LDMC or LD muscle flaps have been conventionally and extensively used to resurface defects in areas of axilla, upper chest wall, lateral thoracic wall, breast, supraclavicular areas, upper arm, shoulder and deltoid areas before the advent of perforator flaps and the perforosome concept [1-4].
TDAP flap was initially designed by Angrigiani C et al., and illustrated and developed by Spinelli HM et al., and Kim JT et al., to reduce the donor site complications related to LDMC, with the main advantages being, muscle sparing and design of thinner flaps that are aesthetically better [5-7].
Blood supply of the flap is from the descending branch of the thoracodorsal artery. The thoracodorsal artery perforators are taken from the main vessel around 8-10 cm below the apex of the posterior axillary fold and reach the dermal plexus either through the septum between LD and serratus anterior muscle (septo-cutaneous) or enter LD muscle 2-3 cm from the lateral edge of LD muscle (muscular perforator) [8-10].
Length of the pedicle is 7-12 cm from the origin of the thoracodorsal artery, diameter of the vessel is 1 mm. Venous drainage of the flap is via the comitant veins of the thoracodorsal artery. On an average, the skin island can be raised to a dimension of length of 5-25 cm, width of 5-25 cm (maximum to close primarily is 12 cm) and thickness of 4-10 mm [11].
We intend to establish versatility of this flap, a relatively new member of the perforator flap family, and study the drawbacks, if any in this study.
Materials and Methods
The prospective study was conducted on 14 cases initially (3 males/11 females) out of which 12 cases (3 males/9 females) were included finally over two years (January 2014-December 2015) in the Department of Plastic and Reconstructive Surgery, Medical College and Hospital, Kolkata, India. Study population comprised of patients attending the Out Patient Department/Emergency Room (OPD/ER) and referred cases from Orthopaedics, General Surgery and Surgical Oncology departments. All patients that fulfilled the inclusion and exclusion criteria during the study period were finally included. An Institutional Ethical Clearance was obtained (Registration no. ECR/287/Inst/WB/2013). Written informed consent was obtained from the patients or patient’s parents (if peadiatric patient) before including them in the study.
Patients aged 5-70 years with post traumatic, post burn contracture release, post tumour excision, soft tissue defects in anterior chest wall, breast, neck, axilla and arm were included while grossly infected wounds, medically unfit patients, post irradiation and post cicatrisation of the proposed donor areas were excluded from the study.
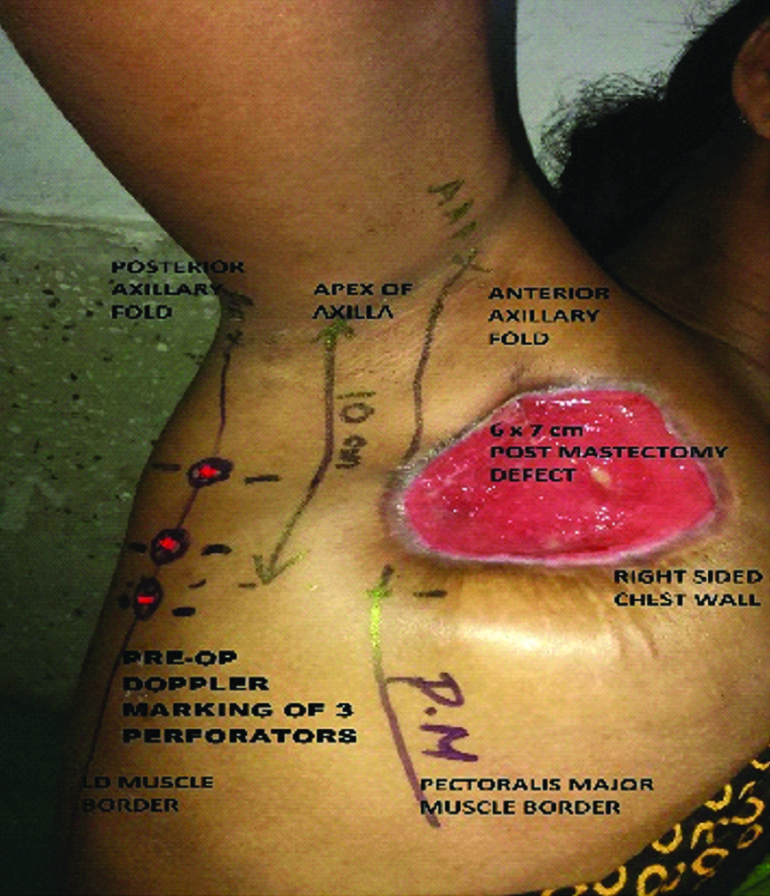
Technical details-procedure of flap harvest: Anterior axillary line, mid axillary line and posterior axillary line were marked on patient pre-operatively. The perforators were now located and marked with hand held Doppler probe. Planning in reverse was done with the template of the defect, the point of reach of the flap as well as the estimated pivot point [Table/Fig-1].
Planning of TDAP flap in a post-mastectomy defect of 6×7 cm perforators dopplered and marked with respect to anatomical landmarks.
The patient was now positioned supine or semi lateral with the upper extremity painted and draped within the operative field for manipulation. General anaesthesia with muscle relaxation was advocated in all the cases.
An exploratory incision was made along the proposed anterior border of the flap. Anterior border of the flap was kept anterior to mid axillary line so that the incision was carried straight on to serratus anterior muscle. Dissection was continued posteriorly above the muscle plane under loupe magnification. Septum between latissimus dorsi and serratus anterior muscle was identified by a fat plane and the septocutaneous perforator was looked for [Table/Fig-2].
Showing intraoperative dissection of the septocutaneous perforator from the descending branch of the thoracodorsal artery and the flap harvest in resurfacing defect after anterior axillary band contracture release in a 26-year-old post-burn female.
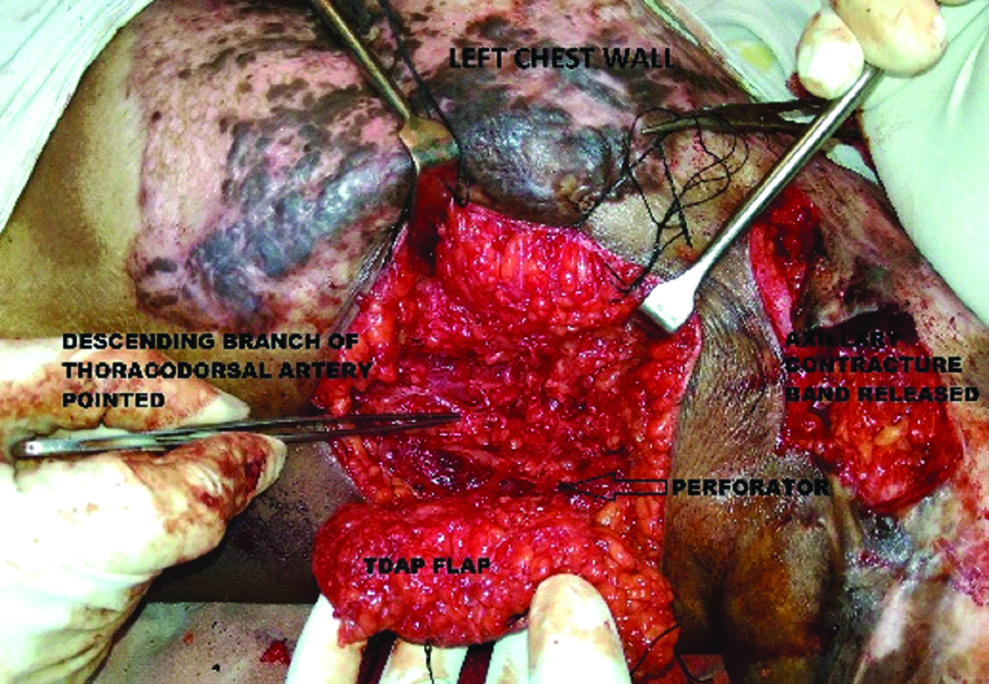
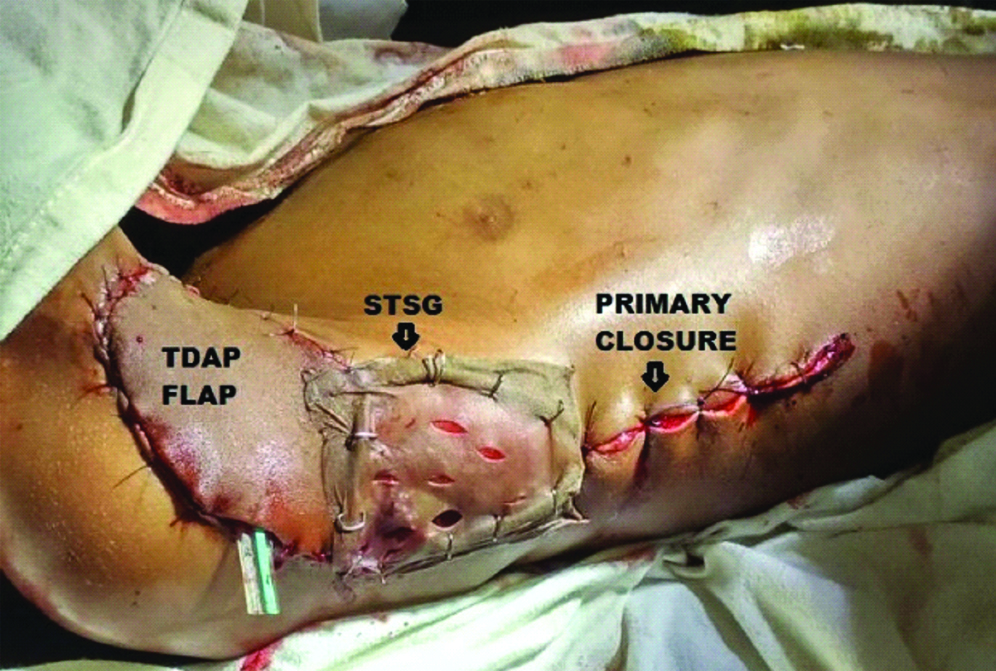
If a reliable septocutaneous perforator was not present, dissection proceeded posteriorly for musculo-cutaneous perforator through latissimus dorsi muscle. It was usually found within 2-3 cm from lateral border of LD muscle. Reliable perforator is identified by substantial size and pulsation and it is usually accompanied by a sensory nerve branch. For musculocutaneous perforator, careful deroofing is done till the origin of the thoracodorsal vessel, ligating all other branches as per requirement of the reach and pivot point. The committing incision was then made, islanding the flap and transposing it to the recipient defect area by subcutaneous tunnelling or opening up the intervening skin. A suction or corrugated rubber drain was placed under the flap and the final inset was given. The donor site was primarily closed and/or skin grafted [Table/Fig-3,4].
Showing inset of the flap and the donor site being closed primarily partially and split skin grafted partially in the defect after excision of lymphangiomacircumscripta right axilla in a 7-year-old boy.
Showing TDAP flap to resurface defect due to non-healing ulcer in superior quadrant of left breast in an 18-year-old woman and primary closure of the donor site.

Post-operative care and follow-up: Post-operatively each flap was monitored every four hours for the first 48 hours and henceforth eight hourly till the discharge of the patient. Donor site wound dressing was changed with wound inspection after 24 hours except for the skin grafted cases for which the dressing check was done after four days. The patients were discharged on an average of 5-7 days following the surgery and were followed up at two weekly intervals in OPD for the next three months.
Results
Among 12 patients (3 males/9 females), excluding two patients from the initial sample size of 14 cases, 10 flaps (84%) survived completely with complete necrosis of one flap (8%) and partial necrosis of one flap (8%). Mean age of the patients was 28.83 years. The different etiopathologies and the recipient areas are tabulated in [Table/Fig-5,6] respectively. The spectrum of soft tissue defects, the details of the patients, the dimensions of flap selected and the types of perforators encountered intraoperatively along with the complications related to flap and donor site are tabulated in [Table/Fig-7].
Different aetiopathologies that required excision.
| Etiopathologies | n=12 | % |
|---|
| Tumour resection defects | 4 | 33 |
| Trauma | 1 | 8 |
| Burn contracture release defects | 3 | 25 |
| Skin lesion excisional defects | 2 | 17 |
| Post-cellulitis scar or defects | 2 | 17 |
Recipient areas where the defects were to be resurfaced.
| Recipient Area | n=12 | % |
|---|
| Breast | 5 | 42 |
| Axilla | 5 | 42 |
| Upper Arm | 1 | 8 |
| Infraclavicular Area | 1 | 8 |
Showing the spectrum of defects and the details of the patients, according to the flaps selected, the types of perforators and the complications.
| S. No. | Age (in years) | Gender | Co-morbidity | Etiopathology | Size (in cm) and shape of flap | Perforator type | Donor site management | Complications of Flap | Donor site complications |
|---|
| 1 | 24 | Female | nil | Post-BCS defect - Early CA lt. Breast | 4×3 oval | Septo-cutaneous | primary closure | nil | Nil. |
| 2 | 19 | Female | nil | Post-cellulitis lt. Infraclavicular scar | 6×8 oval | Septo-cutaneous | primary closure | nil | widened scar at follow up. |
| 3 | 21 | Male | nil | Post-traumatic tissue loss over postero-medial lt. upper arm | 8×3 elliptical | Septo-cutaneous | primary closure | nil | nil. |
| 4 | 7 | Male | nil | Post-excision of Lymphangiomacircumscripta lt. Axilla | 5×6 oval | Musculo-cutaneous | primary closure and STSG | nil | widened scar at follow up. |
| 5 | 37 | Female | HTN | Post-Toilet mastectomy wound in advanced CA rt. Breast | 6×7 oval | Musculo-cutaneous | primary closure | nil | nil. |
| 6 | 32 | Female | nil | Post-Toilet mastectomy wound in advanced CA rt. Breast | 5×6 oval | Musculo-cutaneous | STSG | nil | wound seroma. |
| 7 | 30 | Female | nil | PBC lt. Axilla excisional release defect | 4×3 oval | Septo-cutaneous | primary closure | TOTAL FLAP NECROSIS followed by debridement & STSG | nil. |
| 8 | 52 | Female | D.M., HTN | Post-excision of Hidradenitis suppurativa of rt. Axilla | 4×3 oval | Septo-cutaneous | primary closure | nil | widened scar at follow up. |
| 9 | 55 | Female | D.M. | Post-MRM defect rt. Breast LABC | 6×4 oval | Septo-cutaneous | primary closure | nil | nil. |
| 10 | 26 | Female | nil | Post burn contracture lt. Axilla | 6×3 oval | Septo-cutaneous | primary closure | MARGINAL NECROSIS 30% requiring re-inset | widened scar at follow up. |
| 11 | 25 | Male | nil | Post burn contracture lt. Axilla | 7×5 oval | Musculo-cutaneous | STSG | Flap inset area dehiscence requiring re-inset | widened scar at follow up. |
| 12 | 18 | Female | Nil | Post-cellulitis lt. Breast ulcer | 6×5 oval | Musculo-cutaneous | primary closure | nil | nil. |
BCS: Breast conservation surgery; CA: Carcinoma; STSG: Split thickness skin graft; HTN: Systemic hypertension; PBC: Post burn contracture; D.M.: Diabetes mellitus; MRM: Modified radical mastectomy; LABC: Locally advanced breast carcinoma; lt.: left; rt.: right
Musculocutaneous perforators were encountered in five cases (42%) as opposed to septocutaneous ones in seven cases (58%). Primary closure of the donor site was done in nine cases (75%), Split Thickness Skin Graft (STSG) was done alone in two cases (17%) and combination of STSG and closure in one case (8%). Average size of the flap was 5.58×4.67 cm, mean thickness was 10 mm, and shape of flap was oval in most cases. Average operative time was 3.0 hours.
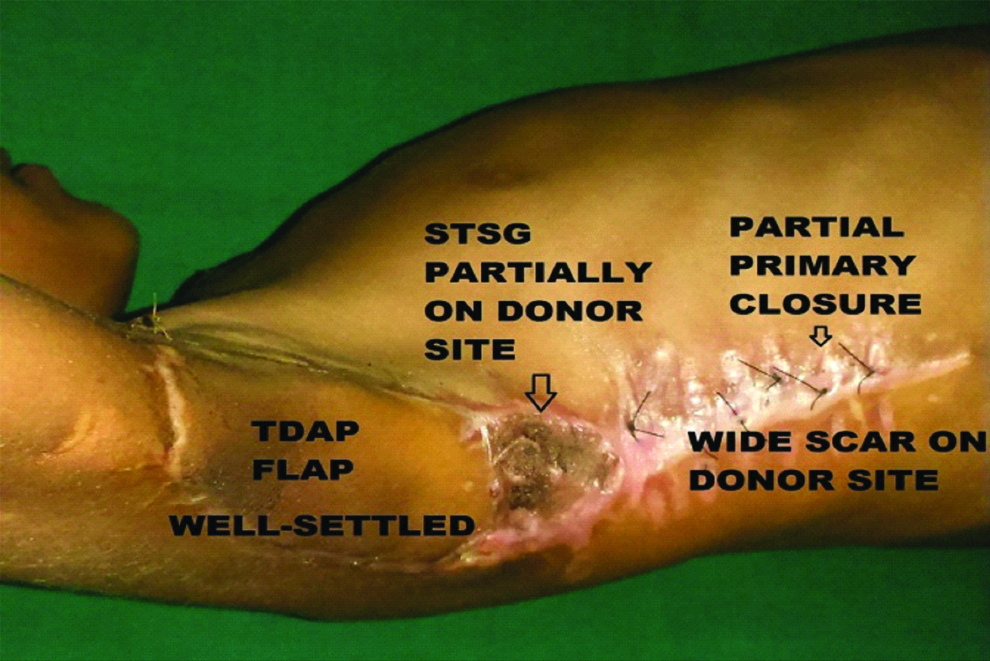
Donor site complications were encountered in the form of scar widening in five cases (41.67%) [Table/Fig-7,8], seroma in one case (8.3%).
Showing a well-settled TDAP flap with wide scar on the part of donor area where primary closure was done in a 7-year-old boy post-excision of lymphangioma circumscripta.
Discussion
The study is intended to highlight the versatility of the flap in different soft tissue defects, find out the reliable technique of flap harvest and analyse the results in term of flap quality and donor area morbidity.
The peninsular flap was used to resurface diverse areas as upper chest wall, breast, axilla and upper arm indicating the far reach of the flap. Reach of the flap is increased considerably if the perforator dissection is continued till the origin of the thoracodorsal vessel. We could get pedicle length upto 23 cm.
The flap provides a cosmetic, thin, pliable and durable cutaneous cover and the skin paddles could be oriented in either vertical, transverse or oblique axis [7,12].
The flap can be islanded, used as a peninsular rotation transposition or V-Y advancement varieties [12-14]. Size of flap on an average from our study was 5.58×4.67 cm, predominantly oval shaped with mean thickness around 1 cm. Flap as large as 16×9 cm has also been harvested in another study [7]. Primary closure was solely done for donor site management in 75% cases and the rest of 25% cases required split thickness skin grafts. In most of the other studies, as per literature, however primary closure was done in 100% cases of wound management [6]. Flap survival on post-operative monitoring and follow-up was observed in 84% cases, 8% cases underwent complete necrosis and 8% underwent partial marginal necrosis in our study. Flap failure as documented from literature for partial or marginal necrosis was 7 to 15% [7]. Scar widening in the donor site was noticed in quite a few number (41.67%) of patients. Scar widening is well known entity in the back, however upper back scar is well hidden.
In case of failure of identification of a reliable perforator, there is always a life boat of using the LD muscle primarily.
In two cases, out of the initial sample size of 14 patients, the procedure was abandoned as the exploratory incision was placed too much posteriorly near the anterior margin of LD muscle, causing the perforator along the descending vascular axis to be located much more anteriorly with their inadvertent exclusion from the flap territory. These two procedures were subsequently converted to the conventional LD muscle flap with STSG cover to resurface the defects.
Donor sites can be primarily closed with the scar in concealed line of undergarments in most of the cases with careful preoperative planning. As the LD muscle is spared donor site morbidity is substantially reduced [5,13].
Limitation
The limitation we found was the inconsistency of perforator position but nevertheless, the perforator can be found. Ours was also too small for a series of patients to reproduce statistically significant results. Continuation of this study in future will include use of this flap in distant sites as free flaps and chimeric flaps with LD muscle, serratus anterior muscle and/or scapular bone, thereby enabling reconstruction of complex defects using a single flap.
Conclusion
Pedicled TDAP flap is safe and versatile flap based on an anatomically consistent reliable perforator of the descending branch of the thoracodorsal artery, mainly septocutaneous in nature, with ease of harvest and primary closure of the donor site in well planned flaps. The spectrum of use according to aetiopathologies and the recipient sites is also wide. Also, in cases of difficulty in perforator location, inadvertent injury or doubts in flap viability, the procedure can be easily converted to a conventional LD muscle flap.
BCS: Breast conservation surgery; CA: Carcinoma; STSG: Split thickness skin graft; HTN: Systemic hypertension; PBC: Post burn contracture; D.M.: Diabetes mellitus; MRM: Modified radical mastectomy; LABC: Locally advanced breast carcinoma; lt.: left; rt.: right