The “floating elbow” term is simply used to delineate the different injuries in one heading. Combined supracondylar fracture of humerus with ipsilateral fracture of forearm bone, is not a common injury. Literature with the largest case series of supracondylar humerus fracture and even some textbook of paediatric orthopaedics does not enumerates such combination of injury [1].
Simultaneous ipsilateral fracture of supracondylar humerus and fracture both bone forearm causes the functional dissociation of elbow with the rest of the body and resulted in “floating elbow”. Initially the term “floating elbow” was restricted for ipsilateral humeral and forearm shaft fractures [2,3]. But now, term “floating elbow” also includes the intra-articular fracture of distal humerus and elbow dislocation along with forearm shaft fractures. Because such injuries also lead to functional joint dissociation with the rest of the upper limb, so these variants are also conceded as “floating elbow” injury [4,5]. So, in this study we also included the cases of ipsilateral forearm fracture and intra-articular fracture of distal humerus which finally culminates to functional floating elbow. Albeit there is paucity of this topic in Indian literature, so we want to bring it to horizon of knowledge with mentioned seriousness and rarity of this injury. Hence, the aim of the present study was to evaluate the cases of floating elbow presented to us in past four years.
Materials and Methods
This was a prospective interventional study of floating elbow injury sustained by the children presenting to orthopaedic emergency department at one of the transcendent tertiary care hospital of central India from December 2013 to December 2017. We included the children (Range: 4-16 years) who approached the Hospital with displaced fracture of humerus with ipsilateral displaced fracture of single or both bone forearm (Floating elbow). Patients with un-displaced fracture, older age group, pathological fracture, elsewhere treated and neglected cases of floating elbow injury were excluded from the study. The variables of study were age, sex, side, and mode of injury, fracture classification, injury-to-surgery interval, executed treatment, pre and post-op complications.
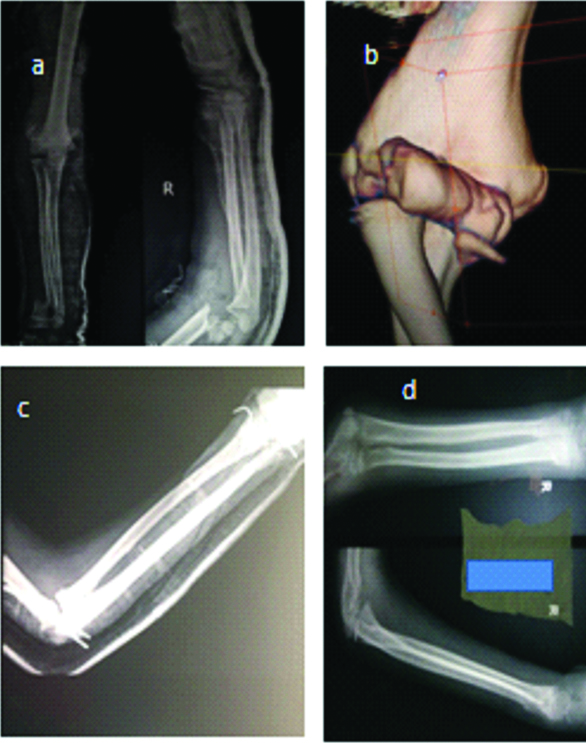
There is no universally or officially accepted classification of floating elbow, which standardises the management protocol. Cuéllar ER et al., proposed the classification of floating elbow based on mode of injury, duration of injury and fracture level [6]. It is categorised into six types and gives a comprehensive idea of management and prognosis. So in this study the Cuéllar-Nieto classification was used to classify the all floating injuries [Table/Fig-1]. All the cases were managed on the emergency basis with closed/open reduction and fixation with Kirschner wires. None of them were chosen to be treated by conservative mean. Based on the complexity of the trauma and further intervention, the patients were called at regular follow-up. [Table/Fig-2a-d] is showing the pre-op, post-op and follow-up of Cuéllar-Nieto type I fracture in nine years old child. Other few cases are shown in [Table/Fig-3,4 and 5] with details.
Cuellar-Nieto Classification of floating elbow.
| Type I-Distal metaphyseal fracture of the humerus with metadiaphyseal fracture of the radius and/or ulna, with <20° of volar angulation with lateral displacement <90°. |
| Type II-Humeral diaphyseal fracture plus metaphyseal fracture of the ulna and/or radio, with >20° of volar angulation with independent lateral displacement. |
| Type III-Humeral diaphyseal fracture plus metaphyseal fracture of the ulna and/or radius, with >20° of volar angulation and >90° of lateral displacement. |
| Type IV-Open fracture in Types I, II, or III with neurovascular compromise. |
| Type V-Open fracture in Types I, II, or III within less than 6 hours. |
| Type VI-Open fracture in Types I, II, or III within more than 6 hours. |
Radiograph (case 1) showing floating elbow in a nine years old child who fell down from height had Cuéllar-Nieto type I fracture. Preoperative radiograph (a), preoperative CT image (b), immediate postoperative image (c) and final follow-up radiographs.
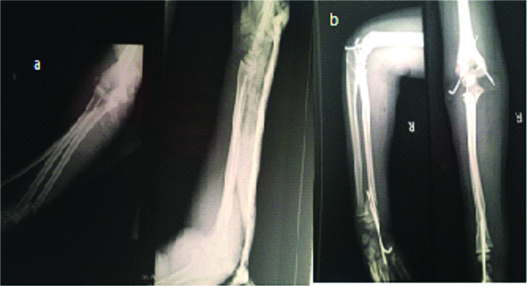
Case detail (case 2) showing floating elbow in a 12 years old child who slipped from tree and suffered with Cuéllar-Nieto type V fracture showing preoperative radiograph (a) and immediate postoperative (b) image.
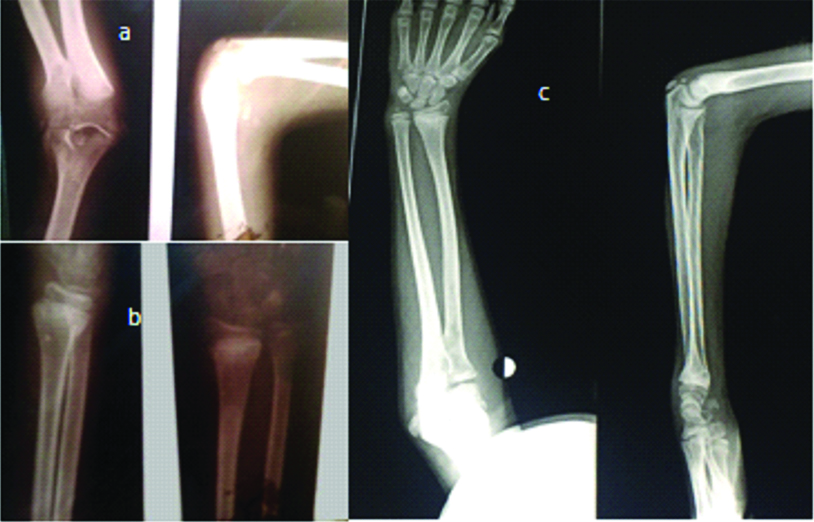
Radiograph (case 3) showing floating elbow in a ten years old male. Preoperative radiographs of elbow and wrist (a) showing fracture of supracondylar humerus and (b) fracture of distal end radius respectively. Fractures were managed by closed reduction and K-wire fixation and follow up image (c) at 1year.
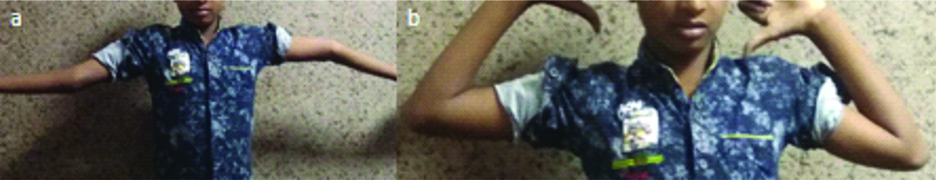
Follow-up (case 4) of floating elbow (Cuéllar-Nieto type I) right side in 11 years old boy. a) Flexion and b) extension movements were terminally restricted (arc of motion 100 degree).
The average follow-up of the study was 20 months (range 15-30 months). All cases underwent serial clinical and radiographic detail at each follow-up. The last clinical follow-up was enumerated by Mayo Elbow Performance Score (MEPS) and Khalfayan score [7,8]. MEPS includes the evaluation of pain, range of motion, grip power at wrist and elbow, stability and day to day activity (excellent >90, good 75-89, fair 60-74, poor <60). The parameters evaluated in Khalfayan scoring system were pain, motion, elbow and grip strength, and function in activities of daily living (excellent 90-100, good 80-89, fair 70-79, poor <70).
We started early rehabilitation of the elbow during the recuperation period. After one week, active-assisted flexion and extension (uniplaner) exercise started, except for two cases of intra-articular fracture. In such cases we did it after 2 weeks. There were two removable slab (one in full flexion and second in full extension) which were made to wear alternatively for the rest of the time. When the obvious callus was formed, then the rotational movements started.
The statistical calculation was done with Microsoft XL 2007 (data add in function were installed for data analysis). Due to absence of comparison group, this study was conceded as descriptive study of floating elbow.
Results
In this study, we evaluated the patients of paediatric age group who sustained the injury of floating elbow. Nineteen patients were included in the case series but, two patients were not traceable over follow up period so our result was based on seventeen complete case records.
The average age was 9.58 years (Range 6-15 years) with the male and female ration of 11:6. The injury was more common on right side (65%) in 11 patients. In present series most common encountered mode of injury was fall from height (76%) in thirteen patients, followed by Road Traffic Accident (RTA) and cycling in (18%) three and (6%) one patient respectively [Table/Fig-6]. Open fracture happened in 5 (29%) patients, in which two patients had open supracondylar fracture of humerus, two patients had open fracture of both bone forearm and one patient had the open fracture of supracondylar humerus as well as fracture of both bone forearm too.
Demographic profile of study population with details of injury classification, treatments, complication and results.
| S. No. | Age (Yrs)/sex | Cuellar-Nieto classification | Side | Mode of trauma | Injury-to-surgery interval | Pre-op Complications | Post-op Complications | MPES | Khalfayan score |
|---|
| 1 | 8/M | Type I | R | Fall from height | 1 day | | | 93 | 90 |
| 2 | 8/F | Type I | R | Fall from height | 8 hours | | Pin tract infection | 80 | 83 |
| 3 | 15/M | Type VI | L | RTA | 8 hours | | | 69 | 70 |
| 4 | 6/M | Type IV | R | Fall from height | 12 hours | | | 93 | 94 |
| 5 | 10/M | Type VI | R | Fall from height | 2 days | | Pin tract infection | 71 | 68 |
| 6 | 10/M | Type III | L | Fall from height | 2 days | Compartment syndrome | Skewed union | 60 | 70 |
| 7 | 7/M | Type I | R | RTA | 1 day | | | 69 | 65 |
| 8 | 11/F | Type V | R | Fall from height | 4 hours | | Pin tract infection | 71 | 70 |
| 9 | 11/M | Type VI | L | Fall from height | 1 day | | Skewed union | 71 | 71 |
| 10 | 11/M | Type I | R | RTA | 12 hours | | | 89 | 90 |
| 11 | 12/F | Type I | R | Cycling | 12 hours | | Nerve (Ulnar) inury | 69 | 65 |
| 12 | 10/F | Type III | L | Fall from height | 1 day | Median nerve injury | | 65 | 66 |
| 13 | 8/M | Type I | R | Fall from height | 12 hours | | | 70 | 70 |
| 14 | 7/F | Type I | L | Fall from height | 3 days | | | 94 | 96 |
| 15 | 9/M | Type I | R | Fall from height | 1 day | | Skewed union | 70 | 70 |
| 16 | 9/F | Type I | L | Fall from height | 1 days | | | 95 | 94 |
| 17 | 11/M | Type VI | R | Fall from height | 1 day | | Pin tract infection | 61 | 65 |
Two patients (11.7%) suffered from pre-op complications. One of them had compartment syndrome, for which fasciotomy was done and one had median nerve injury which recovered during the follow-up. Post-op complications occurred in 8 patients (47%) and its distribution was pin tract infection in 4 (23.5%), skewed union in 3 (17%) and ulnar nerve injury in one (5.8) patient. Superficial pin tract infection subsided by next week, but the ulnar nerve injury did not improve.
Clinico-radiological obvious fracture healing was noticed at average of 9 weeks (range, 6-13 weeks). The final average range of movement was 95 degree (range, 15-110 degree), with the 80% of elbow strength (range 60-100%) and grip strength of 90% (range 70-100%) in the comparison to uninvolved side. The functional results of the study as per the MPES were as follows-4 patients (24%) with excellent result, 2 patients (12%) with good result, and 11 patients (64%) with fair result [Table/Fig-6]. Average score of overall MPES was 74.78 (max-95, min-60). Functional results of Khalfayan scoring system were as: 5 patients (29.4%) with excellent result; 1 patient (6%) with good result; and 6 patients (35.2%) with fair result, 5 patients with (29.4%) poor result [Table/Fig-6]. Average score of overall Khalfayan score was 76.29 (max-96, min-65).
Discussion
Initially, the floating elbow injury was used to be managed by conservative method [9,10]. There are literature which found that incidence of loss of reduction occurred in 7% to 25% cases of floating elbow injuries managed by conservative methods [11,12]. Williamson DM et al., in his study, percutaneously fixed the supracondylar fracture only and applied the cast for forearm fracture. They concluded that there was longer hospitalisation period, which manifested in the form of financial and psychological overload [13].
Combination of the ipsilateral fracture of both bone forearm and distal humerus is an uncustomary entity [14,15]. The constellation of skeletal trauma with combined forearm and distal humeral fracture (floating elbow) has the incidence of 3-13% [16]. Contrary to isolated fracture, the floating elbow injury is high energy trauma and poses the difficulty in treatment. Management strategy of floating elbow injury has been changing constantly over time from closed reduction with posterior slab, olecranon traction to the K-wire pinning.
Though, the term floating elbow seems the extra simplification of injury components. But the nomenclature of such complex and severe injury by such vague term seems “fancy” but grossly inappropriate. In spite of this loophole, the term “floating elbow” is widely used. Collectively, floating elbow is a principally complex trauma (Simpson and Jupiter) and entails the complications like infection, myositis, reduced range of movement, and functional impairment of limb. So with time, Simpson and Jupiter attempted to accurate the equivocation of this term [17].
Floating elbow injury is associated with increased incidence of compartment syndrome (up to 33%) and higher chance of redisplacement of fracture if managed by slab or cast. So the authors have advocated pinning to fix both fracture, which permits the close observation of neurovascular status as well as reduces the complications like compartment syndrome and redisplacement, in comparison to conservative management of floating elbow [18]. Rogers JF et al., reported that non-union occurred in humerus of all cases of floating elbow injury, if managed without the rigid fixation [19]. So the stable external/internal fixation of all the fracture has been advocated as management protocol for floating injury. And now-a-days, the general consensus favours the surgical intervention. So in present series, all the cases were managed by close/open reduction and K-wire fixation.
The preference of fixation varies among authors. Even after diligent search, no definitive study could be found which prioritised the fixation order for supracondylar fracture or forearm injury of floating elbow. Some authors have favoured to first fix the supracondylar fracture. They assumed that by this, neurovascular access of limb and fracture reduction will be easier. And the management of open fracture and dressing would have posed difficulty, if the forearm fracture would have been managed firstly [20]. But in this study, fixing the forearm fracture in all cases was prioritised. Because we thought that, dangling of forearm during supracondylar fracture reduction may ensue soft tissue injury and compartment syndrome. Secondarily the supracondylar fracture reduction needs supination and pronation, and it will be difficult if forearm fractures could not have been managed.
The comparative results of the present study with few previously published literatures are discussed below [Table/Fig-7]. Ring D et al., (n=16), found no complication in 6 patients who were managed by percutaneous fixation, but in 10 patients in which closed reduction and cast application was done, 6 out of 10 patients had compartment related syndrome and they further required the intervention and rest 4/10 patients had normal post-op period [18]. In a subsequent year Tabak AY et al., fixed the all, (n=22) forearm fracture as well as the supracondylar fracture of humerus in floating elbow cases and the post-op period was uneventful without any complication [21]. Suresh SS also managed his all cases of floating elbow injuries by percutaneous K-wire fixation and got the promising results [22].
Comparison with previously published study of floating injury in children.
| Seriol no. | Series | No. of cases | Management | Complications |
|---|
| 1 | Ring D et al., [18] | n=16 | 10 patients-CR and cast6 patients-CR and K-wire pinning | 2/10-developed compartment syndrome, 4/10-had incipient compartment and rest 4/10 had normal course.No complication. |
| 2 | Tabak AY et al., [21] | n=22 | All patients were addressed by CR and K-wire pinning for all fracture. | No complication. |
| 3 | Suresh SS [22] | n=4 | All patients were addressed by CR and K-wire pinning for all fracture. | No complication. |
| 4 | Dhoju D et al., [23] | n=31 | 9 patients-CR and cast22 patients-CR and K-wire pinning | 1/9-impending compartment syndrome.2/22-post-op ulnar nerve palsy and 3/22 had pin tract infection. |
| 5- | Blumberg TJ et al., [24] | n=47 | All supracondylar humerus fracture was operatively managed.All of the displaced (21/47) forearm fracture was closely reduced and non-circumferential splint applied. | None of them developed compartment syndrome or loss of reduction. |
| 6 | Our study | n=17 | All patients were addressed by K-wire pinning for all fracture. | 1/17-Ulnar nerve injury.2/17-Skewed union. |
Dhoju D et al., in their series (n=31) conservatively managed the 9 patients of floating elbow. And only one patient developed the impending compartment syndrome; while the rest 22 patients, were managed by percutaneous K-wire fixation. In the two patients, post-op ulnar nerve injury occurred but no other obvious complications were noticed [23]. Blumberg TJ et al., in his study they fixed the all (n=47) supracondylar fracture of humerus and the displaced forearm fractures were reduced and managed by back slab and obtained the excellent result [24]. Present study also followed the same protocol and all fracture component were fixed. In the present series there was one case in which iatrogenic ulnar nerve injury occurred and in two cases skewed union happened.
Limitation
Despite the favourable result, this study has its own limitations like, single center study, small number of cases (due to rare injury) and absence of control group. Study included only the paediatric age group patients so the same outcome cannot be expected in adults. Presumably the larger sample size, multicenter study and wider age group variation study is needed in near future to withdraw the better and more precise and prognostic inference.
Conclusion
Floating elbow is a serious injury with wary outcome. Injury type is out of the way and treatment recommendations are polemical. In this literature the better results could have obtained due to surgical intervention in all cases. So it can be emphasised that floating elbow injury can be best treated by aggressive surgical intervention. The less invasive approach or percutaneous techniques seems to be better to treat this injury. Prompt intervention with soft tissue preservation and early rehabilitation offer the better course to patients. At the end of the closure of this article we realised that floating elbow injury is province of large knowledge gap which entails the plentiful space for continuous investigation.