Virtual Amputation as a Conservative Surgical Approach in Treating Diabetic Foot Osteomyelitis- A Case Series
Abdul Wafiy Mohd Padzil1, Mohd Yazid Bajuri2
1 Doctor, Department of Orthopaedics and Traumatology, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, W.P Kuala Lumpur, Malaysia.
2 Associate Professor, Department of Orthopaedics and Traumatology, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, W.P Kuala Lumpur, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohd Yazid Bajuri, Department of Orthopaedics and Traumatology, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, W.P Kuala Lumpur, Malaysia.
E-mail: ezeds007@yahoo.com.my
Diabetic Foot Osteomyelitis (DFO) has been described as one of the factor that can interrupt the healing process of a Diabetic Foot Ulcer (DFU). It shows that it has a significant correlation with lower limb amputation. One of the methods to treat this condition is by virtual amputation in which the infected bone is debrided with the ulcer site and the wound has a better chance to heal faster. This also shortens the duration of antibiotic course. We present a case series consisting of six patients that have been treated with virtual amputation from June 2017 till August 2017. These patients were treated by removing part of the osteomyelitic bone and dead tissues. Although there is no bone to support but the surrounding soft tissue coverage helps to maintain the configuration of the affected part in which it retained good appearance, cosmetically.
Debriding, Healing, Infected bone
Introduction
DFU is one of the major complications that can lead to heavy economic burden to patients and health care system. It is known that an accompanied infected bone acts as a limiting factor in wound healing. Here in this case series, we describe a conservative surgical approach in which we remove all the infected bone and necrotic tissue which is described as a virtual amputation. We present a retrospective case series consisting of six patients treated with virtual amputation from June 2017 till August 2017. All of these patients had undergone surgery to remove part of the osteomyelitic bone and necrotic tissue, salvaging the outer soft tissue coverage to maintain the appearance of the toe. The removal of either involved part of the distal phalanx or part of the proximal phalanx of the toe. The wound either had a primary closure or secondary wound healing depending on the severity of the involved part.
Case Series
Patients with diabetic foot infection with osteomyelitic changes were selected. All patients selected had good Ankle Brachial Systolic Index (ABSI). Osteomyelitis changes on plain radiograph with elevated infective marker had weighed in the decision of proceeding with virtual amputation. Empirically, sulbactam/ampicillin was started and post-operative antibiotic was tailored according to bone culture and sensitivity finding. Mean duration of antibiotic treatment for the patients was fourteen days.
There were six patients reported within the study period [Table/Fig-1]. During the surgery, non-viable bone and ulcer were debrided. Unhealthy bones nibbled until “Paprika sign” seen which was characterised by punctuate haversian bleeding [1,2]. Two out of 4 patients underwent primary closure. All wounds were cleansed with superoxide water and dressing was done with either gel or paraffin net based on the wound condition [3]. There was no re-debridement done for all 6 cases.
Summary of patients who underwent virtual amputation.
| No | Presentation | Radiograph | Surgery | Cultures/Antibiotic |
|---|
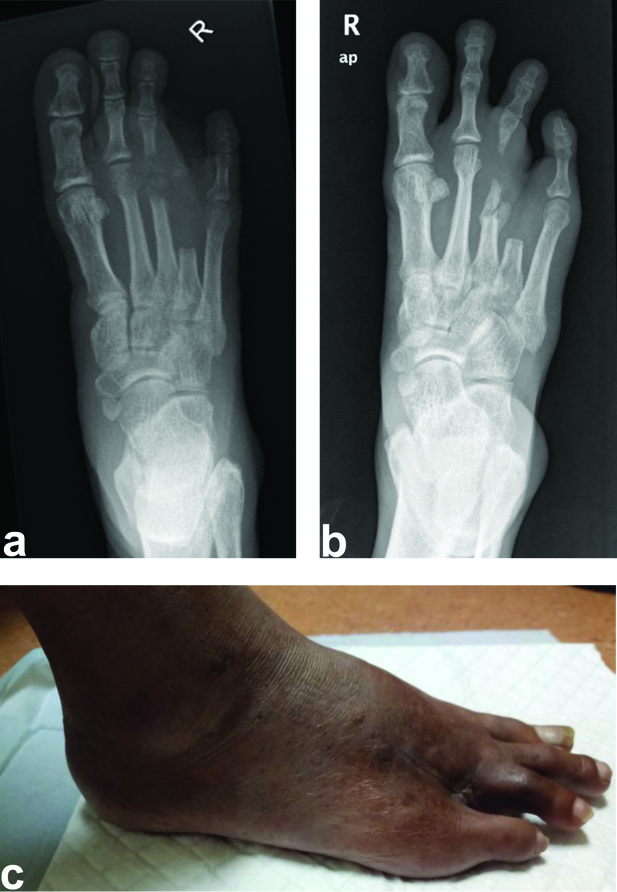
| 1. | A 66-year-old Malay lady presented with blisters over dorsum of base left 5th toe [Table/Fig-2]. | Osteomyelitis over head of 5th Metatarsal Bone (MTB) | Wound debridement and virtual amputation of left 5th MTB.Secondary suturing was done. | Mixed growthSulbactam/Ampicillin |
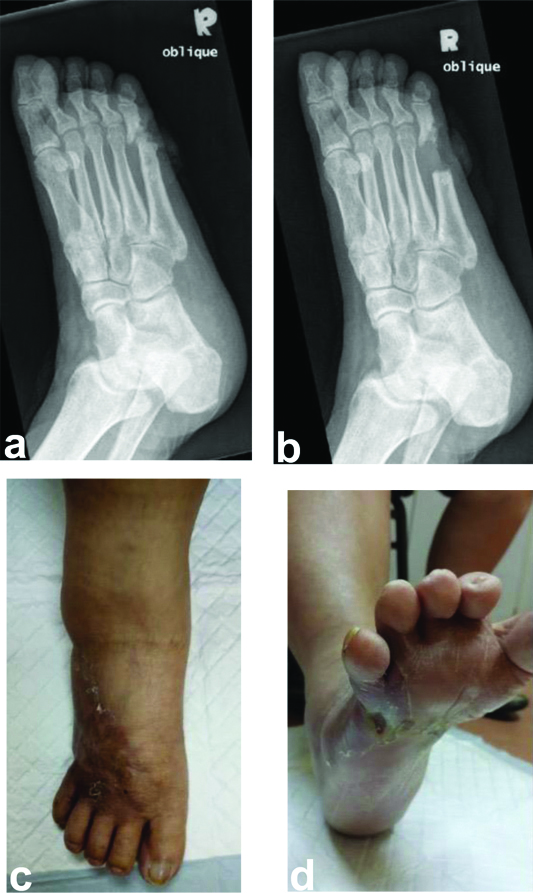
| 2. | A 43-year-old Indian gentleman with history of rays amputation of left 2nd and 3rd toes presented with non-healing plantar ulcer over head of left 4th metatarsal area [Table/Fig-3]. | Osteomyelitis over left 4th Metatarsophalyngeal Joint (MTPJ) | Wound debridement and virtual amputation of left 4th MTPJ with primary closure. | Staphylococcus aureusPseudomonas aeroginosaSulbactam/Ampicillin |
| 3. | A 52-year-old Malay gentleman with history of 4th toe ray amputation presented with abscess over right 3rd MTPJ area [Table/Fig-4]. | Osteomyelitic changes over right 3rd MTPJ | Wound debridement and virtual amputation of 3rd MTPJ.Secondary suturing was done. | Mixed growthSulbactam/Ampicillin |
| 4. | A 67-year-old Malay gentleman presented with abscess over right 2nd web space [Table/Fig-5]. | Osteomyelitic changes over right 2nd and 3rd MTPJ. | Incision and drainage over right 2nd web space virtual amputation of 2nd and 3rd MTPJ.Secondary suturing was done. | Mixed growthSulbactam/Ampicillin |
| 5. | A 54-year-old chinese gentleman presented with chronic ulcer over right 5th MTPJ area [Table/Fig-6]. | Osteomyelitic changes over right 5th MTPJ. | Wound debridement with virtual amputation of right 5th MTPJ.Secondary healing by daily dressing was done. | Pseudomonas aeroginosaResistance to Sulbactam/ampicillinChange to IV Ceftazidime |
| 6. | A 60-year-old malay gentleman presented with abscess over medial border of right big toe [Table/Fig-7]. | Osteomyelitic changes over metatarsal, proximal phalanx and distal phalanx of right big toe. | Wound debridement with virtual amputation of metatarsal, proximal phalanx and distal phalanx of right big toe.Primary closure of medial wound done. | Staphylococcus aureusSulbactam/Ampicillin |
Case 1. (a) Pre-operative radiograph revealed osteomyelitic changes over head of 5th MTPJ; (b) Post virtual amputation radiograph, where osteomyelitic bone removed; (c) Wound over 4th webspace completely healed with plantigrade feet preserved.

Case 2. (a and b) Radiograph pre and post virtual amputation of left foot; (c and d) Plantigrade foot with well healed wound post 2 weeks virtual amputation.

Case 3. (a and b) Pre and post operative radiograph shows osteomyelitic bone over 3rd MTPJ had been removed; (c) wound healed well during visit at 4 weeks postoperatively.
Case 4. (a and b) Virtual amputation done over 2nd and 3rd MTPJ done. (c, d and e) Note that, even 2nd and 3rd toes shortened and deformed, patient still able to wear shoe.
Case 5. (a) Preopertive radiograph revealed osteomyelitic changes of 5th MTPJ; (b) 5th MTPJ were removed until healthy edge. (c and d) Virtual amputation of 5th MTPJ had fasten the ulcer recovery.

Case 6. (a) Osteomyelitic changes over 1st ray; (b and c) Note that extensive virtual amputation has been done with big incision over medial border of right big toe; (d and e) Patient was offered for germinal matrix ablation but refused as he satisfied with current surgical outcome.

All 6 patients showed good wound healing post virtual amputation with mean time of six weeks. Even though the affected toes were shortened and deformed, all six patients had painless, plantigrade, stable and shoe-able foot [Table/Fig-2,3,4,5,6 and 7].
Discussion
Diabetes mellitus is a major health concern in Malaysia with 1/5th of population aged more than 30-year-old was diagnosed with Type 2 diabetes mellitus in 2007 [4]. Idea of this virtual amputation technique is mainly to conserve bio-mechanics [5] of the foot and to anticipate subsequent amputation of the ipsilateral limb [6]. However, early detection remains a challenge as bony changes will occur over time from the initial inoculation. Differentiation between DFO and neuropathic osteoathropathy is a challenge in treating this condition [5]. Three pathogenesis namely vasculopathy, neuropathy and immunopathy have always been blamed for delayed healing of DFU [5,7]. DFO rarely become a primary attention in treating this condition as plain radiograph is not a routine investigation during clinic follow-up. Serial radiographs are more cost-effective as compared to expensive imaging such as magnetic resonance imaging or scintigraphy [8]. DFO is an indication of the severity for DFU as it is a criteria in grade 3 Wagner classification [9]. Sun JH et al., proposed that a high Wagner grade together with elevated white cells count and low ankle brachial systolic index, serum albumin and haemoglobin were significantly correlated with lower limb amputation [9].
In DFO, involucrum and biofilm act as a barrier for antibiotic to penetrate [2,5,10]. By doing virtual amputation, resection of this bone not only shortens the antibiotic period but also fasten the healing process [11-13]. Lázaro-Martínez JL et al., suggested for 10 days of antibiotic treatment for patient who underwent virtual amputation as compared to the group being treated solely with 90 days antibiotic without surgical intervention [12]. This is important as the risk of antibiotic toxicity and resistance increases as well [11]. The mainstay of the treatment if the patient develops chronic osteomyelitis is to eradicate the infection, reduce the pain and try to salvage the functional limb [14]. Later, when there is a need for reconstructive surgery, it can be done when the patient’s nutrition and any underlying metabolic diseases have been optimised and there is normalisation of the infective parameters and favourable condition of the soft tissue [15].
As the wound healing is rapid in virtual amputation, we observed that the compliance of the patients towards offloading treatment can be shortened and patient can return to their premorbid function faster [13]. However, the challenge with virtual amputation is that the healed toes could be deformed and short. A proper bandaging and wound management can “guide” the healing toe to align with other toes. By doing this, the patient’s psychological effect can be boosted in a positive way, as patient is able to keep the normal appearance of the foot [13].
Izumi Y et al., had proposed that the risk of subsequent amputation over ipsilateral limb is higher within 6 months after the initial amputation [6]. Murdoch DP et al., had similar finding with 40% of his patients with lower extremity amputation had history of amputation before [16]. Attempt to avoid amputation and preservation of soft tissue is essential to prevent alteration in foot’s biomechanics [13]. In cases where ray amputation was done, ulcers developed as the consequence of imbalance plantar pressure point [13]. Besides that, ray amputation is always done extensively and neighbouring digital artery is at risk for injury. This leads to risk of gangrene, further bacteria inoculation and amputation of neighbouring toes [5].
Conclusion
As conclusion, a systematic approach towards DFO with virtual amputation as an option of treatment is likely to reduce healthcare cost and reserve functional foot.
[1]. Hannan CM, Attinger CE, Special considerations in the management of osteomyelitis defects (diabetes, the ischemic or dysvascular bed, and irradiation)In Seminars in plastic surgery 2009 23(2):132Thieme Medical Publishers10.1055/s-0029-121416520567735 [Google Scholar] [CrossRef] [PubMed]
[2]. Fang RC, Galiano RD, Adjunctive therapies in the treatment of osteomyelitisIn Seminars in plastic surgery 2009 23(2):141Thieme Medical Publishers10.1055/s-0029-121416620567736 [Google Scholar] [CrossRef] [PubMed]
[3]. Aragón-Sánchez J, Lázaro-Martínez JL, Quintana-Marrero Y, Sanz-Corbalán I, Hernández-Herrero MJ, Cabrera-Galván JJ, Super-oxidized solution (Dermacyn Wound Care) as adjuvant treatment in the postoperative management of complicated diabetic foot osteomyelitis: preliminary experience in a specialized departmentThe International Journal of Lower Extremity Wounds 2013 12(2):130-37.10.1177/153473461347671023446366 [Google Scholar] [CrossRef] [PubMed]
[4]. Raja NS, Microbiology of diabetic foot infections in a teaching hospital in Malaysia: a retrospective study of 194 casesJournal of Microbiology Immunology and Infection 2007 40(1):39 [Google Scholar]
[5]. Berendt AR, Peters EJ, Bakker K, Embil JM, Eneroth M, Hinchliffe RJ, Diabetic foot osteomyelitis: a progress report on diagnosis and a systematic review of treatmentDiabetes/Metabolism Research and Reviews 2008 24(S1)10.1002/dmrr.83618442163 [Google Scholar] [CrossRef] [PubMed]
[6]. Izumi Y, Satterfield K, Lee S, Harkless LB, Risk of re-amputation in diabetic patients stratified by limb and level of amputation: a 10-year observationDiabetes Care 2006 29(3):566-70.10.2337/diacare.29.03.06.dc05-199216505507 [Google Scholar] [CrossRef] [PubMed]
[7]. Damir A, Why Diabetic Foot Ulcers do not heal?J International Medical Sciences Academy 2011 24(4):205-06. [Google Scholar]
[8]. Pineda C, Espinosa R, Pena A, Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphyIn Seminars in Plastic Surgery 2009 23(2):80Thieme Medical Publishers10.1055/s-0029-121416020567730 [Google Scholar] [CrossRef] [PubMed]
[9]. Sun JH, Tsai JS, Huang CH, Lin CH, Yang HM, Chan YS, Risk factors for lower extremity amputation in diabetic foot disease categorized by Wagner classificationDiabetes Research and Clinical Practice 2012 95(3):358-63.10.1016/j.diabres.2011.10.03422115502 [Google Scholar] [CrossRef] [PubMed]
[10]. Brady RA, Leid JG, Calhoun JH, Costerton JW, Shirtliff ME, Osteomyelitis and the role of biofilms in chronic infectionFEMS Immunology & Medical Microbiology 2008 52(1):13-22.10.1111/j.1574-695X.2007.00357.x18081847 [Google Scholar] [CrossRef] [PubMed]
[11]. Van GH, Siney H, Danan JP, Sachon C, Grimaldi A, Treatment of osteomyelitis in the diabetic foot: contribution of conservative surgeryDiabetes Care 1996 19(11):1257-60.10.2337/diacare.19.11.12578908390 [Google Scholar] [CrossRef] [PubMed]
[12]. Lázaro-Martínez JL, Aragón-Sánchez J, García-Morales E, Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis. A randomized comparative trialDiabetes Care 2013 :DC_13152610.2337/dc13-152624130347 [Google Scholar] [CrossRef] [PubMed]
[13]. Bajuri MY, Virtual amputation in diabetic foot infection with osteomyelitisAnn Clin Case Rep 2017 2:1249 [Google Scholar]
[14]. Muhammad Hafiz AS, Mohd Yazid B, Norliyana M, Rasyidah R, Limb salvage surgery in chronic osteomyelitis: a case reportMed & Health 2018 13(1):286-90.10.17576/MH.2018.1301.31 [Google Scholar] [CrossRef]
[15]. Bajuri MY, Abdul Razak KA, Chronic osteomyelitis of the femur with segmental bone defect: concepts and treatmentJournal of Krishna Institute of Medical Sciences University 2017 6(2):127-30. [Google Scholar]
[16]. Murdoch DP, Armstrong DG, Dacus JB, Laughlin TJ, Morgan CB, Lavery LA, The natural history of great toe amputationsThe Journal of Foot and Ankle Surgery 1997 36(3):204-08.10.1016/S1067-2516(97)80116-0 [Google Scholar] [CrossRef]