“Thalessaemia” is Greek word meaning “sea” and “blood” named after the fallacy of its confinement to mediterranean region only [1,2]. This disorder is found in every ethnic group all over the world, with high prevalence in equatorial regions of Asia and Africa [1]. Incidence of thalassaemia ranges from 3 to 100 patients per 100,000 people in middle eastern countries, south-east asia, caspian sea (Thalassaemia Belt). About 5-70% thalassaemia carriers are seen in these regions [3]. This condition was first described by Cooley TB et al., in 1927 [4].
The average prevalence of β thalassaemia carriers is 3-4% which equals to 35 to 45 million carriers in our multi-ethnic and culturally and linguistically diverse population of 1.21 billion people; which also includes around 8% of tribal groups according to the Census of India 2011. Several ethnic groups have a much higher prevalence (4-17%) [5].
Thalassaemia is a chronic, inherited haemoglobinopathy caused due to defective erythropoiesis resulting in absence of globin chains. Based on affected globin chains thalassaemia is classified into alpha and beta thalassaemias. According to genetic and clinical findings thalassaemia is classified into major, minor and intermediate type [1,2]. ‘Cooley’s Anaemia’ is other name of thalassaemia major which is also called as ‘Mediterranean Anaemia’. Thalassaemia Intermedia and Thalassaemia Minor are referred as ‘Beta thalassaemia carrier’, ‘Beta thalassaemia trait’ or ‘Heterozygous beta thalassaemia’ [2].
This condition presents with typical radiographic features due to associated craniofacial defects which are important diagnostic criteria to identify the disease. Intraoral periapical radiographs, orthopantamographs, lateral skull radiographs in these patients show characteristic changes in diploic spaces, typical ‘hair on end appearance’, taurodontism and enlarged bone marrow spaces. Computed Tomography scan (CT) may demonstrate various skeletal manifestations of this disorder pertaining to bone marrow spaces, ribs, spine and long bones.
With advent of CBCT in 1900’s, creating 3D anatomically true images is possible with less radiation exposure as compared to CT. CBCT has been widely used since then because of its benefits such as improved magnification of images and lower price compared to conventional CT systems [6].
This article attempts to provide an overview of radiographic findings of Thalassaemia by conventional radiography, CT, MRI and by CBCT comprehensively, combining the literature findings and analysing the early detection of the potential manifestations.
Materials and Methods
A literature search was performed using PubMed and ResearchGate, with language restriction to English. The search used key words such as ‘thalassaemia’,‘radiological features of thalassaemia’, ‘CBCT images of thalassaemia patients’. The search was broadened to case reports, case control studies, randomised control trials related to thalassaemia. Out of 80 articles, only 20 of them were found relevant out of which 12 articles had direct access and were included in the present review, 40 articles had duplication of information and 20 articles with improper content were excluded. Only one study retrieved was a randomised trial. Five articles were case reports and two were pictorial reviews. The [Table/Fig-1,2] present complete analysis of literature search [1,3,4,6-9,11-13,14,15] [1,4,7,8,10-13,14,15].
Over view of the studies utilized in the review with the imaging modalities [1,3,4,6-9,11-13,14,15].
| Author | Year | Imaging modalities | Description |
|---|
| Bougilia S et al., [1] | 2006 | CBCT | Case report |
| Tunaci M et al., [8] | 1999 | Conventional skull radiographs, CT, MRI | Pictorial review |
| Tyler PA et al., [7] | 2006 | Skull radiographs, MRI | Pictorial review |
| Javid B et al., [3] | 2015 | CT | Case report |
| Hazza AM et al., [11] | 2006 | Conventional radiography | Randomised controlled trials |
| Akkurta A [6] et al., | 2017 | CBCT | Study |
| Guangbin Z et al., [4] | 2012 | CT, MRI, conventional radiographs | Retrospective review on medical records |
| Akpek S et al., [9] | 2001 | CT | Study |
| Ohri N et al., [12] | 2015 | Conventional and Skull radiographs | Study |
| Basu S et al., [13] | 2009 | Skull radiographs | Case report |
| Amit B et al., [14] | 2014 | Skull radiographs | Case report |
| Dinan D et al., [15] | 2013 | Conventional radiographs, MRI | Case report |
CT: Computed tomography; MRI: Magnetic resonance imaging; CBCT: Cone beam computed tomography; OPG: Orthopantamograph
Overview of all radiological features of thalassaemia [1,4,7,8,10-13,14,15].
| Investigations | Salient features | Reference studies |
|---|
| Conventional radiography | Prominent antegonial notch Spiky-shaped and short roots showing Taurodontism, diminished lamina dura, enlarged bone marrow spaces, small maxillary sinuses, non appearance of inferior alveolar canal, thin cortex of the mandible, cob webbing pattern of pelvis | Guangbin Z et al., [4]Tyler PA et al., [7]Tunaci M et al., [8]Abolhasani FA et al., [10]Hazza AM et al., [11]Ohri N et al., [12]Dinan D et al., [15] |
| Skull radiography | Widened diploic spaces, displacement and thinning of outer cortical table,“hair -on-end” pattern of trabeculae, laterally displaced orbits, forwardly displaced incisors | Tyler PA et al., [7]Tunaci M et al., [8]Ohri Net al., [12]Basu S et al., [13]Amit B et al., [14] |
| CT scan | Widened diploic space, Rib-within-rib appearance, trabecular destruction, cortical thinning and osteoporosis of vertebrae, excess growth of marrow in temporal, frontal and facial skeleton causing obliteration of paranasal sinuses vascular impressions in tubular bones, metaphyseal abnormalities of long bones | Javid B et al., [3]Guangbin Z et al., [4]Tunaci M et al., [8]Akpek S et al., [9] |
| MRI scan | Sites of extra medullary haematopoiesis at posterior paravertebral, mediastinal, or presacral masses, widened diploic spaces | Tyler PA et al., [7] Tunaci M et al., [8]Guangbin Z et al., [4]Dinan D et al., [15] |
| CBCT | Widening of medullary spaces and thinning of cortices, high angle Class II skeletal growth pattern with increased ANB angle | Bougilia S et al., [1]Akurt A et al., [6] |
CT: Computed tomography; MRI: Magnetic resonance imaging; CBCT: Cone beam computed tomography; ANB: Angle between point A, nasion and point B
Clinical Characteristics
Thalassaemia major is a life-threatening condition with extreme clinical symptoms and orofacial defects while thalassaemia minor can be asymptomatic or present with mild morphological abnormalities [6].
Thalassaemia major requires blood transfusion without which severe anaemia leads to death in infancy. Haemoglobin levels in thalassaemia intermedia patients are approximately 6-7 g/dL without transfusion favoring normal growth and survival in them [2]. Beta thalassaemia does not show any manifestation till six months of age while alpha thalassaemia defects are observed at birth or from embryonic life [1].
Other clinical manifestations include extramedullary haematopoiesis, haemosiderosis, and accumulation of haemolytic products. Splenomegaly, hepatomegaly, cardiac enlargement and congestive heart failure may be secondary to anaemia [4].
Oral and Maxillofacial Manifestations
The most characteristic oral and maxillofacial skeletal changes are mongoloid features, slanted eyes, chipmunk faces with prominent frontal and parietal bossing, prominent cheek bones, depressed nasal bridge, hypertrophied maxilla and mandible due to active bone marrow hyperplasia. Oral mucosa and gingiva may present with pale bronze colour mucosal pigmentation [7].
Typical Radiological Manifestations
A) Conventional Radiographs
The conventional radiography is widely employed and serves as the source for detection of early and late manifestations of the disorder. The Postero-anterior and lateral skull projections may be employed for demonstration of the features. There may be appearance of wide medullary spaces and trabeculae of maxilla giving a characteristic ‘chicken wire’ appearance. Long bones may demonstrate osteoporosis and generalised radiolucency with thinning of cortical plates which might be a source for pathological fractures. Vertebral bodies may display typical granular or ground glass appearance. Hand-wrist views of the phalanges may demonstrate rectangular or biconcave features. Cranial vault characteristically presents ‘hair on end’ appearance on lateral skull view [7].
Osteoporosis may be due to ineffective erythropoiesis causing extreme expansion of marrow spaces in long bones, spine, skull, facial bones and ribs.
Chronic anaemia in thalassaemia may lead to medullary expansion of bone marrow, thinning of cortical bone, diminishing cancellous bone due to resorption and widening of diploic spaces. Epiphysis of long bones fuses prematurely leading to short proximal humerus and thus affects the height of the person [1].
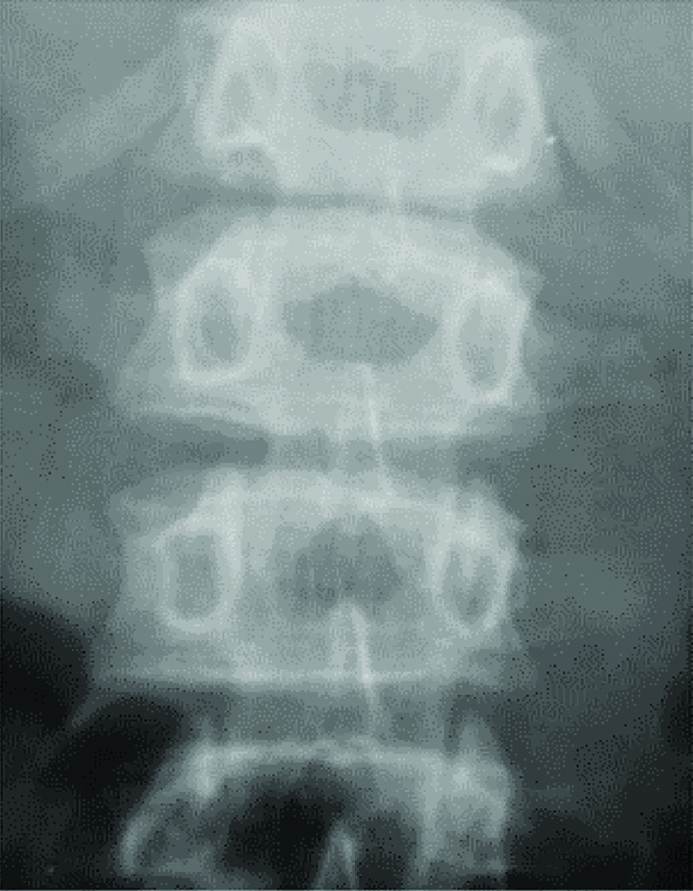
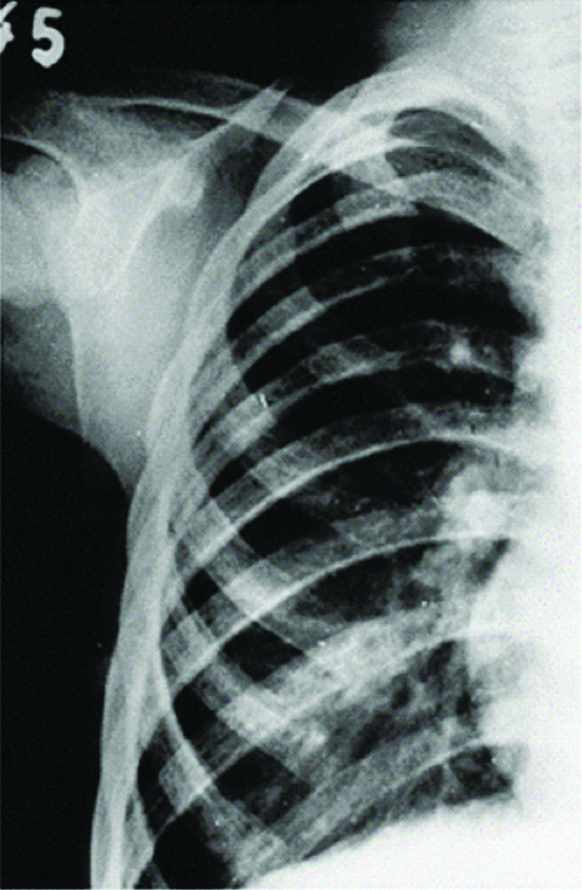
Ribs, spine vertebrae, skull bones, scapula, sternum are also involved [3]. Anteroposterior views of spine shows ‘bone-within-bone’ appearance [Table/Fig-3]. Therapy with desferrioxamine causes retarded growth and premature fusion of growth plates in tubular bones [4]. Cortex is perforated by hypertrophic marrow and extends longitudinally under the periosteum concealing the original developing rib which presents as ‘rib-within-rib’ on radiograph [Table/Fig-4] [8].
Anteroposterior view of lumbar spine showing bone-within bone appearance [7].
Courtesy: Tyler PA, Madani G, Chaudhuri R, Wilson LF, Dick EA. The radiological appearances of thalassaemia. Clin Radiol 2006;61(1): 40-52
Rib-within-rib appearance [8].
Courtesy: Tunaci M, Tunaci A, Engin G, Ozkorkmaz B, Dinçol G, Acunaş G. Imaging features of thalassaemia. Eur Radiol. 1999;9(9):1804-9.
Diffuse osteoporosis in thalassaemia patients is due to mechanical pressure from hyperactive erythroid marrow [9]. Other skeletal features are osteopenia, erosion, scoliosis, cord compression, paraspinal mass, fracture, rib erosion, rib widening and cortical thinning [10].
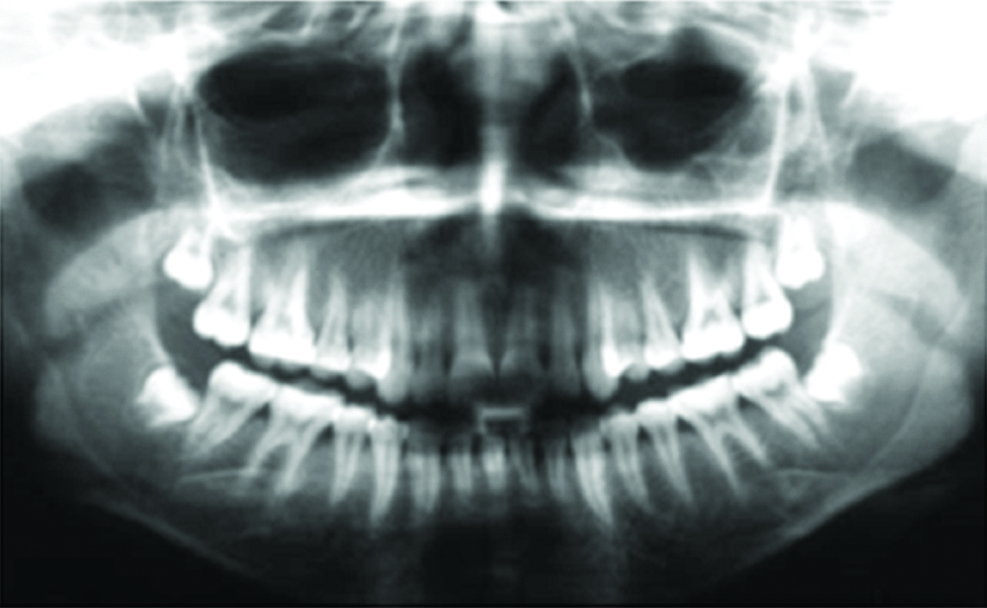
The panoramic projection may exhibit dilated vascular canals, prominent antegonial notch, spiky, short rooted teeth exhibiting taurodontism, diminished lamina dura, enlarged bone marrow spaces, small maxillary sinuses, non-appearance of inferior alveolar canal and thin cortex of the mandible [11].
Spiky roots are seen mostly in mandibular 1st molar followed by mandibular 1st premolar. Taurodonts tend to prevail in maxilla than in mandible and also maxillary 1st molar area is most commonly involved followed by mandibular molar. Lamina dura may be thin with posterior mandibular region presenting large marrow spaces [Table/Fig-5]. Maxillary sinuses may be small or totally absent in certain patients [11,12].
Panoramic radiograph presenting mandibular molars with thin spiky roots [11].
Courtesy: Hazza’a AM, Al-Jamal G. Radiographic features of the jaws and teeth in thalassaemia major. Dentomaxillofacial Radiol. 2006;35(4):283-88.
Skull radiograph may present with widened diploic spaces with thin, displaced outer cortical table. Marrow overgrowth in maxilla leads to laterally displaced orbits and forwardly displaced incisors giving typical rodent face to thalassaemia patient. Perpendicular orientation of trabeculae to cortical table produces radial pattern called as “hair-on-end” pattern [8]. The trabeculae are alternating opaque, thickened and bone marrow is radiolucent hyperplastic presenting typical hair-on-end appearance on skull radiographs [Table/Fig-6].
Hair-on-end appearance on lateral skull view and PNS [13].
Courtesy: Basu S, Kumar A. Hair-on-end appearance in radiograph of skull and facial bones in a case of beta thalassaemia. Br J Haematol. 2009;144(6):807.
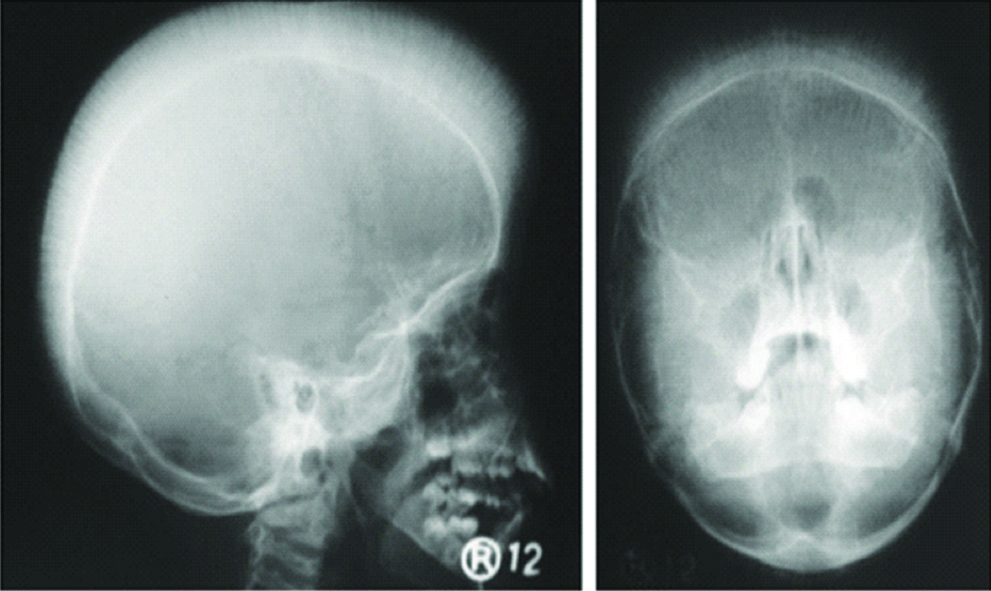
Diploic widening is first manifested in frontal region. Occipital bone is spared may be due to its lower marrow content. Typically, well-circumscribed solitary or multiple lytic lesions are usually evident. Hyperplasia of marrow spaces in frontal, temporal and maxillary sinus decreases pneumatization of the sinuses in the skull. Paranasal and frontal sinuses may not appear along with obliterated mastoid spaces. Exceptionally, the ethmoid air sinuses are spared evidently due to scantiness of red bone marrow within the surrounding bones [7].
B) Advanced Imaging Modality
1. Computed Tomographic Features: Increased diameter of diploic space of bony calvarium as well as maxillary facial body structures may be seen. The prominence of bony structures may lead to narrowing of optic foramen; obliteration of nasal cavity and paransal sinuses except ethmoidal sinuses which can be viewed in coronal CT scans [Table/Fig-7] [3].
Coronal Computed Tomography (CT) scans of the patient without contrast, indicating (a-d) generalised marrow hyperactivity affecting the maxillofacial skeletal system, (b) narrowing of the optic foramen (arrow), (c and d) thickened calvarias (arrows), and narrowing of the frontal sinuses (asterisk) [3].
Courtesy: Javid B, Said-Al-Naief N. Craniofacial manifestations of β-thalassaemia major. J Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119(1):33-40.
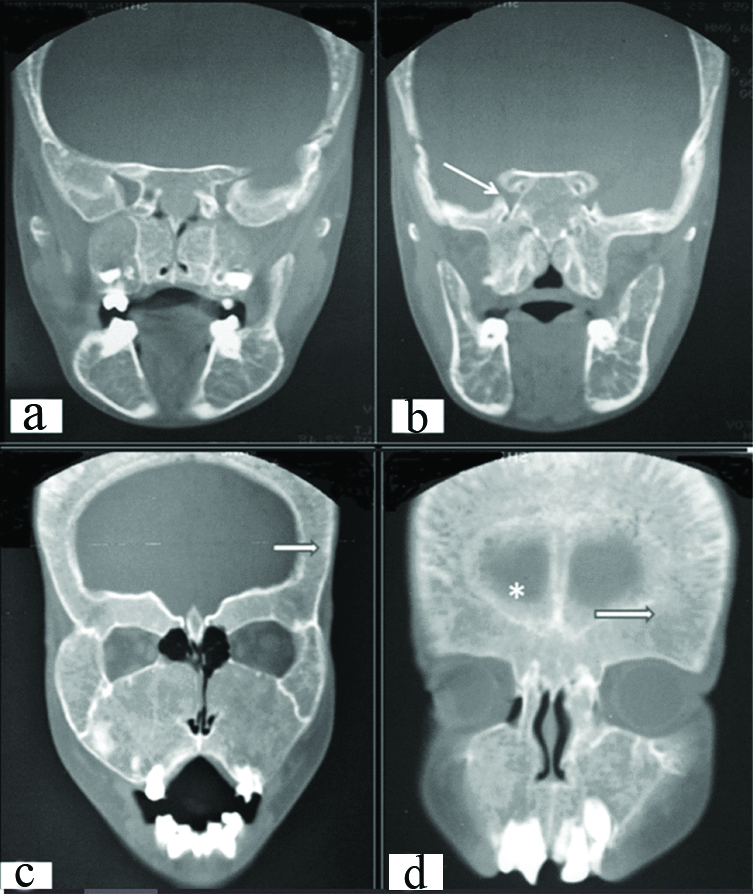
The ribs are expanded at the sites of attachments to the vertebral column [4]. Anterior and middle part of ribs may demonstrate “rib-within-rib” appearance.
There can be compression fracture of vertebrae causing neurological defects due to cortical thinning and osteoporosis which presents as a prominent feature. The sites of extramedullary hematopoiesis are posterior mediastinal, paravertebral, or presacral masses due to extraosseous extension of medulla. Vascular impressions in tubular bones and metaphyseal abnormalities may be noticed [4]. Increased overall attenuation values of trabecular bone may be attributed to iron deposition in bone tissue in beta thalassaemia patients [9].
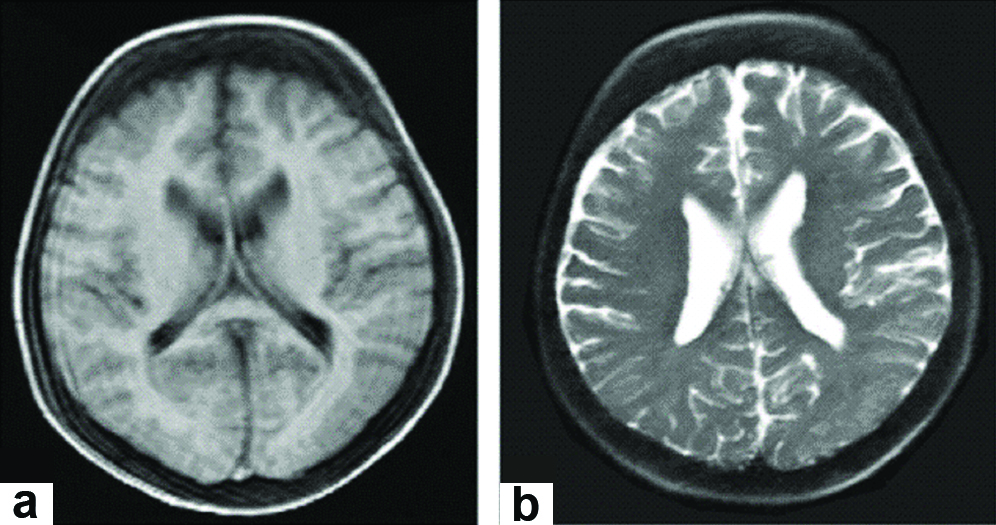
2. MRI Features: The MRI appearance of marrow in thalassaemia is characteristic and may be due to fusion and chelation therapy. Iron deposition despite chelation therapy may occur in active red marrow. In thalassaemia, posterior paravertebral, mediastinal, or presacral masses represent sites of extramedullary hematopoiesis resulting from extraosseous extension of medullary tissue. Epidural extension can cause cord compression. Platyspondyly generally may be associated with hyper transfused thalassaemic patients [8]. Widened diploic spaces may be depicted as hypointense areas in T1, T2 and proton weighted images. Excess growth of marrow in temporal, frontal and facial skeleton consistently impedes pneumatization of paranasal sinuses [Table/Fig-8].
a. T1W and b. T2W axial MR images show thickening of cranial bones diploe [4].
Courtesy: Guangbin Z, Xianomei WU, Xuelin Z, Meiyou WU, Aingsi Z, Xinchun LI. Clinical and imaging findings in thalassaemia patients with extramedullary hematopoiesis. Clin Imag 2012;36(5):475-82.
3. CBCT Features: Computed tomography 3D reconstruction shows widening of medullary spaces and thinning of cortices. There is reduced volume of maxillary sinus pneumatization due to marrow expansion within maxilla [1].
Lateral Cephalometric images obtained from CBCT scan presented with high angle Class II skeletal growth pattern with increased ANB angle [6].
Abbreviations
CBCT: Cone beam computed tomography; ANB: Angle between point A, nasion and point B.
Conclusion
Literature is abundant with radiological manifestations of thalassaemia with respect to conventional radiographs, CT and MRI. Generally, skull radiographs are sufficient to define the osseous abnormalities of thalassaemia. CT and MRI images further depict the bone marrow changes. After advent of CBCT the usage of the same should be incorporated on day to day basis because of advantages offered over other modalities. This paper highlights the need for further exploration of these manifestations by CBCT to facilitate evidence based practice approach.
CT: Computed tomography; MRI: Magnetic resonance imaging; CBCT: Cone beam computed tomography; OPG: Orthopantamograph
CT: Computed tomography; MRI: Magnetic resonance imaging; CBCT: Cone beam computed tomography; ANB: Angle between point A, nasion and point B