Idiopathic Charcot’s Arthropathy of Ankle Joint: A Rare Case
Rohan Somani1, Pratik Panda2, Mayank Dungarwal3, Suvarn Gupta4, Pratik Kawde5
1 Student, Jawaharlal Nehru Medical College, Sawangi, Maharashtra, India.
2 Student, Jawaharlal Nehru Medical College, Sawangi, Maharashtra, India.
3 Student, Jawaharlal Nehru Medical College, Sawangi, Maharashtra, India.
4 Assistant Professor, Department of Orthopaedics, Jawaharlal Nehru Medical College, Sawangi, Maharashtra, India.
5 Junior Resident, Department of Orthopaedics, Jawaharlal Nehru Medical College, Sawangi, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pratik Kawde, Khati Chowk, Virani Hall Road, Near Shri Ram Mandir, Wani-445304, Maharashtra, India.
E-mail: kwdepratik@yahoo.in
Charcot’s Arthropathy also known as Neuropathic Joint of ankle in a non-diabetic patient is a rare entity. We identified similar case who presented to us with the swelling over left ankle and foot with a discharging sinus. On further evaluation with X-ray and Magnetic Resonance Imaging (MRI), diagnosis of Charcot’s arthropathy was made. Initially patient was managed with conservative trial and later arthrodesis of left ankle joint was done. Postoperatively, patient had pain relief and was on full weight bearing with regression of symptoms.
Bone resorption, Degenerative arthropathy, Neurological defects, Neuropathic joint
Case Report
A 72-year-old non diabetic female presented with diffuse progressive swelling and instability with restricted movements over the left ankle joint since 2 years. The patient also complains of a discharging sinus present over the lateral aspect of left ankle joint [Table/Fig-1] with seropurulent non-foul smelling discharge since 2 years. On local examination, the temperature was raised with tenderness and redness over the affected site. Physical examination revealed grossly restricted dorsiflexion and plantar flexion and movements at the subtalar joint were also restricted. On CNS examination higher mental function, cranial nerves were normal. Deep tendon reflex at left ankle joint were diminished. Sensory system examination revealed loss of superficial sensations over the ankle and dorsum of left foot and there was no motor loss in muscles around ankle joint. Consent was obtained from patient and her husband for publication of this case.
Clinical image of anterior and lateral aspect of left ankle and foot (Arrow pointing discharging sinus).

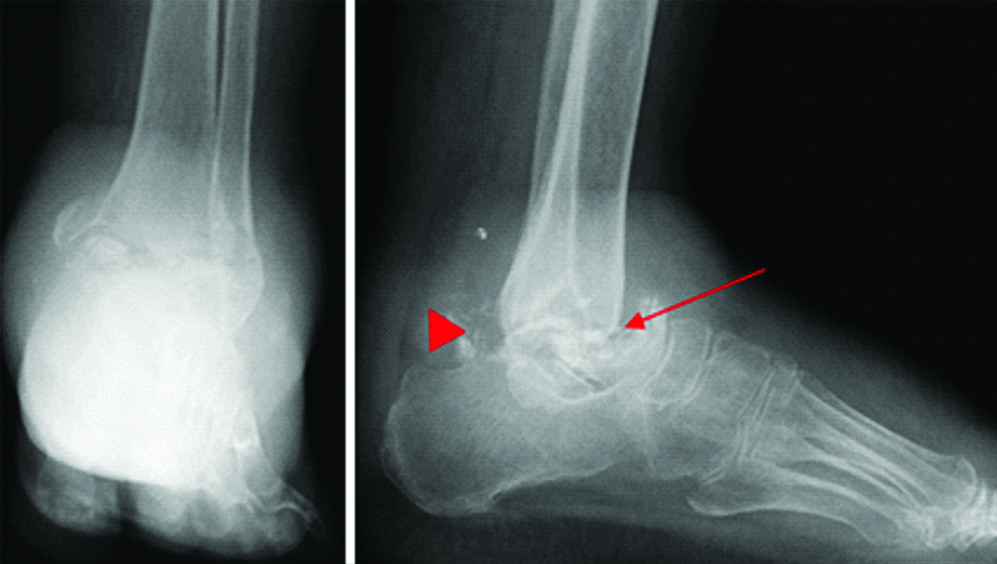
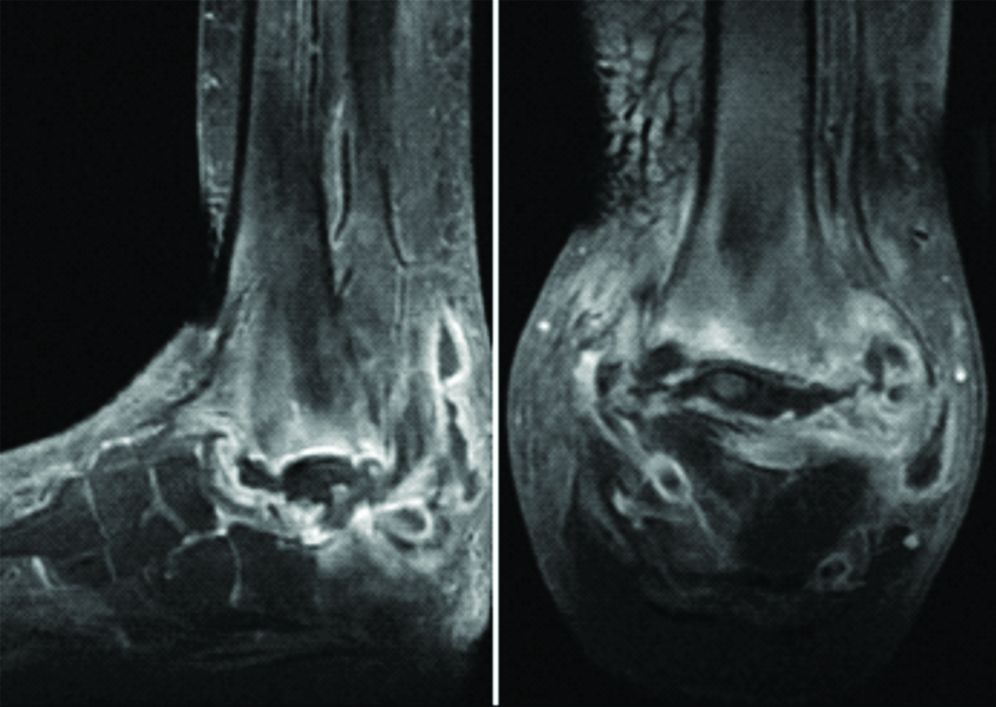
Further investigations revealed normal hemogram, urine analysis and blood sugar. Culture showed growth of coagulase positive staphylococci. Nerve conduction velocity study showed severe generalised sensory motor axonal polyneuropathy. X-ray picture of left ankle revealed complete resorption of talus, loose bodies (osteophytes) around ankle joint and osteopenia and subluxation of ankle joint, with complete obliteration of joint space [Table/Fig-2]. MRI of the left ankle revealed non-visualisation of neck and body of talus with loss of tibiotalar and talocalcaneal joint space. Cortical irregularity and diffused subcortical marrow oedema was noted in the distal end of tibia and calcaneum, distal fibula and head of talus. Findings also revealed marked synovial thickening with heterogeneous enhancement and loculated peripherally enhancing fluid pockets in ankle joint, subtalar joint and distal tibio-fibular joint with surrounding soft tissue oedema [Table/Fig-3]
X-ray left ankle Antero-posterior and lateral view shows complete resorption of talus (arrow), osteophytes (arrow head) around ankle joints, osteopenia and subluxation.
Saggital and coronal magnetic resonance image.
On the basis of clinical findings like painless instability of left ankle and radiographic evaluation showing destruction of left ankle, talar resorption, with multiple loose bodies, oedema in distal end of tibia and calcaneum and as the aetiology could not be explored, the case was diagnosed as idiopathic charcot’s arthropathy of the left ankle joint.
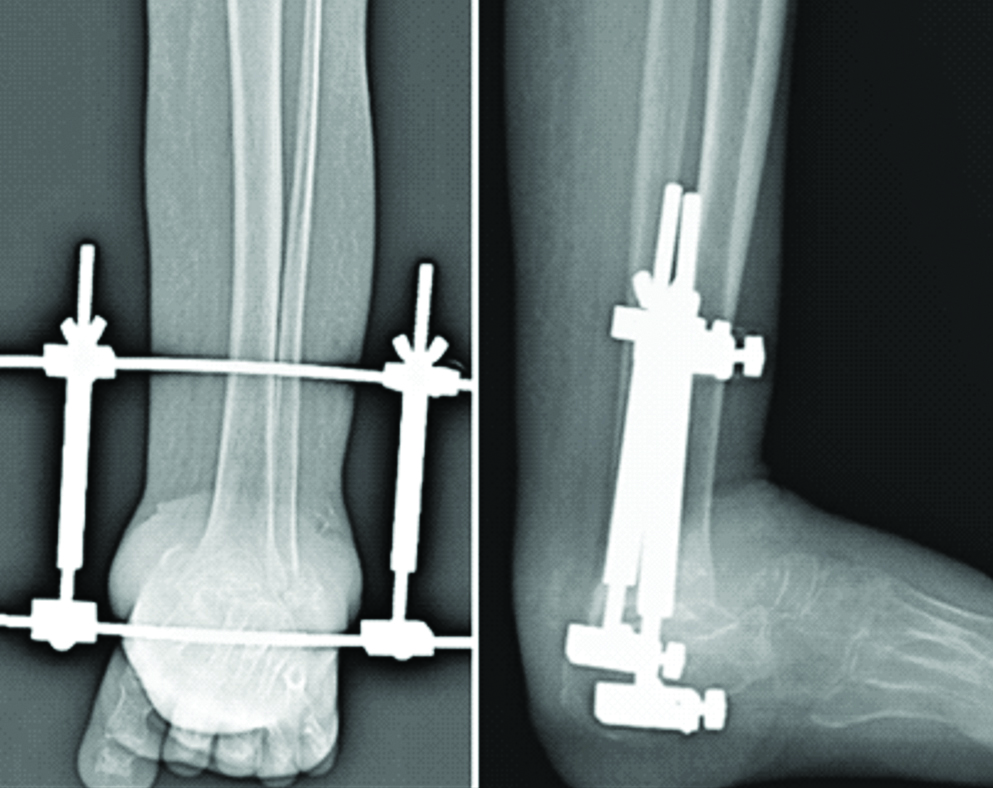
As the primary cause of illness was unknown so the patient was given broad spectrum antibiotic therapy in the form of injection Ceftriaxone 1 gm (cephalosporin) intravenous twice daily for 5 days and conservative treatment with Total Contact Cast (TCC) which is primarily based on immobilisation. At four months follow-up, TCC was removed and arthrodesis of left ankle joint was done using Charnley’s clamps [Table/Fig-4]. Post-surgery patient was kept non-weight bearing for three weeks. Also, due to presence of external fixation device (Charnley’s clamps), patient complained of some discomfort in her daily activities. Patient has improved symptomatically and clinically swelling subsided and discharging sinus was healed at 15 days follow-up.
Post-operative anteroposterior and lateral view of left ankle joint.
Discussion
Neuropathic joint disease (Charcot’s joint) is a progressive destructive arthritis associated with loss of pain sensation, proprioception or both, normal muscular reflex that modulate joint movement are impaired. Without these protective mechanism, joints are subjected to repeated trauma resulting in progressive cartilage and bone damage [1]. It is characterised by bony disruption, bone resorption and eventual deformity. This condition is most frequently seen with Diabetes mellitus. Other causes associated with neuropathic arthritis include tabes dorsalis, leprosy, syringomyelia, yaws, amyloidosis etc., [2]. There are two underlying mechanism: Neurotraumatic theory and Neurovascular theory. Neurotraumatic theory states that the somatic muscular reflexes normally prevent joint from exceeding specific safe limits. Ranges of movements are degraded by account of absent or decreased sensation which is then subjected to repeated sub clinical trauma and thereby joint destruction and according to Neurovascular theory, the underlying condition leads to development of autonomic neuropathy causing the extremity to receive an increased blood flow [3,4].
Radiologically, Charcot joint is of two types [5]: Atrophic: Licked candy stick appearance commonly seen at distal aspect of metatarsals. There is bone resorption and osteolysis. It is usually localised to forefoot and hypertrophic in which joint distention is seen and the joint density increases. Also, there is debris production, joint dislocation and destruction.
The diagnosis is based on patient’s history, clinical examination and radiological imaging methods. The patient of charcot’s joint present with warm, swollen, red foot or ankle without pain. Another clinical feature of Charcot’s arthropathy in the diagnosis is presence of crepitus or grinding in the involved joint. In some cases, plantar ulcers may be seen which makes it difficult to distinguish it from osteomyelitis. In such cases, synovial and bone biopsies may be necessary for definitive diagnosis [6,7]. During the initial stage, X-ray findings can be negative or only minor bone infractions and joint incongruence projection may be seen. In a developed stage fractures and subluxations or luxations are clearly observed with osteophytes around the joint and osteopenia [8]. Examination using MRI is a very valuable method for early stages of illness when X-ray imaging alone results in practical normal findings. An important finding is oedema of the bone marrow of two or more bones, oedema of adjacent soft tissues, and fluid accumulation in several joints or cortical fractures [9]. All in all, the symptoms observed in our patient were in line with the above description.
The treatment of Charcot’s joint is mostly conservative. This method is primarily based on immobilisation and complete absence of weight bearing for the affected extremities in the active stage [10]. The most commonly used methods of immobilisation are TCC which is done in active phase when swelling and erythema are present upto four months [11] and CROW which is recommended after resolution of swelling and erythema and achieving radiographic stability. This device is used for six months to two years until a stable foot is obtained [12].
Only after failure of conservative management, a patient becomes a candidate for surgical treatment [13]. The commonly employed surgical procedures include Exostectomy of Bony prominence; Arthrodesis: It is used in patients with tibiotalar destruction; and Open Reduction and Internal Fixation (ORIF): It is used for an ankle with displaced fractures [14]. In our study, the treatment strategy employed emphasised mostly by conservative methods that included restricted weight bearing, immobilisation, antibiotic therapy and nonsteroidal anti-inflammatory medication. Early recognition and treatment is crucial for good prognosis in such cases [15].
Physicians should always educate their patients about the proper care of the neuropathic foot and the use of orthotic devices or custom footwear. Early identification and treatment of charcot process can minimise the foot deformity, ulceration and loss of function and prevents amputation.
Conclusion
The most common cause of Charcot arthropathy is polyneuropathy secondary to diabetes mellitus, syringomylia, leprosy, etc., but it can be idiopathic also. The clinical picture, i.e., oedema, redness, increased skin temperature and painless instability at ankle joint with X-ray and MRI findings of severe destruction of ankle joint, talar resorption and osteophytes was helpful in diagnosis of the patient. The treatment of Charcot’s joint is mostly conservative with immobilisation and absence of weight bearing for the affected extremities in the active stage. Only after failure of conservative management a patient becomes a candidate for surgical treatment.
[1]. Frykberg RG, Belczyk R, Epidemiology of the charcot footClinics in Podiatric Medicine and Surgery 2008 25(1):17-28.10.1016/j.cpm.2007.10.00118165108 [Google Scholar] [CrossRef] [PubMed]
[2]. Stuck RM, Sohn MW, Budiman-Mak E, Lee TA, Weiss KB, Charcot arthropathy risk elevation in the obese diabetic populationThe American Journal of Medicine 2008 121(11):1008-14.10.1016/j.amjmed.2008.06.03818954849 [Google Scholar] [CrossRef] [PubMed]
[3]. Armstrong DG, Todd WF, Lavery LA, Harkless LB, Bushman TR, The natural history of acute Charcot’s arthropathy in a diabetic foot specialty clinicJournal of the American Podiatric Medical Association 1997 87(6):272-78.10.7547/87507315-87-6-2729198348 [Google Scholar] [CrossRef] [PubMed]
[4]. Harrelson JM, The diabetic foot: Charcot arthropathyInstructional Course Lectures 1993 42:141 [Google Scholar]
[5]. Munson ME, Wrobel JS, Holmes CM, Hanauer DA, Data mining for identifying novel associations and temporal relationships with Charcot footJournal of Diabetes Research 2014 2014:21435310.1155/2014/21435324868558 [Google Scholar] [CrossRef] [PubMed]
[6]. Rajbhandari S, Jenkins RD, Davies C, Tesfaye S, Charcot neuroarthropathy in diabetes mellitusDiabetologia 2002 45(8):1085-96.10.1007/s00125-002-0885-712189438 [Google Scholar] [CrossRef] [PubMed]
[7]. Lipsky BA, Osteomyelitis of the foot in diabetic patientsClinical Infectious Diseases 1997 25(6):1318-26.10.1086/5161489431370 [Google Scholar] [CrossRef] [PubMed]
[8]. Yanık B, Tuncer S, Seçkin B, Neuropathic arthropathy caused by Arnold-Chiari malformation with syringomyeliaRheumatology International 2004 24(4):238-41.10.1007/s00296-003-0389-x14648112 [Google Scholar] [CrossRef] [PubMed]
[9]. Johnson JT, Neuropathic fractures and joint injuries: Pathogenesis and rationale of prevention and treatmentJBJS 1967 49(1):1-30.10.2106/00004623-196749010-00001 [Google Scholar] [CrossRef]
[10]. Bramham R, Wraight P, May K, Management of charcot neuroarthropathyDiabetic Foot Journal 2011 14(4) [Google Scholar]
[11]. Sinacore DR, Acute Charcot arthropathy in patients with diabetes mellitus: healing times by foot locationJournal of Diabetes and its Complications 1998 12(5):287-93.10.1016/S1056-8727(98)00006-3 [Google Scholar] [CrossRef]
[12]. Mehta JA, Brown C, Sargeant N, Charcot restraint orthotic walkerFoot & Ankle International 1998 19(9):619-23.10.1177/107110079801900909 [Google Scholar] [CrossRef]
[13]. Adams SR, Lee RM, Leibowitz M, Charcot NeuroarthropathyProceedings of UCLA Healthcare 2014 :18 [Google Scholar]
[14]. Lowery NJ, Woods JB, Armstrong DG, Wukich DK, Surgical management of charcot neuroarthropathy of the foot and ankle: A systematic reviewFoot & Ankle International 2012 33(2):113-21.10.3113/FAI.2012.011322381342 [Google Scholar] [CrossRef] [PubMed]
[15]. Frykberg RG, Mendeszoon E, Management of the diabetic charcot footDiabetes/Metabolism Research and Reviews 2000 16(S1):S59-65.10.1002/1520-7560(200009/10)16:1+<::AID-DMRR134>3.0.CO;2-N [Google Scholar] [CrossRef]