Fracture Neck of Femur with Proximal Femoral Nail Antirotation Insitu: A Rare Case
Sunil Lakshmipura Krishnamurthy1, Surendra Umesh Kamath2, Rajendra Annappa3, Aditya Vardhan Guduru4
1 Senior Resident, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Karnataka, India.
2 Professor and Head, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Karnataka, India.
3 Assistant Professor, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Karnataka, India.
4 Postgraduate, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil Lakshmipura Krishnamurthy, Kasturba Medical College, Manipal Academy of Higher Education, Mangalore-575001, Karnataka, India.
E-mail: sunilmurthylk@gmail.com
Hip fractures are common in elderly population due to osteoporosis. Proximal Femur Nail Antirotation (PFNA) system has gained more importance in management of peritrochanteric fractures than conventional Proximal Femur Nail (PFN) due to ease of application and low complication rate. We report a case of a 64-year-old male patient who has sustained fracture neck of femur, seven months’ post PFNA. It’s a rare association to have fracture neck of femur with PFNA insitu and hence reported. Patient treated with removal of implant and hemi-replacement of hip.
Hemiarthroplasty, Osteoporosis, Peritrochanteric fractures
Case Report
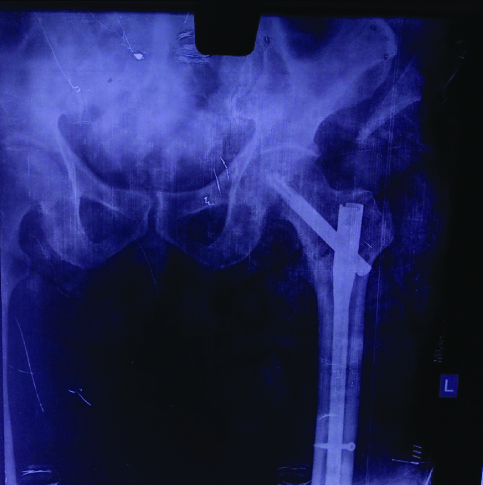
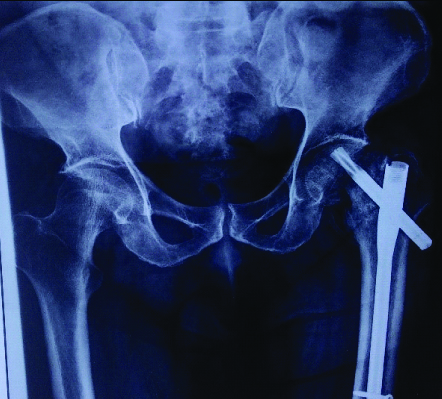
A 64-year-old male patient, came to emergency department with complaints of pain in left hip and inability to walk since two weeks. Pain was acute in onset, developed following trivial fall at home. Patient had taken analgesics; he consulted, when he found no improvement in his symptoms. Records of patient showed, he had sustained stable intertrochanteric fracture femur and had undergone fixation with proximal femoral nail antirotation system seven months back [Table/Fig-1,2]. Post-surgery patient was kept on non-weight bearing mobilisation for one month and partial weight bearing later for another month, followed by full weight bearing mobilisation. Patient had gained his hip range of motion and fracture united at the end of five month post surgery radiologically.
Previous X-ray which shows intertrochanteric fracture of femur.

X-ray shows fracture which was stabilised by PFNA.
Patient was moderately obese with BMI of 32.4, with no significant medical illness; on inspection his left lower extremity was externally rotated compared to normal side, three linear scars of about 4 cm, 3 cm, 1.5 cm presented on later aspect of thigh suggestive of previous scars. On palpation, he had joint area tenderness; also his movements were grossly restricted in all planes.
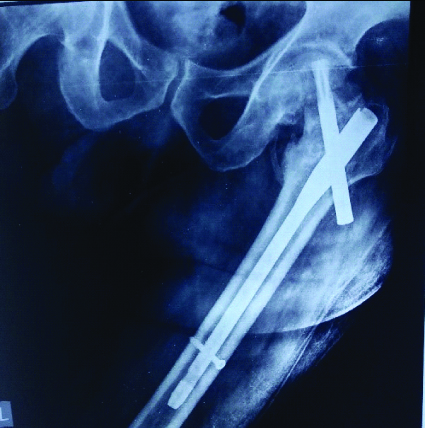
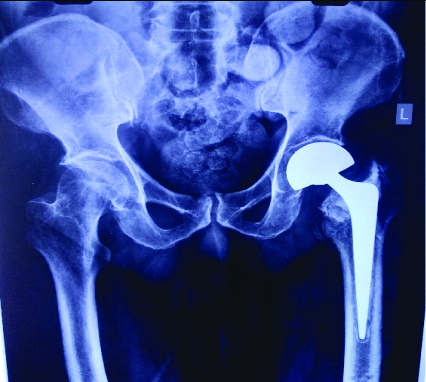
X-ray of pelvis with bilateral hip showed, fracture neck of femur with proximal femur nail with antirotation screw in-situ with previous healed intertrochanteric fracture and normal hip joint space [Table/Fig-3,4]. The blood investigations revealed a normal haemogram, normal liver and renal functions. Chest X-ray and 2D echo were within normal limits.
Fracture neck of femur with implant insitu (AP view).
Fracture neck of femur with implant insitu (lateral view).
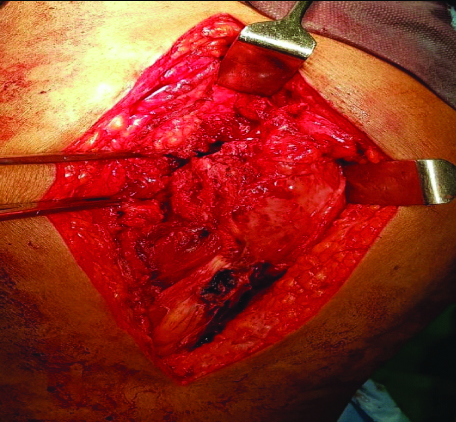
In view of his functional disability and pain, we decided to treat patient with cemented hemiarthroplasty of hip. Patient was positioned in lateral position following spinal anaesthesia. Hip joint was opened by lateral approach to hip. Intraoperatively our previous intertrochanteric fracture was found to be united, we removed PFNA nail after removing helical screw and distal screw [Table/Fig-5]. Hip was dislocated anteriorly, neck cut made, head extracted out, femur preparation done and cemented bipolar hemiarthroplasty prosthesis was placed. Hip reduced and found stable. Capsule and muscles and fascia were sutured with absorbable sutures, skin closed with staples.
Intraoperative photograph.
Postoperative period was uneventful and wound healed well. Patient was on full weight bearing mobilisation on postoperative day two with walker, and was discharged on postoperative day five. Patient followed up at four weeks and eight weeks and clinically and radiologically patient is doing well [Table/Fig-6]. Patient was mobilised without support at end of eight weeks. Currently, its six months follow-up post procedure and patient had attained good range of movement and had resumed his occupation activities.
Postoperative radiograph.
Discussion
Osteoporosis is most common reason for pathological fractures around hip [1]. Proximal femur fractures need to be treated at earliest or else associated with untoward complications. Treatment of peritrochanteric fractures are constantly evolving over past 2 to 3 decade. Treatment of intertrochanteric fractures is done with PFNA, as they are associated with less complication compared to conventional PFN. Conventional PFN have 2 neck screws which requires expertise in proper positioning of screws to minimise z effect and reverse z effect. PFNA is a novel device with helical blade which is applied by impaction to head of femur, this compaction limits rotation and varus collapse [1,2].
There are few studies which shows complications associated with PFNA nailing like, implant break out, implant cut through, perforation to acetabulum, peri implant fracture with distal to tip of nail, fracture femur shaft during procedure [3,4].
Helical blade in PFNA prevents collapse and adds to stability of fracture, blade act as internal splint and helps in transmitting weight across construct. However, even though intertrochanteric fracture united in our patient, yet patient developed fracture neck of femur with implant insitu following fall which is extremely rare association. Hence, we are reporting this case.
Patient was treated with hemi arthroplasty of hip for fracture neck of femur after implant removal [5,6]. Patient had relatively normal acetabulum and hence entire hip was not replaced and patient gained movement at hip and resumed his regular activities and occupation activities post-procedure.
Conclusion
Treatment of intertrochanteric fractures has evolved and PFNA has surpassed management over conventional PFN. However, the unusual association of neck of femur fracture, following trivial fall with PFNA implant insitu opens up option to study implant design.
[1]. Xue L, Zha L, Chen Q, Liang YJ, Li KR, Zhou Z, Randomized controlled trials of proximal femoral nail antirotation in lateral decubitus and supine position on treatment of intertrochanteric fracturesSci World J 2013 2013:27601510.1155/2013/27601523606811 [Google Scholar] [CrossRef] [PubMed]
[2]. Loo WL, Loh SYJ, Lee HC, Review of Proximal Nail Antirotation (PFNA) and PFNA-2–Our local experienceMalaysian Orthopaedic Journal 2011 5(2):10-14.10.5704/MOJ.1107.001 [Google Scholar] [CrossRef]
[3]. Liu JJ, Shan LC, Deng BY, Wang JG, Zhu W, Cai ZD, Reason and treatment of failure of proximal femoral nail antirotation internal fixation for femoral intertrochanteric fractures of senile patientsGenet Mol Res 2014 13(3):5949-56.10.4238/2014.August.7.1025117353 [Google Scholar] [CrossRef] [PubMed]
[4]. Kini SG, Hin LC, Haniball J, Lateral cortex blowout during PFNA blade insertion in a subtrochanteric fracture-Should bone quality determine the type of nail used? Chinese J TraumatolEnglish Ed 2015 18(2):116-19.10.1016/j.cjtee.2014.11.00326511307 [Google Scholar] [CrossRef] [PubMed]
[5]. Ono NK, Andrade Li, Honda GD, Ploesello EK, Guimaraes GC, Junior RP, Hemiarthroplasty in the treatment fractures of the femoral neckRev Bras Ortop 2010 45(4):382-88.10.1590/S0102-3616201000040000727022567 [Google Scholar] [CrossRef] [PubMed]
[6]. Jain V, Kamath SU, Tejaswi P, Hegde AS, Unipolar versus bipolar uncemented modular hemiarthroplasty in patients with displaced femoral neck fractures: A three year follow-upAsian J Pharm & Clin Res 2016 9(4):173-76. [Google Scholar]