Pain during and after caesarean delivery is one of the greatest concerns by patients [1]. Indeed, inadequate pain control after a caesarean delivery can significantly detract from the sense of well-being and joy for the postpartum mother by limiting maternal activities such as breastfeeding [2,3].
Opioids are commonly used for postoperative pain control in various forms such as intrathecal, parenteral, intramuscular or PCA. However, their side-effects are dizziness, nausea; vomiting and also some severe side-effect (i.e., respiratory depression) were also reported [4]. Recently, with the introduction of the Early Recovery After Surgery (ERAS) concept, early postoperative feeding has been recommended, so oral analgesic drugs were studied to decrease opioid use which minimised their undesirable side-effects. Non-Steroidal Anti-Inflammatory Drug (NSAIDs) and paracetamol are commonly used for this purpose [2].
The combination of both drugs is based on its different mechanism of action and the synergistic effect for pain relief [5-7]. Balanced multimodal analgesia uses two or more agents that act by different mechanisms to achieve a superior analgesic effect without having side-effects rather than increasing the dose of a single agent [6]. However, few randomised clinical trials have studied the effectiveness of diclofenac plus paracetamol for postoperative pain control in caesarean delivery [6] and no previous study about oral form of this combination in cesarean delivery was reported. Therefore, the purpose of this study was to determine the effectiveness of the combination of diclofenac plus paracetamol orally for pain relief after caesarean delivery.
Materials and Methods
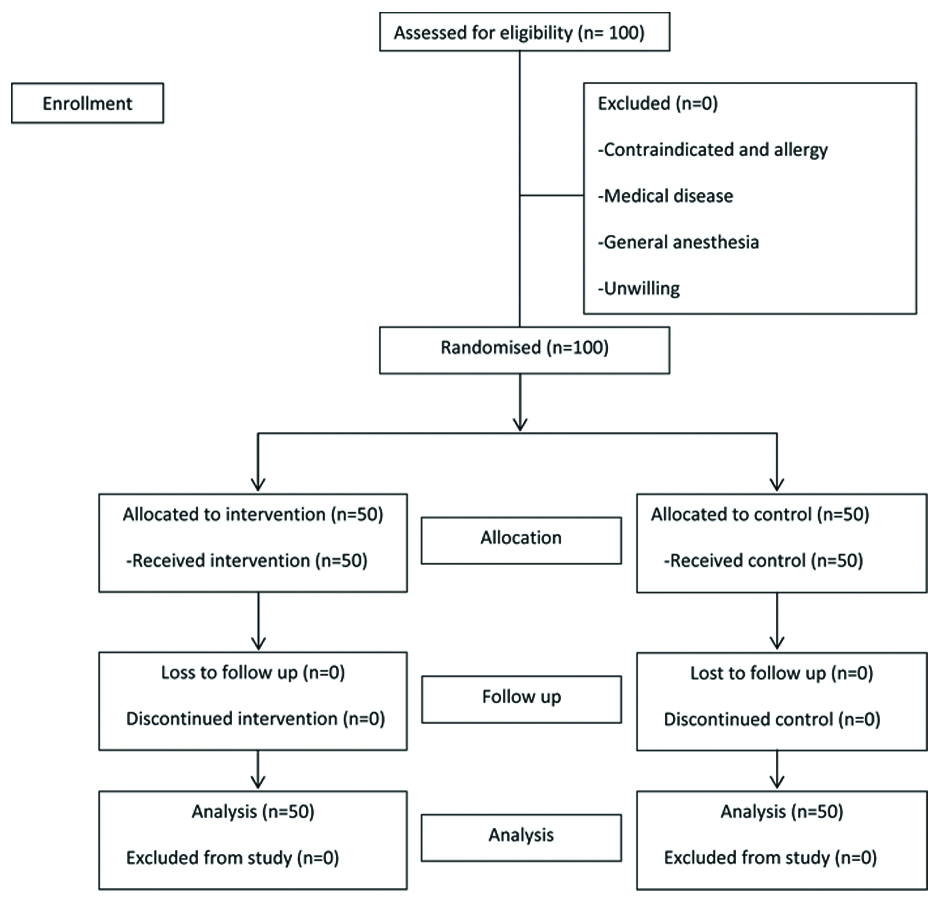
This study is a double-blind, randomised, placebo-controlled trial which was conducted in Udonthani Hospital, Udonthani, Thailand. It was approved by the Udonthani Hospital Research Ethics Committee (Number 58/2560) and was registered in the Thailand Clinical Trial Registry (TCTR20180314003). The study’s participants were 100 pregnant women who underwent low transverse caesarean delivery under spinal anaesthesia from January 2018 to June 2018. They were counselled and invited to participate in this study.
The inclusion criteria were singleton term parturient women, age 18 years or older who had an indication for low transverse caesarean delivery. The exclusion criteria were patients in whom the use of NSAIDs and paracetamol was contraindicated, had a history of NSAIDs and paracetamol allergy, had a medical disease such as hypertension, diabetes, received general anaesthesia for this operation or were unwilling to participate in this study.
Written informed consent was obtained after the explanation of study methods and side-effects to the participants. Then, all participants were randomly allocated to one of two study groups. The block randomisation, by block of four using a computer-generated number and sealed opaque envelopes, was performed.
Spinal anaesthesia was performed by an anaesthesiologist in the operating room using 0.5% bupivacaine plus 0.1-0.2 mg of morphine. All patients received standard care for low transverse caesarean delivery during the operation, in the recovery room and then were transferred to postpartum ward after two hours postoperative. After the operation, both groups received the same regimen of PCA for postoperative pain control. The intravenous morphine by PCA protocol was a concentration of 1 mg/mL, PCA only mode without loading, five minutes delayed time and 30 mg for four hours limit.
At 12-hours after the caesarean delivery, the intervention group (N=50) received diclofenac 50 mg plus paracetamol 500 mg orally [7] and then every eight hours for 24-hours. The placebo group (N=50) received the placebo on the same schedule as the intervention group. The drug and the placebo were prepared in similar packages and numbered by the researchers. The drug in the package was given to the participants by nurses. The pain scores were recorded using numerical rating scale by the trained ward nurses at 12, 20 and 24-hours postoperative [8]. The 0 to 10 numerical pain score was used which “0” represented “no pain” and “10” represented “maximum pain” [8]. All patients received omeprazole (20 mg) orally every 12-hour to prevent gastrointestinal side-effect and a soft diet according to the ERAS concept [9-11]. Drug side-effect and complications such as respiratory depression, itching, nausea and vomiting, abdominal discomfort were recorded. The postoperative complications and neonatal complication were also assessed [Table/Fig-1].
Statistical Analysis
The sample size was calculated using the formula for randomised control trial for continuous data [12]. The mean pain score in the study group was 3.0 and SD was 1.7, the mean pain score in a control group was 4.0 and the SD was 1.7. An alpha error was 0.05 and power was 80%. Numbers of participant by calculation were 46 participants per groups. An additional four subjects per groups were recruited to the study for possible drop out from study, the total sample size was 50 per group. The groups were compared using an unpaired t-test for continuous variables, Chi-square and Fisher-exact tests for categorical variables. The mean difference with a 95% CI was calculated for the magnitude of effect. Statistical analysis was performed using Stata version 13.0 (Stata Corp, College Station, TX). The p-value <0.05 was considered statistically significant.
Results
A total of 100 participants were included in this study with 50 in each group. All were continued until the study’s completion and were included in the data analysis. The participants’ characteristics in both groups are shown in [Table/Fig-2]. Both groups were comparable in terms of maternal age, parity, body weight, type of incision, operation time, estimated blood loss, adhesion and tubal resection except previous surgery and indication for caesarean delivery.
Baseline characteristic of diclofenac plus paracetamol (intervention) and placebo group. (data was presented in mean (SD) unless specified otherwise).
| Characteristics | Intervention group (N=50) | Placebo group (N=50) | p-value |
|---|
| Age, years (SD), range | 29.0 (5.3),22-41 | 29.2 (5.6),20-42 | 0.80a |
| Maternal weight (kg, SD) | 72.4 (12.1) | 72.5 (13.9) | 0.99a |
| Primipara (N,%) | 8 (16.0%) | 15 (30.0%) | 0.10b |
| Operation time (min) | 49.2 (15.7) | 49.5 (26.8) | 0.94a |
| Tubal resection (N,%) | 31 (62.0%) | 26 (52.0%) | 0.31b |
| Adhesion (N,%) | 10 (20.0%) | 5 (10.0%) | 0.16b |
| Previous surgery (N,%) | 33 (64.0%) | 19 (38.0%) | 0.01b* |
| Indication (N,%) |
| Previous C/S | 32 (64.0%) | 15 (30.0%) | <0.01b* |
| CPD | 16 (32.0%) | 27 (54.0%) |
| Fetal distress | 2 (4.0%) | 8 (16.0%) |
| Type of incision |
| Pfannenstiel | 15 (30.0%) | 9 (18.0%) | 0.16b |
| Low midline | 35 (70.0%) | 41 (82.0%) |
| Blood loss (mL) | 303.0 | 302.0 | 0.96a |
SD=standard deviation; C/S=Caesarean delivery
p-value were calculated by (a) unpaired t-test and (b) Chi-square tests
*statistical significance (p<0.05)
The primary outcome was the comparison of effectiveness of pain control after operation between two groups by using a numerical rating scale. The mean pain scores at the beginning of diclofenac plus paracetamol and placebo (12-hours postoperative) were similar in both groups. The mean pain scores at 20 and 24-hours postoperative were lower in the diclofenac plus paracetamol group which were 2.10+1.39 and 1.66+1.33 in the diclofenac plus paracetamol group compared with 2.86+1.60 and 2.92+1.55 in the placebo group. The mean difference at 20-hours was 0.76 (95% CI 0.17 to 1.36, p-value=0.01) and the mean difference at 24 hours was 1.26 (95% CI 0.69 to 1.83, p-value<0.01) with statistical significant difference. The amount of opioids used was also higher in the placebo group [Table/Fig-3]. The adverse effect of opioid, such as nausea and vomiting, was decreased in the diclofenac plus paracetamol group. The adverse effect of NSAIDS, such as abdominal discomfort, was not increased. Postoperative complications such as fever or postpartum haemorrhage were not detected in either group. Neonatal complication such as gastrointestinal side-effect was also not detected [Table/Fig-4].
Pain score in intervention and control group (mean+SD) at baseline (12 hours), 20 and 24 hours and total dosage of opioid used (mg).
| Outcome | Intervention Group | Control Group | Mean difference (95%CI) | p-value* |
|---|
| Mean pain score |
| Baseline (12 hours) | 2.66±1.36 | 2.76±1.89 | 0.10 (-0.55 to 0.75) | 0.76 |
| 20-hours | 2.10±1.39 | 2.86±1.60 | 0.76 (0.17 to 1.36) | 0.01** |
| 24-hours | 1.66±1.33 | 2.92±1.55 | 1.26 (0.69 to 1.83) | <0.01** |
| Opioid used (mg) | 1.46±2.81 | 3.34±4.53 | 1.88 (0.38 to 3.38) | 0.01* |
SD=Standard deviation; CI=Confidence interval
*p-values were calculated by unpaired t-test; **statistical significance (p<0.05)
Side-effect of diclofenac plus paracetamol (intervention) and placebo group.
| Side-effect | Intervention group | Control group | p-value* |
|---|
| Nausea/Vomiting | 1 (2.0%) | 7 (14.0%) | 0.03** |
| Abdominal discomfort | 4 (8.0%) | 9 (18.0%) | 0.12 |
| Itching | 5 (10.0%) | 4 (8.0%) | 0.50 |
*p-value was calculated by Fisher’s-exact test; **statistical significance (p<0.05)
Discussion
The objective of this study was to evaluate the effectiveness of diclofenac plus paracetamol in post-cesarean delivery pain control. The result demonstrates that the combination of these two drugs can decrease the mean pain score at 20 and 24-hours postoperative significantly. The amount of opioid used and its adverse effect was also lower than the placebo group. The adverse effect of NSAIDs, such as abdominal discomfort, was not increased.
The result from current study was similar to previous studies such as Taneja AV et al., Mitra S et al., and Darvish H et al., that reported the intravenous form of combination of diclofenac and paracetamol was effective in pain control after caesarean delivery without serious adverse effect [6,13,14]. Siddik SM et al., and Munishankar B et al., reported the rectal suppository form of combination of diclofenac and paracetamol was also effective in pain control after caesarean delivery [15,16]. This study was interested in studying the effectiveness of an oral route of this combination because of patient’s advantages in the convenient form of drug administration, less pain and lower cost than the other routes. The results of the study confirmed that the combined oral use of diclofenac plus paracetamol is effective in addition with intravenous PCA for better postoperative pain control in caesarean delivery.
A worrisome side-effect of NSAIDs is gastrointestinal irritation. In this study, the short postoperative period use of the oral form of diclofenac did not increase the gastrointestinal side-effect which was similar to a previous study [15], however, this might be caused from the prophylaxis proton-pump inhibitor (omeprazole) used in this study. Another concern is the side-effect to the baby by breastfeeding. From this study, there was no neonatal complication detected which corresponded with the previous studies about diclofenac and paracetamol level in breast milk which found only small amounts of both drugs. Therefore, there is a low risk of any hazard to breastfed infants [17,18].
The strength of this study is the prospective randomised, double-blinded with placebo-controlled study design. The block randomisation with opaque envelope made a good representation of the population.
Limitation
This study has some limitations such as it studied only the combination of diclofenac plus paracetamol, so the effect of diclofenac only or paracetamol only cannot be demonstrated from this study. The use of other types of oral NSAID in post caesarean delivery still needs further study.
Conclusion
The addition of diclofenac 50 mg plus paracetamol 500 mg orally provided better pain control with less opioid used in 24-hours after a caesarean delivery when compared with intravenous opioid PCA only.
SD=standard deviation; C/S=Caesarean delivery
p-value were calculated by (a) unpaired t-test and (b) Chi-square tests
*statistical significance (p<0.05)
SD=Standard deviation; CI=Confidence interval
*p-values were calculated by unpaired t-test; **statistical significance (p<0.05)
*p-value was calculated by Fisher’s-exact test; **statistical significance (p<0.05)