Head and neck neoplasms are often referred to as areas more commonly inclusive of the upper aerodigestive tract, which includes the oral cavity, pharynx, larynx, cervical oesophagus, paranasal sinuses, thyroid, the associated bone and soft tissues, along with nodes. In the head and neck area, amongst the various mesenchymal tumours, schwannoma form a major portion, accounting for not less than 25% to 45% of tumours. Laryngeal schwannoma arising in the glottis area of the larynx is an extremely rare entity. It arises from the nerves supplying the organ and despite having a benign growth pattern; the schwannomas can pose extreme diagnostic as well as operative complexity. The strategic location of the larynx with its special functioning can both be hurdles in management of even such benign tumours like schwannoma, resulting in considerable post operative sequel. Here, we report a case of 30-year-old female with chief complaints of severe dyspnea and dysphonia. On radiological as well as histopathological examination, diagnosis of schwannoma was confirmed.
Case Report
A 30-year-old woman presented to the casualty with chief complaint of severe dyspnea, which has exacerbated over a week’s time prior to which she did have the same complaint for the past six months but of modest proportions. The patient also presented with near complete loss of speech (severe dysphonia) along with altered voice quality (hoarse, rough) with occasions of diplophonia since the past one year. She did not have a history of smoking or alcohol intake; however she does give history of tobacco and betel nut chewing for the past eight years.
In casualty, the physician and the anesthetist were called in for vital stabilisation and intubation. Since vocal cords were not visualised, intubation was unsuccessful. Otorhinolaryngologist was subsequently called for and an emergency tracheostomy was carried out as SpO2 had dropped to 60 mmHg. Once the patient’s vitals were stabilised, she was shifted to the ENT ward. On day two, Otorhinolaryngology examination was done and she was found to be severely dyspnoic with evidence of hoarseness of voice and stridor. Examination showed that the patient used the accessory muscles during phonation as well as breathing. There was no cervical lymphadenopathy and systemic examination was within normal limits. Direct laryngoscopy was carried out where the vocal cords could not be visualised however; it revealed an expansive solid well-circumscribed oval lesion arising from left aryepiglottic fold upto the level of the cricoid cartilage. The lesion was midline extending in both halves of the larynx, almost completely occluding the glottis and the subglottis. A biopsy was carried out; the histopathology report suggested an unremarkable fibrous tissue, probably from the capsule of the lesion. The report highlighted that the biopsy was not representative of the tumour tissue. Subsequently, a Contrast Enhanced Computed Tomography was carried out which showed a well defined, hypoattenuating expansile mass with heterogeneous enhancement of size 3.5 cm×2.5 cm×1.5 cm arising from epiglottis at the left aryepiglottic fold extending into the subglottis upto the level of the cricoid cartilage, with minimal destructive changes in the cricoid cartilage [Table/Fig-1].
Computed Tomography showing well defined, hypoattenuating expansible mass with heterogeneous enhancement of size 3.5 cm×2.5 cm×1.5 cm arising from epiglottis at the left aryepiglottic fold extending into the subglottis upto the level of the cricoid cartilage (arrow).
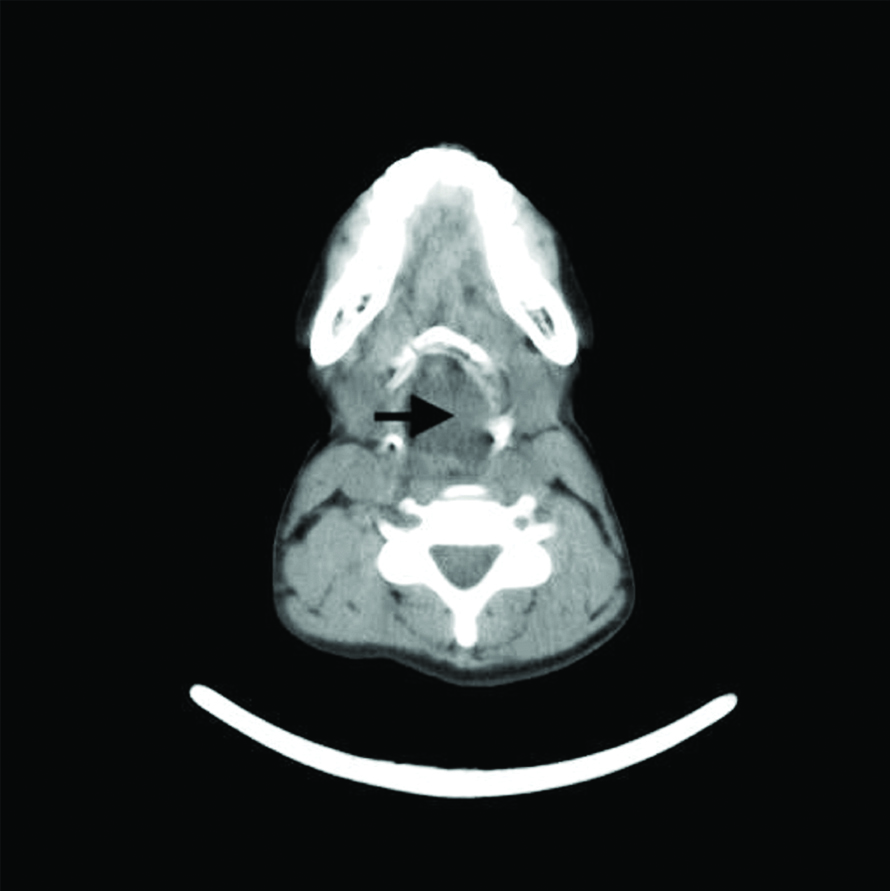
The CT scan findings were suggestive of a benign encapsulated tumour, and differentials being Schwannoma, Neurofibroma, Neuroma and Fibroma. It is very well documented in literature that Schwannoma and Neurofibromas have similar features on radiological scans. Considering the critical symptomatology, clinical findings and CT report, surgery was advised and a complete laryngectomy was performed thereafter. Postoperatively, the patient was extubated and tracheostomy was maintained. The resected Larynx along with the mass was sent for histopathological examination for further management and prognostic evaluation.
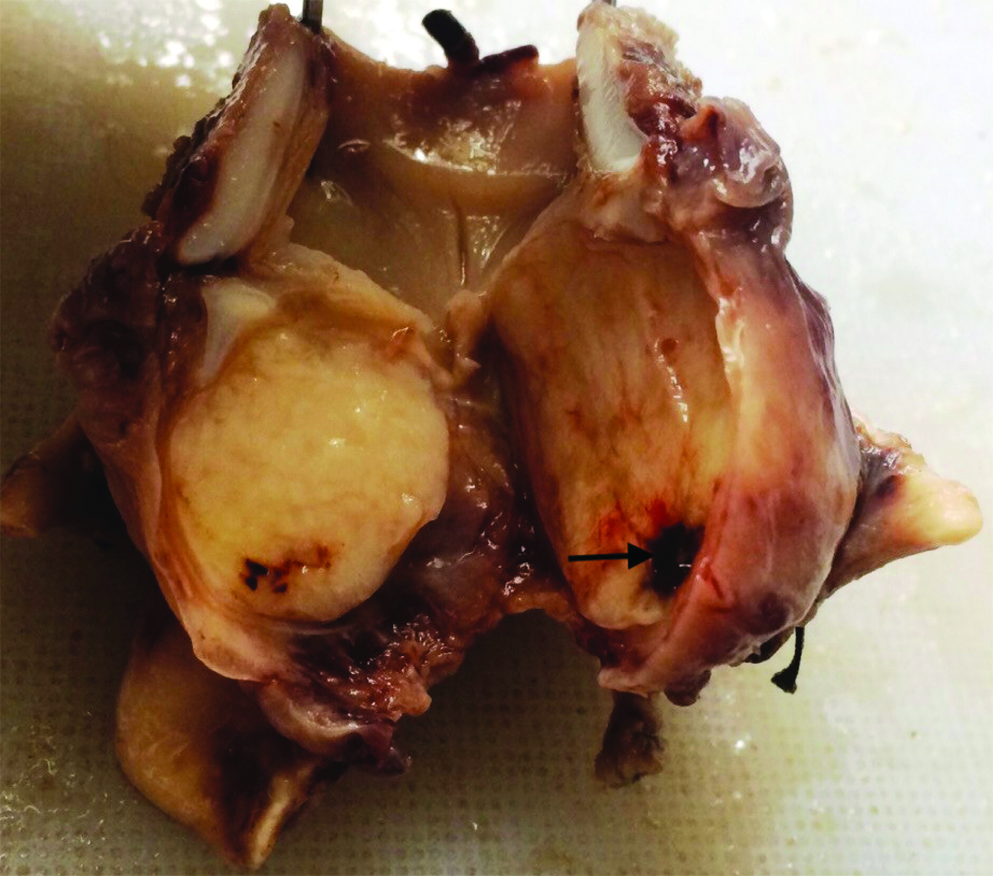
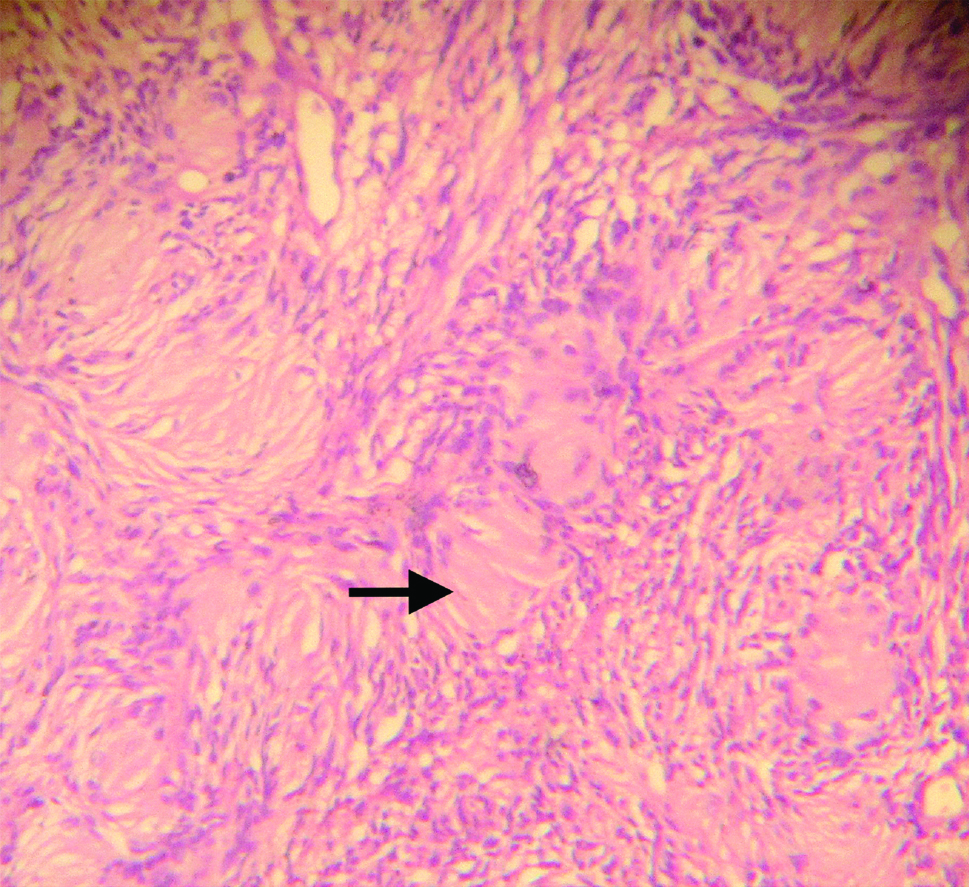
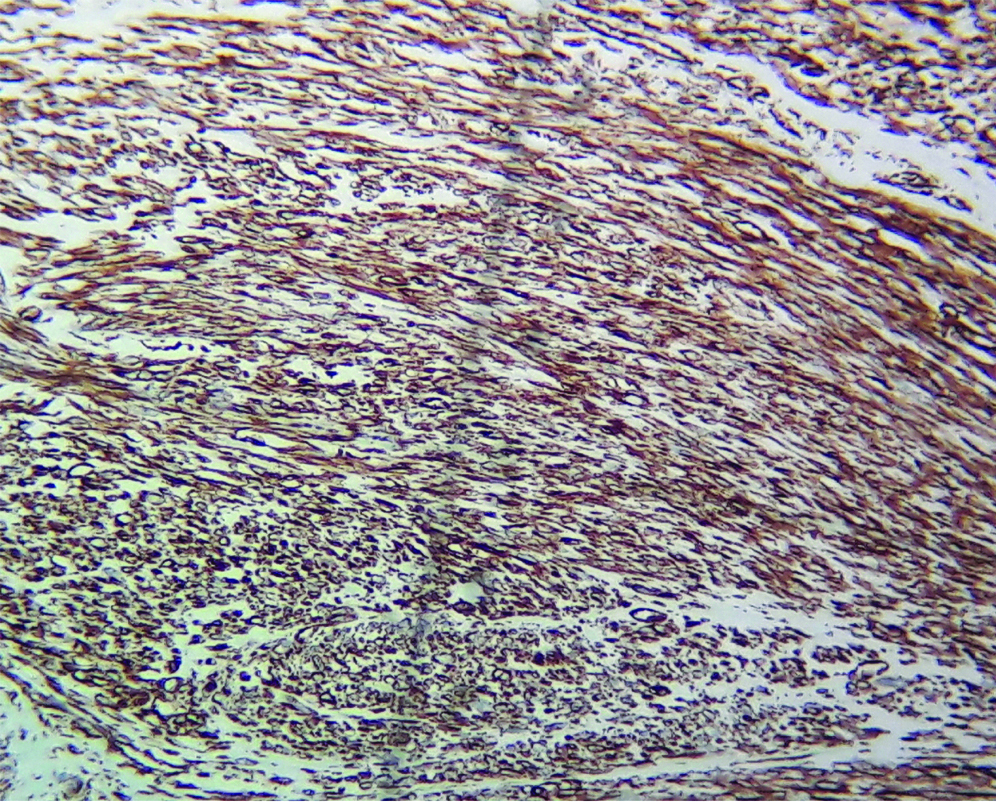
On surgical pathological examination, grossly, the mass was arising in the left aryepiglottic fold and completely occupying the glottis and damaging the left vocal cord extending into the subglottis pushing the cricoid cartilage (arrow showing cystic area). The tumour mass was well-capsulated, oval in appearance and firm to solid in consistency. The lesion on cut section showed predominantly homogeneous white area with occasional cystic areas. There were no areas of haemorrhage and necrosis [Table/Fig-2]. On microscopy, the periphery of the tumour mass showed a well-defined fibrous capsule, the predominant cells were spindle-shaped Schwann cells of neurogenic origin. The cells formed two distinct areas hypercellular antoni A areas and hypocellular antoni B areas. The spindle cells were also arranged in characteristic palisade arrangement forming pathognomic “Verocay bodies” seen in schwannomas. Histopathological features were suggestive of Schwannoma [Table/Fig-3]. Further histopathological diagnosis was confirmed by subjecting the tumour mass for immunohistochemistry. S100 stained slide of tumour mass shows strong cytoplasmic positivity in the spindle cells, which was suggestive of Schwann cell origin [Table/Fig-4]. Postoperatively, the patient has been asymptomatic.
Section from laryngectomy specimen shows a well encapsulated mass arising from the left aryepiglottic fold. Cut section shows homogeneous yellowish white areas at one or two places showing areas of haemorrhage and cystic degeneration. (arrow showing cystic area).
Microscopic examination showing spindle shaped cells with elongated nuclei, cells are of neural origin arranged in hypocellular and hypercellular areas, forming “Verocay bodies” (arrow). (H and E stain, 10x)
S100 showing strong cytoplasmic positivity in the spindle cells, suggestive of tumour of Schwann cell origin. (IHC stain, 40x)
Discussion
The laryngeal tumours are most commonly of epithelial origin, there is paucity in global incidence of laryngeal neurogenic tumours. The schwannomas are not more than 1.5% of all the benign tumours of the larynx [1,2]. Over 130 cases have been reported in the worldwide literature since it was first described in 1925 [3]. Also, known as Neurilemmomas, schwannomas are mesenchyme tumours of neural origin, arising from the nerve sheaths. The nerve tumours arise from the schwann cells responsible for myelination of the nerves [4].
Clinically schwannomas are commonly found in the flexor surfaces, and are of solitary occurrence. Common sites include spinal roots of neck, mediastinum, Cerebropontine angle is a common intracranial site of occurrence. Schwannomas also occur as part of Von Recklinghausen’s disease. Cranial nerves affected by schwannomas in the head and neck areas are the sympathetic chain, glossopharyngeal, vagal, accessory and hypoglossal nerve [5].
Schwannoma occurs more commonly in females (slight preponderance) than males, schwannoma are known to occur at any age, majority falling in the 6th to 7th decades. Considering, the cell of origin of schwannoma being the schwann cell which is responsible for formation of the peripheral sheath [6]. Schwannomas tend to spare the nerve hence, intraoperative procedures should focus on nerve sparing procedures and every attempt should be there to spare the nerve specially nerves like the facial or the vagus. The neurogenic tumours in the larynx arise from the main nerves supplying the larynx and its sub branches, nerves commonly involved include recurrent laryngeal nerve, and rarely from the superior laryngeal nerve, vagus and their minor sub branches. The schwannoma in the larynx is presumed to arise from the internal branch of the superior laryngeal nerve [7].
Origin of schwannoma involves the aryepiglottic folds rarely the vocal cords itself. Clinically, the patient symptomatology is altered voice with hoarseness and rough quality or double sounding voice (dysphonia, diplophonia), stridor is present with dyspnea, depending on the tumour size and site, there maybe presence of lump in neck, with a peculiar globus sensation accompanied with dysphagia [1].
The radio imaging of the larynx gives a good detailed outline of the neurogenic neoplasms (neurofibroma and schwannoma), especially the nature and extent of lesion, soft, solid, cystic, cartilaginous and/or bony involvement. The lesion appears well demarcated, discrete, oval in shape, with heterogenous enhancement and isoattenuation [8]. However, the radio imaging cannot differentiate between the origins of the neurogenic tumour along with explicit confirmation on the neoplastic status (benign or malignant).
The correct diagnosis of neurological tumours is extremely important as it helps to predict the clinical behaviour of the neoplasms, hence even in the larynx the differentiation between neurofibromas with that of schwannomas is vital. The behaviour of neurofibromas is different as it involves the nerve which is particularly spared in schwannomas (arising from the sheath), also the neurofibromas tend to have increased incidence of recurrence as well as malignant transformation [9].
The definitive diagnosis is performed histologically which is the gold standard. Enzinger and Weiss established three histological criteria for the diagnosis of schwannoma: encapsulation, presence of Antoni A and/or Antoni B stroma, and S-100 protein positivity. On histopathology, the schwannoma has a biphasic appearance, hypercellular areas known as Antoni A and Hypocellular areas with myxoid change Antoni B areas; the schwann cells at places have nuclei arranged in palisades to form Verocay bodies. By electron microscopy, the tumour cells have a continuous and often reduplicated basal lamina; numerous, extremely thin cytoplasmic processes; aggregates of intracytoplasmic micro fibrils; peculiar intracytoplasmic lamellar bodies; and extracellular long-spacing collagen [10].
The management for schwannomas is absolutely simplistic involving enucleation or scooping of the tumour, with minimal issue of recurrence or sequel. Ironically, in case of laryngeal neurogenic tumours like schwannoma, even being a benign well-capsulated tumour, the location particularly works against the good outcome of surgical procedure, resectibility issues as well as causing significant sequel and or complications. The usual preferred modality for laryngeal schwannomas ranges from minimal access surgery to partial laryngectomy, however in this particular case as the previous histopathological biopsy was superficial, uncertain and not clear, histopathological report stating the diagnosis as being unremarkable fibrous tissue, probably from the capsule not representing the tumour mass and the CT scan report showing extensively large midline well-delineated mass occupying most of the glottis and subglottis and also involving the cricoid cartilage with partially damage to the cartilage, since the tumour origin was uncertain along with its neoplastic potential, a complete laryngectomy was performed [11].
Laryngeal tumours require surgical management as a mainstay treatment modality. Most importantly the dyspnea and stridor needs to be allayed by securing the airway through tracheostomy. Endoscopic removal of tumour from larynx can be carried out in smaller lesions. Total laryngectomy is not recommended unless the tumour completely fills the glottic space with severe symptoms, else larger tumours utilise the external approach for removal i.e. wide excision are preferred. Procedures done are lateral thyrotomy, lateral pharyngotomy, or laryngofissure technique [12].
Conclusion
This particular case presents itself in the glottis which is an extremely unusual presentation as laryngeal schwannomas are rare and glottis of origin is most unique. Though, the benign neurogenic tumours like schwannoma have an excellent outcome and prognosis when occurring elsewhere in the body, but when present in larynx which is an extremely rare neoplastic pathology for that area, even such indolent and benign tumours impose diagnostic dilemmas and generate critical symptomatology with significant post operative sequel which can be debilitating for the patient.
[1]. Rosen FS, Pou AM, Quinn FB Jr, Obstructive supraglottic schwannoma: A case report and review of the literatureLaryngoscope 2002 112:997-1002.10.1097/00005537-200206000-0001112160298 [Google Scholar] [CrossRef] [PubMed]
[2]. Jones SR, Myers EN, Barnes L, Benign neoplasms of the larynxOtolaryngologic Clinics of North America 1984 17(1):151-78. [Google Scholar]
[3]. Zbären P, Markwalder R, Schwannoma of the true vocal cordOtolaryngol Head Neck Surg 1999 121:837-39.10.1053/hn.1999.v121.a9928210580252 [Google Scholar] [CrossRef] [PubMed]
[4]. Sonig A, Gandhi V, Nanda A, From the cell of schwann to schwannoma- a century’s fruitionWorld Neurosurg 2014 82(5):906-11.10.1016/j.wneu.2014.05.03824928363 [Google Scholar] [CrossRef] [PubMed]
[5]. Kachhara R, Raje P, Pauranik A, Schwannoma originating in lateral recess of the fourth ventricleAsian J Neurosurg 2012 7:151-53.10.4103/1793-5482.10372823293673 [Google Scholar] [CrossRef] [PubMed]
[6]. Fletcher CD, Peripheral nerve sheath tumors. A clinicopathologic updatePathol Annu 1990 25:53-74. [Google Scholar]
[7]. Nanson EM, Neurilemoma of the larynx: A case studyHead and Neck Surg 1978 1:69-74.10.1002/hed.2890010110 [Google Scholar] [CrossRef]
[8]. Lin J, Martel W, Cross-sectional imaging of peripheral nerve sheath tumors: characteristic signs on CT, MR imaging, and sonographyAJR Am J Roentgenol 2001 176:75-82.10.2214/ajr.176.1.176007511133542 [Google Scholar] [CrossRef] [PubMed]
[9]. Delozier HL, Intrinsic malignant schwannoma of the larynx: A case reportAnnals of Otology, Rhinology and Laryngology 1982 91:336-38.10.1177/0003489482091003247092059 [Google Scholar] [CrossRef] [PubMed]
[10]. Gay RE, Gay S, Jones RE Jr, Histological and immunohistological identification of collagens in basement membrane of schwann cells of neurofibromasAm J Dermatopathol 1983 5:317-25.10.1097/00000372-198308000-000026356960 [Google Scholar] [CrossRef] [PubMed]
[11]. Tulli M, Bondi S, Smart CE, Giordano L, Trimarchi M, Galli A, Diagnosis and treatment of laryngeal schwannoma: A systematic reviewOtolaryngol Head Neck Surg 2018 158(2):222-31.10.1177/019459981773550829039258 [Google Scholar] [CrossRef] [PubMed]
[12]. Ho WK, Lo SD, Ng RW, Schwannoma of the larynxEar Nose Throat J 2005 84:554-55.10.1177/014556130508400905 [Google Scholar] [CrossRef]