Introduction
Recently, it has been revealed that oral microbiota exert several effects on the general health in humans [1]. Investigations demonstrated a bunch of microbial complexes that possess systemic impact on the host via interfering with the immune host response and up-regulating host gene expression [2]. Different diseases such as Diabetes Mellitus (DM), Cardiovascular Diseases (CVD), obesity and periodontal diseases have been linked to alterations of the oral microbial ecosystems [3]. To date, researchers are still exploring the incidence of a variety of diseases and linking them to oral microbial dysbiosis in an attempt to seek for crucial therapeutic modalities [4]. It was reported that abnormalities of Nitric Oxide (NO) signaling pathways were coupled with higher risk to hypertension, CVD, reduced insulin sensitivity and obesity [1]. Recently, reduction of oral commensal flora by antiseptic mouthrinses was found to prevent endogenously generated nitrates from being converted to nitrite by their bactericidal effects [5]. As a result, the decreased nitrites due to bacterial unbalance can possess a direct lowering effect on the blood pressure [6]. Accordingly, it was suggested that excessive use of oral antiseptic mouthrinses might lead to cardiovascular events particularly in patients with high risk to cardiovascular diseases [7].
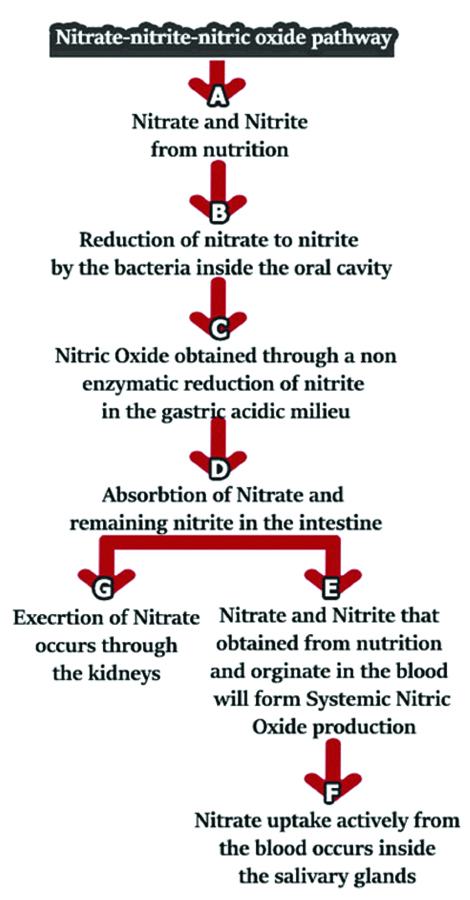
The ingested nitrates from dietary sources generate nitrite molecules by the action of microbial enzymes. Nitrites have been considered as a secondary source of NO as well as other forms of nitrogen oxides [8]. It was exhibited that nitrite metabolism plays a crucial role in maintaining the basal vascular tone and endothelial integrity, thus preserving normal blood pressure and preventing vasculitis during inflammatory stress conditions [9]. The NO metabolic pathway in addition to generated nitrites depends on the reduction of inorganic nitrate via specific bacteria which synthesise nitrate reductases (Naturally, are not present in humans) [10]. Dietary nitrates are readily absorbed after ingestion in the gastrointestinal tract via the nitrate-nitrite-NO pathway [Table/Fig-1] [11]. With regards to the total amount of dietary nitrate, about 25% of plasma nitrate is concentrated into the salivary glands to be secreted with whole salivary flow (It is 20-fold higher than in plasma concentration) [12]. It was previously reported that NO synthase and O2-independent enzymatic reductions convert salivary nitrates into nitrites in the oral cavity [13]. Then, nitrites are ingested and subjected to a series of successive reactions to produce NO and NO-donating molecules after protonation to HNO2 and a group of secondary nitrosating and nitrating molecules in the presence of low pH in the stomach [14], or reduction by intestinal bacterial nitrite reductase enzymes [15] thus, resulting in the formation of nitro-fatty acid signaling molecules such as NO2-conjugated linoleic acid and derivatives of S-nitrosothiol that could be detected at elevated plasma concentrations after oral nitrate ingestion [16]. These reactions can effectively regulate the cardiovascular functions and will cease after killing of the oral microbiota [17]. Based on the nitrate-nitrite-NO pathway, signal transduction leading to the generation of NO and bioactive nitrogen oxides will not progress to cGMP-dependent signaling and NO synthesis [18]. Thus, a wide spectrum of redox-derived nitrogen oxides induced post-translational modification of proteins with alterations in their function and gene expression profiles [19].
Diagrammatic illustration of nitrate-nitrite-nitric oxide pathway.
Vascular Health and Blood Pressure
The impaired nitrate-nitrite-NO pathway decreases the conversion of nitrate to nitrite and NO, which might lead to systemic complications, mainly in inflammatory and metabolic disorders [20]. A large body of evidence substantiates that bacterial activation of nitrate might play a major role in preventing and treating cardiovascular diseases [21]. Strong evidence has confirmed appreciated lowering blood pressure and improved vascular changes of nitrate and nitrite dietary supplementation [21]. Previous studies showed that using of chlorhexidine antiseptic mouthrinse resulted in reduction of oral bacterial nitrate reductases and thus reduction of 90% of concentrations of oral nitrite in humans associated with decrease in plasma levels significantly by 25% and increase in blood pressure by 2-3.5 mmHg [5]. Another study in hypertensive patients showed statistically significant blood pressure reduction with different nitrate supplementations [22]. Furthermore, the use of antimicrobial mouthwash reduced this valuable crucial effect [5]. It was reported that endothelial dysfunction has been linked to decreased plasma concentrations of nitrite [7]. It was proven that dietary supplementation with either nitrates or nitrites elevate systemic plasma nitrite levels and ameliorate the endothelial health in a dose-dependent pattern in a mouse model and obese individuals [23]. The same actions have been demonstrated in subjects with peripheral vascular disease and elevated plasma total cholesterol levels [21]. Furthermore, dietary nitrate and nitrite supplements showed significant inhibition of vascular intimal hyperplasia in mice [24], whereas nitrate supplementation reduced ischemia-reperfusion injury and endothelial dysfunction in different animal models and humans [25].
Complexity of the Oral Microbiome
It was previously reported that several billions of bacteria resides in the oral cavity; comprised of almost 700 different bacterial species [26]. A remarkable variability was found in the different sites in the oral cavity, such as gingiva, hard and soft palate, on dorsum of the tongue as well as the tooth surface [27]. It was established that specific types of bacterial flora have been associated with systemic and oral diseases [28]. For instance, bacterial species such as Streptococci and Lactobacilli were found to be involved in the dental carious lesions, whereas anaerobic gram negative bacteria such as species of Porphyromonas and Prevotella have been linked to periodontal diseases [29]. Recently, Porphyromonas gingivalis was revealed to be linked with atherosclerotic lesions, and certain types of cancer [30]. However, individual isolated bacterial strains do not exhibit any activity in a vacuum, they show virulence activity when present in microbial communities; they may have several oral and systemic health affections [31].
Periodontal Disease and Salivary Gland Dysfunction
Chronic periodontitis is a local chronic inflammation of the tooth supporting apparatus initiated by specific microorganisms including Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola, which are collectively known as the “red complex” [29]. It was revealed that periodontal tissue damage begins as inflammatory neutrophil mediated reaction followed by chronic infiltration of monocytes [32]. Previous investigations have reported that most of periodontal tissue destruction is directly caused by the host immune response to the aforementioned specific periodontopathogenic bacteria [33]. Nevertheless, Hajishengalis G and Lamont RJ have established a new model for periodontal disease pathogenesis exhibiting that periodontal disease is initiated by synergistic and dysbiotic periodontopathogens. In this polymicrobial synergy, different members in the microbial community perform specific roles to become a disease provoking microbiota. For a potentially pathogenic community to evolve, certain species, known as ‘keystone pathogens’, are able to modulate the host response by impairing the immune surveillance and tip the balance from symbiosis to dysbiosis [34].
Previous reports have revealed an association between cardiovascular diseases and periodontal disease which has been linked to direct vascular entry of the nitrate-reducing oral pathogenic bacteria, systemic inflammation, and endothelial dysfunction [35]. Conventional periodontal treatment by Scaling and Root Planing (SRP) in conjunction with or without chlorhexidine mouthwash has improved systemic inflammation [36]. Moreover, the levels of salivary nitrate and nitrite and gingival expression of NO have been found to be elevated in periodontal diseases, which increased with disease severity and improves after effective periodontal therapy [37]. It was shown that growth and survival of the nitrate-reducing bacteria inhabiting periodontal pockets and furcation areas can lead to pronounced imbalance of the oral micobiome [38]. Beside the aforementioned periodontal effects on bacterial communities, antimicrobial effects may also be exerted elsewhere in the buccal cavity and gastrointestinal tract as a result of high concentrations of salivary nitrite, possibly disrupting community composition or function of biologically beneficial communities of nitrate-reducing bacteria [39]. Based on the association between periodontal disease and other systemic diseases such as diabetes mellitus and obesity [40] the possibility of dysbiosis and systemic inflammation as a result of periodontal disease and general oral health might affect or reverse the valuable impacts on physiological salivary nitrate metabolism [39]. An additional association also was found between polymicrobial dysbiosis and salivary glands dysfunction which leads to xerostomia [41]. In salivary gland diseases, there is a reduction in salivary nitrate concentration and increase in urinary excretion, consequently diminishing the overall concentration of circulating nitrate [42]. Most importantly, several diseases which share increased pH and enhanced rates of vascular disease, including systemic sclerosis and Sjogren’s syndrome [43], HIV [44], and mucoviscidosis [45] also show dysregulated salivary flow and altered oral microbiota [46].
Conclusion
Some studies have reported that high blood pressure was associated with a reduced production and/or bioavailability of NO by oral microbiota. It was noticed that the dysreguation of the nitrate-nitrite-NO pathway through the use of antibacterial mouthrinses in treated hypertensive individuals was associated with a moderate elevation of systolic blood pressure. In fact, the clear mechanism is still to be identified. More future studies are warranted to explore whether different antibacterial agents present in mouthwashes have the same effect on blood pressure especially in patients with cardiovascular events.
[1]. Krishnan K, Chen T, Paster BJ, A practical guide to the oral microbiome and its relation to health and diseaseOral Diseases 2017 23(3):276-86.10.1111/odi.1250927219464 [Google Scholar] [CrossRef] [PubMed]
[2]. Takahashi D, Hase K, Commensal microbiota-derived signals regulate host immune system through epigenetic modificationsInflammation and Regeneration 2015 35(3):129-36.10.2492/inflammregen.35.129 [Google Scholar] [CrossRef]
[3]. Sansbury BE, Hill BG, Regulation of obesity and insulin resistance by nitric oxideFree Radical Biology and Medicine 2014 73:383-99.10.1016/j.freeradbiomed.2014.05.01624878261 [Google Scholar] [CrossRef] [PubMed]
[4]. Lundberg JO, Weitzberg E, Gladwin MT, The nitrate-nitrite-nitric oxide pathway in physiology and therapeuticsNature Reviews Drug Discovery 2008 7(2):15610.1038/nrd246618167491 [Google Scholar] [CrossRef] [PubMed]
[5]. Petersson J, Carlström M, Schreiber O, Phillipson M, Christoffersson G, Jägare A, Gastroprotective and blood pressure lowering effects of dietary nitrate are abolished by an antiseptic mouthwashFree Radical Biology and Medicine 2009 46(8):1068-75.10.1016/j.freeradbiomed.2009.01.01119439233 [Google Scholar] [CrossRef] [PubMed]
[6]. Gee LC, Ahluwalia A, Dietary nitrate lowers blood pressure: epidemiological, pre-clinical experimental and clinical trial evidenceCurrent Hypertension Reports 2016 18(2):1710.1007/s11906-015-0623-426815004 [Google Scholar] [CrossRef] [PubMed]
[7]. Hobbs DA, George TW, Lovegrove JA, The effects of dietary nitrate on blood pressure and endothelial function: a review of human intervention studiesNutrition Research Reviews 2013 26(2):210-22.10.1017/S095442241300018824134873 [Google Scholar] [CrossRef] [PubMed]
[8]. Lundberg JO, Weitzberg E, Biology of nitrogen oxides in the gastrointestinal tractGut 2013 62(4):616-29.10.1136/gutjnl-2011-30164922267589 [Google Scholar] [CrossRef] [PubMed]
[9]. Lara J, Ashor AW, Oggioni C, Ahluwalia A, Mathers JC, Siervo M, Effects of inorganic nitrate and beetroot supplementation on endothelial function: a systematic review and meta-analysisEuropean Journal of Nutrition 2016 55(2):451-59.10.1007/s00394-015-0872-725764393 [Google Scholar] [CrossRef] [PubMed]
[10]. Sobko T, Reinders CI, Jansson EÅ, Norin E, Midtvedt T, Lundberg JO, Gastrointestinal bacteria generate nitric oxide from nitrate and nitriteNitric Oxide 2005 13(4):272-78.10.1016/j.niox.2005.08.00216183308 [Google Scholar] [CrossRef] [PubMed]
[11]. McKnight GM, Smith LM, Drummond RS, Duncan CW, Golden MI, Benjamin N, Chemical synthesis of nitric oxide in the stomach from dietary nitrate in humansGut 1997 40(2):211-14.10.1136/gut.40.2.2119071933 [Google Scholar] [CrossRef] [PubMed]
[12]. Clodfelter WH, Basu S, Bolden C, Dos Santos PC, King SB, Kim-Shapiro DB, The relationship between plasma and salivary NOxNitric Oxide 2015 47:85-90.10.1016/j.niox.2015.04.00325910583 [Google Scholar] [CrossRef] [PubMed]
[13]. Fukuto JM, Carrington SJ, Tantillo DJ, Harrison JG, Ignarro LJ, Freeman BA, Small molecule signaling agents: the integrated chemistry and biochemistry of nitrogen oxides, oxides of carbon, dioxygen, hydrogen sulfide, and their derived speciesChemical Research in Toxicology 2012 25(4):769-93.10.1021/tx200523422263838 [Google Scholar] [CrossRef] [PubMed]
[14]. Vitturi DA, Minarrieta L, Salvatore SR, Postlethwait EM, Fazzari M, Ferrer-Sueta G, Convergence of biological nitration and nitrosation via symmetrical nitrous anhydrideNature Chemical Biology 2015 11(7):50410.1038/nchembio.181426006011 [Google Scholar] [CrossRef] [PubMed]
[15]. Tiso M, Schechter AN, Nitrate reduction to nitrite, nitric oxide and ammonia by gut bacteria under physiological conditionsPloS One 2015 10(3):e011971210.1371/journal.pone.011971225803049 [Google Scholar] [CrossRef] [PubMed]
[16]. Sparacino-Watkins C, Stolz JF, Basu P, Nitrate and periplasmic nitrate reductasesChemical Society Reviews 2014 43(2):676-706.10.1039/C3CS60249D24141308 [Google Scholar] [CrossRef] [PubMed]
[17]. Webb AJ, Patel N, Loukogeorgakis S, Okorie M, Aboud Z, Misra S, Nitric Oxide, Oxidative StressHypertension 2008 51(3):784-90.10.1161/HYPERTENSIONAHA.107.10352318250365 [Google Scholar] [CrossRef] [PubMed]
[18]. Cosby K, Partovi KS, Crawford JH, Patel RP, Reiter CD, Martyr S, Nitrite reduction to nitric oxide by deoxyhemoglobin vasodilates the human circulationNature medicine 2003 9(12):149810.1038/nm95414595407 [Google Scholar] [CrossRef] [PubMed]
[19]. Delmastro-Greenwood M, Hughan KS, Vitturi DA, Salvatore SR, Grimes G, Potti G, Nitrite and nitrate-dependent generation of anti-inflammatory fatty acid nitroalkenesFree Radical Biology and Medicine 2015 89:333-41.10.1016/j.freeradbiomed.2015.07.14926385079 [Google Scholar] [CrossRef] [PubMed]
[20]. Siervo M, Lara J, Ogbonmwan I, Mathers JC, Inorganic Nitrate and Beetroot Juice Supplementation Reduces Blood Pressure in Adults: A Systematic Review and Meta-AnalysisThe Journal of Nutrition 2013 143(6):818-26.10.3945/jn.112.17023323596162 [Google Scholar] [CrossRef] [PubMed]
[21]. Velmurugan S, Gan JM, Rathod KS, Khambata RS, Ghosh SM, Hartley A, Dietary nitrate improves vascular function in patients with hypercholesterolemia: a randomized, double-blind, placebo-controlled study-3The American Journal of Clinical Nutrition 2015 103(1):25-38.10.3945/ajcn.115.11624426607938 [Google Scholar] [CrossRef] [PubMed]
[22]. Kapil V, Khambata RS, Robertson A, Caulfield MJ, Ahluwalia A, Dietary nitrate provides sustained blood pressure lowering in hypertensive patients: a randomized, phase 2, double-blind, placebo-controlled studyHypertension 2015 65(2):320-27.10.1161/HYPERTENSIONAHA.114.0467525421976 [Google Scholar] [CrossRef] [PubMed]
[23]. Lee JS, Stebbins CL, Jung E, Nho H, Kim JK, Chang MJ, Effects of chronic dietary nitrate supplementation on the hemodynamic response to dynamic exerciseAmerican Journal of Physiology-Regulatory, Integrative and Comparative Physiology 2015 309(5):R459-66.10.1152/ajpregu.00099.201526084693 [Google Scholar] [CrossRef] [PubMed]
[24]. Alef MJ, Tzeng E, Zuckerbraun BS, Nitric oxide and nitrite-based therapeutic opportunities in intimal hyperplasiaNitric Oxide 2012 26(4):285-94.10.1016/j.niox.2012.03.01422504069 [Google Scholar] [CrossRef] [PubMed]
[25]. Kumar D, Branch BG, Pattillo CB, Hood J, Thoma S, Simpson S, Chronic sodium nitrite therapy augments ischemia-induced angiogenesis and arteriogenesisProc Natl Acad Sci U S A 2008 105(21):7540-45.10.1073/pnas.071148010518508974 [Google Scholar] [CrossRef] [PubMed]
[26]. Eren AM, Borisy GG, Huse SM, Welch JL, Oligotyping analysis of the human oral microbiomeProceedings of the National Academy of Sciences 2014 111(28):E2875-E2884.10.1073/pnas.140964411124965363 [Google Scholar] [CrossRef] [PubMed]
[27]. Segata N, Haake SK, Mannon P, Lemon KP, Waldron L, Gevers D, Composition of the adult digestive tract bacterial microbiome based on seven mouth surfaces, tonsils, throat and stool samplesGenome Biology 2012 13(6):R4210.1186/gb-2012-13-6-r4222698087 [Google Scholar] [CrossRef] [PubMed]
[28]. Xu X, He J, Xue J, Wang Y, Li K, Zhang K, Oral cavity contains distinct niches with dynamic microbial communitiesEnvironmental Microbiology 2015 17(3):699-710.10.1111/1462-2920.1250224800728 [Google Scholar] [CrossRef] [PubMed]
[29]. Wara-Aswapati N, Pitiphat W, Chanchaimongkon L, Taweechaisupapong S, Boch JA, Ishikawa I, Red bacterial complex is associated with the severity of chronic periodontitis in a Thai populationOral Diseases 2009 15(5):354-59.10.1111/j.1601-0825.2009.01562.x19371397 [Google Scholar] [CrossRef] [PubMed]
[30]. Duran-Pinedo AE, Frias-Lopez J, Beyond microbial community composition: functional activities of the oral microbiome in health and diseaseMicrobes and Infection 2015 17(7):505-16.10.1016/j.micinf.2015.03.01425862077 [Google Scholar] [CrossRef] [PubMed]
[31]. Chen H, Jiang W, Application of high-throughput sequencing in understanding human oral microbiome related with health and diseaseFrontiers in Microbiology 2014 5:50810.3389/fmicb.2014.0050825352835 [Google Scholar] [CrossRef] [PubMed]
[32]. Kantarci A, Van Dyke TE, Lipoxin signaling in neutrophils and their role in periodontal diseaseProstaglandins, Leukotrienes and Essential Fatty Acids 2005 73(3-4):289-99.10.1016/j.plefa.2005.05.01915979867 [Google Scholar] [CrossRef] [PubMed]
[33]. Van Dyke TE, Serhan CN, Resolution of inflammation: a new paradigm for the pathogenesis of periodontal diseasesJournal of Dental Research 2003 82(2):82-90.10.1177/15440591030820020212562878 [Google Scholar] [CrossRef] [PubMed]
[34]. Hajishengallis G, Lamont RJ, Beyond the red complex and into more complexity: the Polymicrobial Synergy and Dysbiosis (PSD) model of periodontal disease etiologyMolecular Oral Microbiology 2012 27(6):409-19.10.1111/j.2041-1014.2012.00663.x23134607 [Google Scholar] [CrossRef] [PubMed]
[35]. Fåk F, Tremaroli V, Bergström G, Bäckhed F, Oral microbiota in patients with atherosclerosisAtherosclerosis 2015 243(2):573-78.10.1016/j.atherosclerosis.2015.10.09726536303 [Google Scholar] [CrossRef] [PubMed]
[36]. Parwani SR, Chitnis PJ, Parwani RN, Salivary nitric oxide levels in inflammatory periodontal disease–A case-control and interventional studyInternational Journal of Dental Hygiene 2012 10(1):67-73.10.1111/j.1601-5037.2011.00508.x21564536 [Google Scholar] [CrossRef] [PubMed]
[37]. Wadhwa D, Bey A, Hasija M, Moin S, Kumar A, Aman S, Determination of levels of nitric oxide in smoker and nonsmoker patients with chronic periodontitisJournal of Periodontal & Implant Science 2013 43(5):215-20.10.5051/jpis.2013.43.5.21524236243 [Google Scholar] [CrossRef] [PubMed]
[38]. Sánchez GA, Miozza VA, Delgado A, Busch L, Total salivary nitrates and nitrites in oral health and periodontal diseaseNitric Oxide 2014 36:31-35.10.1016/j.niox.2013.10.01224211765 [Google Scholar] [CrossRef] [PubMed]
[39]. Hyde ER, Luk B, Cron S, Kusic L, McCue T, Bauch T, Characterization of the rat oral microbiome and the effects of dietary nitrateFree Radical Biology and Medicine 2014 77:249-57.10.1016/j.freeradbiomed.2014.09.01725305639 [Google Scholar] [CrossRef] [PubMed]
[40]. Han K, Park JB, Age threshold for moderate and severe periodontitis among Korean adults without diabetes mellitus, hypertension, metabolic syndrome, and/or obesityMedicine 2017 96(33):e783510.1097/MD.000000000000783528816984 [Google Scholar] [CrossRef] [PubMed]
[41]. Xia DS, Deng DJ, Wang SL, Destruction of parotid glands affects nitrate and nitrite metabolismJournal of Dental Research 2003 82(2):101-05.10.1177/15440591030820020512562881 [Google Scholar] [CrossRef] [PubMed]
[42]. Xia D, Deng D, Wang S, Alterations of nitrate and nitrite content in saliva, serum, and urine in patients with salivary dysfunctionJournal of Oral Pathology & Medicine 2003 32(2):95-99.10.1034/j.1600-0714.2003.00109.x [Google Scholar] [CrossRef]
[43]. Ratjen F, Pulmonary artery hypertension: an underrated disease manifestation in cystic fibrosis?The Lancet Respiratory Medicine 2016 4(8):596-98.10.1016/S2213-2600(16)30107-2 [Google Scholar] [CrossRef]
[44]. Navazesh M, Mulligan R, Pogoda J, Greenspan D, Alves M, Phelan J, The effect of HAART on salivary microbiota in the Women’s Interagency HIV Study (WIHS)Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2005 100(6):701-08.10.1016/j.tripleo.2004.10.01116301151 [Google Scholar] [CrossRef] [PubMed]
[45]. da Silva Modesto KB, de Godói Simões JB, de Souza AF, Damaceno N, Duarte DA, Leite MF, Salivary flow rate and biochemical composition analysis in stimulated whole saliva of children with cystic fibrosisArchives of Oral Biology 2015 60(11):1650-54.10.1016/j.archoralbio.2015.08.00726351748 [Google Scholar] [CrossRef] [PubMed]
[46]. Li M, Zou Y, Jiang Q, Jiang L, Yu Q, Ding X, A preliminary study of the oral microbiota in Chinese patients with Sjögren’s syndromeArchives of Oral Biology 2016 70:143-48.10.1016/j.archoralbio.2016.06.01627351333 [Google Scholar] [CrossRef] [PubMed]