FAI (Right) and GMQ of PTI.
Correlation of SI (Right) and GMQ of PTI.
Correlation of HEK (Right) and GMQ of PTI.
Limitation
Study considered assessment at single time point, follow-up could have been done at second year to know the status of musculoskeletal problems and impact on motor development.
Conclusion
The result of the study emphasises the clinicians that subtle tonal deviations in PTI should be addressed and strategies that promote musculoskeletal maturity need to be initiated at an early age to prevent musculoskeletal problems leading to biomechanical compromise that affects the motor development.
Chi-square test *Significant p<0.05
Pearson’s correlation *Significant p<0.05
Pearson’s correlation *Significant p<0.05
[1]. Mwansa-Kambafwile J, Cousens S, Hansen T, Lawn JE, Antenatal steroids in preterm labour for the prevention of neonatal deaths due to complications of preterm birthInternational Journal of Epidemiology 2010 39(Supplement 1):I122-33.10.1093/ije/dyq02920348115 [Google Scholar] [CrossRef] [PubMed]
[2]. Quinn J, Munoz F, Gonik B, Frau L, Cutland C, Mallett-Moore T, Preterm birth: Case definition & guidelines for data collection, analysis, and presentation of immunisation safety dataVaccine 2016 34(49):6047-56.10.1016/j.vaccine.2016.03.04527743648 [Google Scholar] [CrossRef] [PubMed]
[3]. Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller A, Born Too Soon: The global epidemiology of 15 million preterm birthsReproductive Health 2013 10(Suppl 1)10.1186/1742-4755-10-S1-S224625129 [Google Scholar] [CrossRef] [PubMed]
[4]. Tsai M, Lien R, Chiang M, Hsu J, Fu R, Chu S, Prevalence and morbidity of late preterm infants: current status in a medical center of northern TaiwanPediatrics & Neonatology 2012 53(3):171-77.10.1016/j.pedneo.2012.04.00322770105 [Google Scholar] [CrossRef] [PubMed]
[5]. Behrman RE, Butler AS, Preterm Birth: Causes, Consequences, and Prevention. 2007 Institute of Medicine (US)Committee on Understanding Premature Birth and Assuring Healthy OutcomesISBN-13:978-0-309-10159-2 [Google Scholar]
[6]. de Kieviet J, Piek J, Aarnoudse-Moens C, Oosterlaan J, Motor Development in Very Preterm and Very Low-Birth-Weight Children From Birth to AdolescenceJAMA 2009 302(20):223510.1001/jama.2009.170819934425 [Google Scholar] [CrossRef] [PubMed]
[7]. Mcgrath JM, Hardy W, (n.d.). 17 The Infant at Risk:362-414. [Google Scholar]
[8]. VK B, Johnson L, Kernicterus: a preventable neonatal brain injuryJ. Arab Neonatal Forum 2005 2:12-24. [Google Scholar]
[9]. Tecklin J, Paediatric Physical therapy 2008 4th edLippincott Williams and Wilkins [Google Scholar]
[10]. Allen M, Aucott S, Cristofalo E, Alexander G, Donohue P, Extrauterine neuromaturation of low risk preterm infantsPediatric Research 2009 65(5):542-47.10.1203/PDR.0b013e3181998b8619127205 [Google Scholar] [CrossRef] [PubMed]
[11]. Bodensteiner J, The Evaluation of the Hypotonic InfantSeminars in Pediatric Neurology 2008 15(1):10-20.10.1016/j.spen.2008.01.00318342256 [Google Scholar] [CrossRef] [PubMed]
[12]. Carole Kenner, Judy Wright Lott. Comprehensive Neonatal Care: An Interdisciplinary Approach IV Edition [Google Scholar]
[13]. Joseph K, Fahey J, Shankardass K, Allen V, O’Campo P, Dodds L, Effects of socioeconomic position and clinical risk factors on spontaneous and iatrogenic preterm birthBMC Pregnancy and Childbirth 2014 14(1)10.1186/1471-2393-14-11724670050 [Google Scholar] [CrossRef] [PubMed]
[14]. de Groot L, Posture and motility in preterm infantsDevelopmental Medicine & Child Neurology 2000 42(01):6510.1017/S001216220000012810665978 [Google Scholar] [CrossRef] [PubMed]
[15]. Developmental-Behavioral Pediatrics 4th edition, by William B. Carey, Allen C. Crocker, William L. Coleman, Ellen Roy Elias, and Heidi M. Feldman ISBN: 978-1-4160-3370-77 [Google Scholar]
[16]. Chotigavanichaya C, Leurmsumran P, Eamsobhana P, Sanpakit S, Kaewpornsawan K, The incidence of common orthopaedic problems in newborn at Siriraj HospitalJournal of the Medical Association of Thailand 2012 95(Suppl 9):S54-61. [Google Scholar]
[17]. Price C, Morrison S, Hashmi F, Phethean J, Nester C, Biomechanics of the infant foot during the transition to independent walking: A narrative reviewGait & Posture 2018 59:140-46.10.1016/j.gaitpost.2017.09.00529031139 [Google Scholar] [CrossRef] [PubMed]
[18]. Hinderer KA, Richardson PK, Sarah W, Atwater Clinical implication of the peabody developmental motor scalesPhysical & Occupational Therapy In Pediatrics 1989 9(2):81-106.10.1080/J006v09n02_06 [Google Scholar] [CrossRef]
[19]. White D, Measurement Of Joint Motion A Guide To Goniometry 2009 4th EditionF A Davis Company [Google Scholar]
[20]. Hazzaa H, El-Meniawy GE, Ahmed S, Bedier M, CorrelationTrends in Applied Sciences Research 2015 10(4):207-15.10.3923/tasr.2015.207.215 [Google Scholar] [CrossRef]
[21]. Vincent, Lauren. Differences in arch index, rear foot plantar pressure, and forefoot deviation from center of force trajectory in those with chronic ankle instability, no history of lateral ankle sprain and copers IUScholarWorks. Indiana University 2014 https://scholarworks.iu.edu/dspace/bitstream/handle/2022/17626/Thesis [Google Scholar]
[22]. Amiel-Tison C, Neurological evaluation of the maturity of newborn infantsArchives of Disease in Childhood 1968 43(227):89-93.10.1136/adc.43.227.895689329 [Google Scholar] [CrossRef] [PubMed]
[23]. Chaudhari S, Deo B, Neurodevelopmental assessment in the first year with emphasis on evolution of toneIndian Pediatrics 2006 43:527-34. [Google Scholar]
[24]. Vanenko Y, Gurfinkel V, Human postural controlFrontiers in Neuroscience 2018 :1210.3389/fnins.2018.0017129615859 [Google Scholar] [CrossRef] [PubMed]
[25]. Gajdosik R, Passive extensibility of skeletal muscle: review of the literature with clinical implicationsClinical Biomechanics 2001 16(2):87-101.S0268-0033(00)00061-9 [Google Scholar] [CrossRef]
[26]. De Sampaio TF, de Nogueira , de Aguiar KP, Pontes TB, de Toledo AM de, Motor behavior of low birth weight and very low birth weight premature infantsFisioterapia e Pesquisa 2015 22(3):253-60. [Google Scholar]
[27]. Silva E, Nunes M, The influence of gestational age and birth weight in the clinical assesment of the muscle tone of healthy term and preterm newbornsArquivos de Neuro-Psiquiatria 2005 63(4):956-62.10.1590/S0004-282X200500060001016400412 [Google Scholar] [CrossRef] [PubMed]
[28]. Schonhaut L, Armijo I, Perez M, Gestational age and developmental risk in moderately and late preterm and early term infantsPediatrics 2015 135(4):e835-41.10.1542/peds.2014-195725733752 [Google Scholar] [CrossRef] [PubMed]
[29]. Vungarala P, Rajeswari M, Correlation of birth weight, gestational age and muscle tone with motor development of preterm infantsInternational Journal of Physiotherapy 2018 5(2)10.15621/ijphy/2018/v5i2/170744 [Google Scholar] [CrossRef]
[30]. Atik A, Ozyurek S, Flexible flatfootNorth Clin Istanbul 2014 1(1):57-64.10.14744/nci.2014.2929228058304 [Google Scholar] [CrossRef] [PubMed]
[31]. Miller M, The bone disease of preterm birth: a biomechanical perspectivePediatric Research 2003 53(1):10-15.10.1203/00006450-200301000-0000512508075 [Google Scholar] [CrossRef] [PubMed]
[32]. Atun-Einy O, Berger S, Scher A, Pulling to stand: Common trajectories and individual differences in developmentDevelopmental Psychobiology 2011 54(2):187-98.10.1002/dev.2059321815138 [Google Scholar] [CrossRef] [PubMed]
[33]. Svoboda Z, Janura M, Kutilek P, Janurova E, “Relationships between movements of the lower limb joints and the pelvis in open and closed kinematic chains during a gait cycle.”J Hum Kinet 2016 51:37-43.10.1515/hukin-2015-016828149366 [Google Scholar] [CrossRef] [PubMed]