The plaque bacteria colonising the teeth are vital for the dental caries and periodontal disease initiation [1]. Several hundred of bacterial species colonise the hard and soft tissue surfaces of oral cavity and the tongue; contributes to major portion of bacteria found in saliva and plaque. Further, the morphology of the dorsum of tongue being papillary provides a niche for these microorganisms and oral debris. The bacteria that are attached to each cell of tongue is four times more than in other intraoral sites [2]. A positive correlation between the number of mutans streptococci colonies on dorsal surface of the tongue and saliva has been reported [3].
The reduction in bacterial counts due to tooth brushing alone is not substantial. Tongue cleaning is gaining popularity as it has been proposed to reduce the counts of cariogenic bacteria in saliva more than tooth brushing [4].
Although dental caries is multifactorial in nature; studies have proved that, MS colonisation and consequent plaque accumulation on dental surfaces is the main causative factor [5,6]. The higher the level of MS, the higher is the plaque accumulation and the greater is the risk of developing carious lesions [6].
The important objective of caries prevention is controlling the levels of MS. Various mechanical and chemical plaque control measures are available for the same. Although toothbrushing is the most dependable oral hygiene measure, its effectiveness is limited by lack of motivation and manual dexterity. Recently, chemotherapeutic treatment regimens have received much attention and have presented satisfactory results in promoting MS suppression, plaque reduction, thereby leading to caries prevention or decreasing its incidence [7].
Oral rinsing with chemotherapeutic agents is known to inhibit plaque growth and maintain gingival health [8], but is not without any shortcomings [9]. It disrupts the bacterial cell membrane and increases the permeability thereby leading to cell lysis. However, when used as an oral rinse, there have been no reports of systemic toxicity and microbial resistance, and even suprainfections do not occur [10].
A natural sugar substitute like Xylitol has an edge over cariogenic sugars in caries prevention as it cannot be metabolised by oral bacteria [11]. Its inhibitory action on the growth of salivary and plaque S. mutans is an intracellular energy consuming futile cycle causing breakdown of energetic phosphate turnover [12].
Numerous mouth rinses are available in the market; each one claiming success over other and the new plethora of herbal mouth rinses are now gaining popularity [13]. A newly introduced herbal antimicrobial mouth rinse, HiOra, has been reported to be having antiseptic, antiviral, antifungal, anticoagulant, antioxidant and anesthetic properties. Its antimicrobial activity is related to the volatile oil of clove present in it [14].
Hence, the present study was conducted to evaluate and compare the adjunctive effect of tongue brushing and mouth rinsing (0.2% chlorhexidine gluconate, Hiora and xylitol) in addition to regular tooth brushing on the salivary MS colony forming units.
Materials and Methods
The present study was a single blind stratified random comparison done in the Department of Pedodontics and Preventive Dentistry, NIMS Dental College, Jaipur in conjunction with the Department of Microbiology, NIMS University. After performing an oral examination and reviewing the available medical records, forty-eight school going children aged 9 to 12 years were selected for the study who did not have more than four decayed, restored and missing teeth; performed tooth brushing twice daily; were not currently involved in any caries prevention trial/home based or professional oral hygiene measures; did not consumed antibiotic or were not hospitalised during past one month; had accepted the treatment regimen and cooperated actively; did not require emergency dental treatment such as abscess, draining sinuses or any other condition; had no known history of allergy or adverse reaction to materials used in the study or any transmissible disease or medical condition that might interfere with the study.
The sample size was calculated using the mean and standard deviation from the previous literature with similar variables and parameters [15,16]. Clinical assessments were performed by a single examiner in a well-equipped dental setup. A trained assistant helped the examiner in recording the forms. To ensure that at no time the examiner was aware of the group assignment of any child, the selected children were coded from 1 to 48 prior to clinical examination. After the investigation, the data was again recoded.
At each visit, questioning of children and intraoral examination of soft tissues, oropharynx, lips and teeth was carried out to ensure that there was no adverse reactions such as desquamation, unpleasant taste or extrinsic staining. A correlation was made as to whether these lesions are caused as an idiosyncratic reaction to any of the test materials.
The number of tooth surfaces involved with caries or missing or filled in both primary and permanent dentitions were recorded using Oral Health Assessment Form for Children for dental caries advocated by WHO in 2013 [17].
After explaining the nature of the study and its possible risks, consent was obtained from children verbally and from parent or guardian through a written consent form. The University ethical committee approval was obtained for the study. The selected children were advised not to undergo any other preventive or restorative dental care during the course of study and continue their routine of tooth brushing twice-daily.
During the Pre-evaluation period, all the children received new toothbrushes and toothpastes (Colgate® Total) and were trained to use the proper tooth brushing technique and tongue brushing for one week period.
Prior to the beginning of the phase I of the study, the children underwent oral prophylaxis to ensure that all visible dental plaque was removed. The baseline levels of mutans streptococci CFU’s in saliva were recorded. The children were asked to refrain from eating/drinking for at least two hours following which the stimulated whole saliva samples were obtained by making the children bite on paraffin wax for two minutes. These salivary samples were obtained in the mid-morning in sterile bottles. The samples were cultured within half an hour and subjected to microbiological analysis. The obtained sample was vortexed for 30 seconds vigorously. This ensured a good representative sample mixture before the process of preparation of dilutions and plating. Prior to the study, baseline mutans streptococci levels were established for each child.
Mitis Salivarius Bacitracin (MSB) agar was the media used to culture salivary mutans streptococci. About ninety grams of Mitis Salivarius dehydrated agar was added to 1 litre of distilled water and boiled to dissolve completely. To this, 20 grams of sucrose per 100 mL was added. This solution was then sterilized by autoclaving for 15 minutes at 15 pounds at 121°C. After autoclaving, the solution was allowed to cool to 50°C. Potassium tellurite and bacitracin were added to get the desired concentration in terms of mg per mL as 0.1 and 0.2 units respectively. It was then mixed well and poured into sterile petriplates and allowed to solidify.
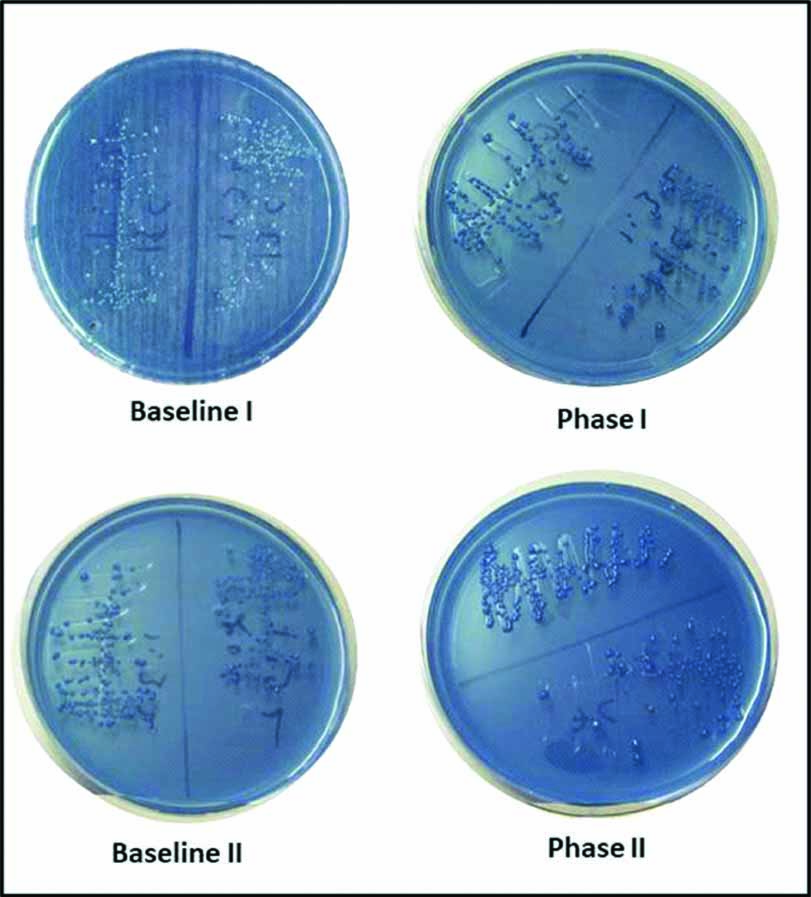
Using a standard 100 μL pipette, 100 μL of the vortexed sample was pipetted out. Serial dilutions (10-1, 10-2, 10-3, 10-4, 10-5) were then prepared on inoculating hood. From each of the dilutions 10 μL volume was inoculated on separate agar plates and made to spread evenly on to the agar surface using sterile disposable loop. Incubation of plates was then carried out at 37°C under 5-10% Carbon dioxide for 48 hours. The processing and examination of all plates was performed by the same investigator to avoid operator induced bias. Identification of colonies of mutans streptococci was done as follows: spherical or round, convex, black, raised with a rough surface, pinpoint to pinhead size [Table/Fig-1]. The colony count of each plate was noted. The mean colony forming units per mL was calculated as a product of colony count of each plate and its respective dilution factor.
Spherical or round, convex, raised colonies of mutans streptococci.
Following baseline scoring, 48 children meeting the inclusion criteria of the study were selected and were distributed to different groups using the lottery method with an equal allocation ratio and assigned to one of the below mentioned groups (12 children).
Group I- Control group: distilled water as mouthwash
Group II- Chlorhexidine gluconate mouthwash (0.2%) group
Group III- HiOra mouthwash group
Group IV- Xylitol mouthwash group
The mouthwashes were used twice daily for one week under professional supervision using 10 mL of respective mouthwash for one minute (morning after breakfast and just prior to sleeping at night). It was made sure that children followed the prescribed method of use of mouthwash without swallowing it and they were reinforced to follow the same method during the entire study period. The tooth brushing was also performed twice daily; morning prior to breakfast and at night immediately after dinner. A minimum of one hour duration between tooth brushing and mouth rinsing was maintained. After seven days, the phase-I salivary mutans streptococci CFU’s were recorded.
A wash-out period of one week was planned during which all the children enrolled in the study were asked to follow twice daily tooth brushing. They refrained from any other method of oral hygiene practices.
Following wash-out period, the participants were again subjected to oral prophylaxis and the second baseline salivary MS CFU was estimated.
The phase-II evaluation was then carried out. The tongue brushing was performed twice daily for a maximum duration of one minute (as trained in the preparatory period to ensure clean tongue surface) using the same tooth brush allotted to the child. All the participants continued with their respective mouth rinsing and tooth brushing twice daily. After a week, the salivary mutans streptococci CFU’s were again recorded.
Statistical Analysis
All the values of salivary mutans streptococci CFU’s obtained were recorded in Microsoft Excel (Microsoft, Redmond, WA, USA) and the comparative evaluation of the effect of 0.2% chlorhexidine gluconate, Hiora and xylitol mouth rinses on the salivary MS colony forming units were performed using IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY, USA (Released 2012.). Paired t-test or Dependent sample t-test was used for intragroup comparison. The intergroup comparison of salivary mutans streptococci was done by Unpaired t-test of Independent sample t-test and then ANOVA followed by Post-hoc Bonferroni test.
Results
The [Table/Fig-2] shows the sample characteristics of the study population. The inclusion of tongue brushing significantly reduced the salivary MS CFU’s only in the control group but not in experimental mouthwash groups [Table/Fig-3]. This suggests that mouth rinsing alone is effective in reducing the salivary MS CFU’s and performing tongue brushing in addition to mouth rinsing does not significantly reduce MS levels in saliva.
Sample characteristics of the study population.
| Groups | Mean and Standard deviation values |
|---|
| Age | No. of teeth | dmft/DMFT | dmfs/DMFS |
|---|
| Group I N=12 | 10.58±1.311 | 25.58±2.065 | 1/0.5 | 1.75/0.58 |
| Group II N=12 | 11±1.206 | 26.58±1.88 | 1.08/0.33 | 2.08/0.33 |
| Group III N=12 | 10.75±1.215 | 25.67±1.215 | 0.92/0.42 | 2/0.41 |
| Group IV N=12 | 10.08±1.164 | 24.25±0.621 | 1.33/0.42 | 2.08/0.42 |
dmfs, decayed missing filled surfaces of primary teeth;
DMFS, decayed missing filled surfaces of permanent teeth
The intragroup comparison of change in salivary mutans streptococci CFU after post-mouth rinsing and post-mouth rinsing+tongue brushing.
| Groups | Mean and Standard deviation values of salivary mutans streptococci CFU |
|---|
| Baseline I | Post mouth rinsing | Change in MS CFU I | Baseline II | Post mouth rinsing and Tongue brushing | Change in MS CFU II | p-value |
|---|
| I | 4.9806 | 4.9615 | -0.01903 | 4.9691 | 4.9146 | -0.05443 | 0.009 |
| II | 4.8155 | 4.5836 | -0.23185 | 4.6821 | 4.3610 | -0.32108 | 0.191 |
| III | 5.2997 | 5.1941 | -0.10559 | 5.2601 | 5.1046 | -0.15541 | 0.102 |
| IV | 5.2713 | 5.0827 | -0.18865 | 5.2116 | 5.0884 | -0.12327 | 0.456 |
Significant at p<0.05. MS CFU, Mutans streptococci Colony forming Paired t-test or Dependent sample t-test for intragroup comparison of change in salivary mutans units
[Table/Fig-4] revealed that intergroup comparison was statistically significant in both phase I and phase II. Hence, the post hoc analysis was performed using Bonferroni test [Table/Fig-5]; which revealed that in phase I, CHX mouthwash significantly reduced salivary MS CFU’s when compared to tooth brushing alone. The other two mouthwashes (Hiora and Xylitol) showed similar results in reducing salivary MS CFU’s. In phase II, the CHX group significantly reduced MS CFU’s when compared to other groups. The other two experimental mouthwashes (Hiora and Xylitol) showed similar results in reducing salivary MS CFU’s when used along with tongue brushing.
The intergroup comparison of salivary mutans streptococci CFU [log values]. after post-mouth rinsing and post-mouth rinsing+tongue brushing.
| Groups | Mean and Standard deviation values of salivary mutans streptococci CFU |
|---|
| Baseline I | Post mouth rinsing | Change in MS CFU I [A]. | Baseline II | Post mouth rinsing and Tongue brushing | Change in MS CFU II [B]. |
|---|
| I | 4.9806 | 4.9615 | -0.01903 | 4.9691 | 4.9146 | -0.05443 |
| II | 4.8155 | 4.5836 | -0.23185 | 4.6821 | 4.3610 | -0.32108 |
| III | 5.2997 | 5.1941 | -0.10559 | 5.2601 | 5.1046 | -0.15541 |
| IV | 5.2713 | 5.0827 | -0.18865 | 5.2116 | 5.0884 | -0.12327 |
| p-value | 0.000 | 0.000 | 0.008 | 0.000 | 0.000 | 0.000 |
Significant at p<0.05. MS CFU, Mutans streptococci Colony forming units Unpaired t-test of Independent sample t-test for intergroup comparison of salivary mutans streptococci
Intergroup comparison of salivary mutans streptococci counts CFU’s (log values) post mouth rinsing and post mouth rinsing+tongue brushing.
| Groups | Salivary Mutans Streptococci CFU’S |
|---|
| Phase I Change in MS CFU | Phase II Change in MS CFU |
|---|
| p-value | p-value |
|---|
| I vs. II | 0.009 | 0.000 |
| I vs. III | 1.000 | 0.293 |
| I vs. IV | 0.057 | 1.000 |
| II vs. III | 0.299 | 0.011 |
| II vs. IV | 1.000 | 0.002 |
| III vs. IV | 1.000 | 1.000 |
Significant at p<0.05. MS CFU, Mutans streptococci Colony forming units ANOVA followed by Post-hoc Bonferroni test
Discussion
Dental plaque is a complex biofilm consisting of a variety of bacteria embedded in a polysaccharide matrix. Once colonised, the pioneer bacteria adhere and produce acidic environment which in due course along with series of micro-environment alterations progress to cavitations. Hence, the antibacterial property of dentifrices is vital as its ingredients which have antibacterial properties combat the microbes and reduce their colonisation on enamel surface [18].
It has been established that the number of MS in saliva is directly linked to its number colonised on hard and soft tissue surfaces that are the basis for salivary counting of MS [4,19]. A subject with low salivary MS count has a lower risk of developing carious lesions and the caries risk threshold is when colony forming units per millilitre of saliva is more than 105 [20]. The earlier the colonisation age, the higher is the caries rate of the child [21,22]. This suggests that timing of mutans streptococci infection in the mouth of children is critical.
The method and duration of tooth brushing, the level of parental involvement and manual dexterity of the child can determine the effectiveness of tooth brushing apart from the design of toothbrush. The efficiency of tooth brushing is lower in children aged less than 10 years due to the fact that they exhibit poor manual dexterity and also due to lack of motivation [23]. However, there are no conclusive evidences regarding the effectiveness of supervised tooth brushing on caries incidence [24].
Hence during the pre-study period of present study, all the children were trained with regard to correct tooth brushing technique (Modified bass method). Mescher KD et al., suggested that children aged eight years and above could master the skills required for brushing [25]. It is reported that as the age of the child increases, the caries risk also increases [26]. In the present study, age group of 9 to 12 years was chosen because late mixed dentition is considered as a period of high caries activity.
In the present study, stimulated salivary samples were obtained as it is more reliable compared to unstimulated saliva [21]. Subjects were refrained from eating or drinking for two hours prior to sample collection as this might alter the level of bacteria in the oral cavity. Mundorff SA et al., justified that the number of S. mutans in stimulated salivary sample describes the variation in caries better as compared to the bacterial count in plaque [27].
MSB agar was selected in this study to determine the growth of salivary MS because these bacteria grow in high sucrose concentration medium and are immune to bacitracin [20].
Mouthwashes not only inhibit the bacterial metabolic activity but also their adhesion and colonisation, thereby preventing bacterial and plaque growth [28]. Chlorhexidine is considered to be the “gold standard” antiplaque mouthwash due to its prolonged broad spectrum antimicrobial and plaque inhibitory potential [27]. It inhibits gram positive and negative organisms, fungi, facultative anaerobes and aerobes. Gram positive cocci especially MS seems to be sensitive to chlorhexidine which acts by binding to bacterial cell wall and affects its function [29].
In the present study, chlorhexidine mouthrinse was found to be as effective as HiOra or Xylitol mouth rinse in inhibiting MS (p>0.05). However, it significantly reduced MS when compared to tooth brushing alone. Xylitol mouthrinse was found to be effective in reducing the salivary MS CFU’s. It is reported that Xylitol reduces MS counts in plaque but it does not affect microbial composition of plaque or saliva. Decker EM et al., reported that xylitol/chlorhexidine combination inhibits streptococci more when compared with xylitol or chlorhexidine being used alone [30]. This synergistic action can be reserved for high caries risk children as it also reduces the transmission of MS from mother to child. The solution of either Chlorhexidine alone or in combination with xylitol is effective against both S. sanguis and S. mutans. However, S. sanguis is more sensitive to chlorhexidine alone, whereas S. mutans is more sensitive to combination of chlorhexidine and xylitol.
In the present study, it was observed that the inclusion of tongue brushing significantly reduced the salivary MS CFU’s only in the control group but not in experimental mouthwash groups. This suggests that mouth rinsing alone is effective in reducing the salivary MS CFU’s and performing tongue brushing in addition to mouth rinsing does not significantly reduce MS levels in saliva. Jacob KC et al., reported that though scraping or brushing the tongue were equally effective in lowering salivary mutans streptococci counts, however their effect on reducing plaque levels was not significant [31].
It is reported that both scraping and brushing the tongue efficiently and equally reduced plaque formation and salivary mutans streptococcus colonies [2,32].
Limitation
The present study has made an attempt to standardise factors relating to dental caries such as age, oral hygiene factors (aids, brushing technique), diet to an extent, caries risk and amount of plaque. However, these factors may not be well synchronised at all times in an individual; thereby making the situation more complex in choosing the suitable anti-caries agent.
Conclusion
Mouth rinsing alone is effective in reducing the salivary MS CFU’s and performing tongue brushing in addition to mouth rinsing does not significantly reduce MS levels in saliva. Chlorhexidine mouthwash significantly reduced salivary MS CFU’s when compared to tooth brushing alone. When tongue brushing was used as an adjuvant, it was observed that the chlorhexidine group significantly reduced MS CFU’s when compared to other groups.
The oral hygiene measures should be simple and easy to be successful in children. Research needs to be carried out to determine the substantivity of these mouth rinses and their effects on specific cariogenic bacteria to check the initiation and progression of caries in children.
dmfs, decayed missing filled surfaces of primary teeth;
DMFS, decayed missing filled surfaces of permanent teeth
Significant at p<0.05. MS CFU, Mutans streptococci Colony forming Paired t-test or Dependent sample t-test for intragroup comparison of change in salivary mutans units
Significant at p<0.05. MS CFU, Mutans streptococci Colony forming units Unpaired t-test of Independent sample t-test for intergroup comparison of salivary mutans streptococci
Significant at p<0.05. MS CFU, Mutans streptococci Colony forming units ANOVA followed by Post-hoc Bonferroni test