Introduction
Neutrophil-to-Lymphocyte Ratio or NLR is a ratio used as a marker for ongoing inflammation process and is independently related to poor clinical outcomes among liver cirrhosis patients.
Aim
To determine any significant correlation between NLR and Child-Turcotte Pugh (CTP) score among decompensated liver cirrhosis patients in a tertiary referral centre in Medan, Indonesia.
Materials and Methods
The cross-sectional study involved patients diagnosed with liver cirrhosis in Haji Adam Malik General Hospital, Medan, Indonesia between May 2016-May 2017. The study enrolled 54 cirrhotic patients, regardless of aetiologic agent. CTP score was fulfilled by using two methods, bilirubin, albumin, and INR was noted from medical record registry and the rest, ascites and encephalopathy, were assessed using physical examination and interview process on the same day of the patient admission. Spearman correlation test was performed to determine the correlation between two variables, while the demographic characteristic was presented in a single table with mean or median and standard deviation in it.
Results
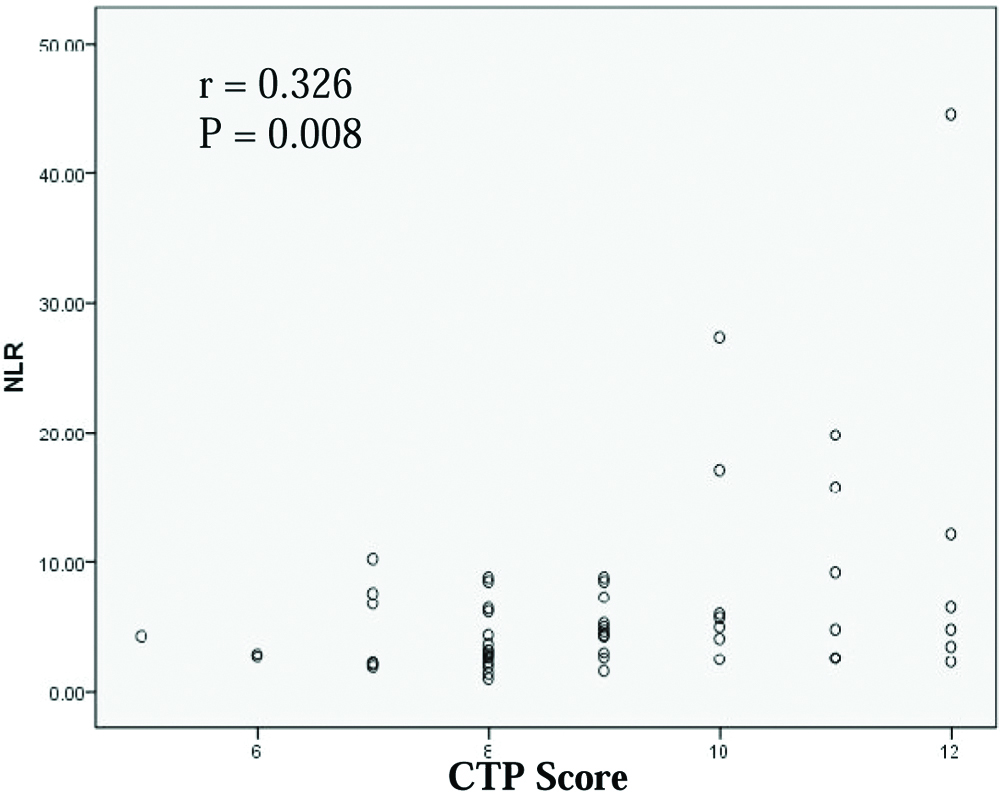
A significant correlation between NLR and CTP score was obtained (p=0.008) and it was positively correlated (r=0.326).
Conclusion
Shifting use of CTP score to NLR ratio still needs further study to acknowledge its potential as mortality and prognosis predictor independently.
Hepatic failure, Inflammation, Leukocyte
Introduction
Cirrhosis of the liver is generally known as an end-stage process where healthy normal liver tissue is replaced by the abnormal, connective tissue, and it induces nodule formation in it [1,2]. Liver cirrhosis commonly occurs as the result of viral infection including Hepatitis B and C virus [3,4]. In Indonesia, cirrhosis and chronic liver disease caused 49,224 deaths each year and 31 million Disability Adjusted Life Years (DALYs) worldwide, 1.2% of global DALYs. The highest mortality rate of cirrhosis patients among south-east Asia nations is found in Indonesia [5].
Therefore, the application of scoring system on primary care setting to predict the outcome and severity of cirrhotic process is mandatory since it can be used to initiate prompt and further assessment [6,7]. It is emphasised that several scoring systems can be used to predict the severity of liver failure, for instance Child-Turcotte Pugh score that consists of five variables (bilirubin level, albumin, INR, ascites, and hepatic encephalopathy) [8,9]. Similarly, Model for End-stage Liver Disease (MELD), as well as CTP, can determine severity of liver failure as well as priority for liver transplantation, health-related quality of life and the outcome [10-12].
In addition, neutrophil to lymphocyte ratio (NLR) is stated as a simple biomarker which can be used to predict systemic infection [13]. As emerging laboratory marker, NLR could be used as accurate prognostic marker to predict severity of the infection process or several types of malignancies [14-16]. High neutrophil level is associated with chronic inflammation while decreased levels of lymphocyte are linked with bacterial infection and regulator scheme [17]. Necroinflammation is one of the hallmarks of liver disease particularly in advanced cirrhosis [18]. Therefore, NLR is able to provide the information related to severity of damaged hepatocyte during fibrosis formation. Both, NLR and CTP, might be used to predict poor outcome independently [19].
Our study aimed to determine whether there was a significant correlation between high NLR ratios with severity of decompensated liver cirrhosis based on CTP score, as this was a point-time approach study, the information related to the prognosis was not noted.
Materials and Methods
The study was conducted in Internal Medicine Department, Haji Adam Malik General Hospital, Medan, Indonesia during May 2016-May 2017. All patients that were admitted in the hospital during this time interval and met the inclusion criteria were included in the study (convenience sample age above 18 years and not having any major condition including malignancy, blood transfusion in the last three months, HIV positive, diabetes mellitus, dyslipidemia, acute liver failure, autoimmune disease and pregnancy, because it could affect the laboratory result particularly leukocyte count. Thorough assessment related to medical history was carried out using patients’ medical record registry [20,21].
Secondary data was obtained from Haji Adam Malik Medical Record Registry such as demographical data (identity, history of certain disease, and history of blood transfusion) and laboratory findings (complete blood count, liver function tests, electrolyte, glucose level-both for random and fasting, lipid profile, albumin, globulin, viral marker, and haemostasis function tests). Neutrophil and lymphocyte levels were, then, transformed into a NLR. The severity of liver cirrhosis was evaluated using Child-Pugh Turcotte Score. The scale ranges from 5 to 15 points and stratified into three categories, class A (5-6), B (7-9) or C (10-15). CTP score was, then, calculated using an online calculator (https://www.mdcalc.com/child-pugh-score-cirrhosis-mortality).
Approval for the study was obtained from Medical Research Ethics Committee, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia with letter number 544/TGL/KEPK FK USU-RSUPHAM/2017 and performed in accordance with Helsinki declaration for human study.
Statistical Analysis
Statistical analysis was performed using Statistical Package for the Social Science (SPSS Inc., Chicago, IL) version 12.0 and significant results were noted as p-value<0.05 obtained from the analysis, Kruskal-Wallis test for statistical analysis was used to determine any significance in three groups since the data were not normally distributed while categorical variable, gender, was analysed using chi-square test. The correlation between NLR and severity of liver cirrhosis based on Child-Turcotte Pugh score was evaluated using Spearman correlation test.
Results
This cross-sectional study enrolled 54 liver cirrhosis patients, including 37 males and 17 females. Baseline characteristics of all patients are depicted in [Table/Fig-1]. Serologically, it proved that hepatitis B virus infection (53.7%) was the major infection followed by unknown causative agent (Non-B and C), 44.4%.
Baseline characteristics and demographic details of cirrhotic patients.
| Characteristics | Cirrhotic patients (n=54) |
|---|
| Gender (male/female) | 37/17 |
| Age (y) | 52.76±12.57* |
| Haemoglobin (g/dL) | 8.89±2.85* |
| Platelet count (x109/L) | 126.0 (26.0-582.0) |
| Serum Iron (μg/dL) | 30.0 (8.0-228.0) |
| Total Iron Binding Capacity/TIBC (μg/dL) | 175 (36-413) |
| Ferritin (ng/mL) | 398.35 (2.5-10133) |
| Prothrombin Time (secs) | 18.5 (12.6-45.4) |
| INR | 1.31 (0.81-2.96) |
| Total bilirubin (mg/dL) | 1.35 (0.29-29.8) |
| Urea (mg/dL) | 31.5 (6-268) |
| Creatinine (mg/dL) | 0.93 (0.52-13.58) |
| Albumin (g/dL) | 2.2 (1.5-3.7) |
| Child Turcotte Pugh (CTP) score | 9 (5-12) |
| Aetiology (positive) |
| HBsAg | 29 (53.7%) |
| Anti HCV | 1 (1.9%) |
| Non B and C | 24 (44.4%) |
Data is depicted in above table, as in column n consists of *mean±SD or median (interquartile range); INR: International normalised ratio; HBsAg: Hepatitis B surface antigen; Anti HCV: Anti Hepatitis C virus
NLR level were categorised into three groups: group A (NLR≤2.0), group B (2<NLR<5), and group C (≥5). Demographic data and laboratory findings are demonstrated in [Table/Fig-2], based on different value of NLR. There was no significant difference between laboratory results and NLR ratio, not with standing, several variables including age, albumin, creatinine, bilirubin and CTP score was higher in NLR ≥5 group patients. In addition, a significant correlation between NLR and CTP score was demonstrated in this study (r=0.326; p 0.008) using Spearman correlation test [Table/Fig-3].
Clinical and laboratory findings in cirrhotic patients included in the study.
| Variables | NLR ≤2 (n=5) | 2<NLR<5 (n=26) | NLR ≥5 (n=23) | p |
|---|
| Age (y) | 53.4±20.48 | 51.12±11.73 | 54.48±11.90 | 0.650 |
| Gender (Male/Female) | 4/1 | 17/9 | 16/7 | 0.804 |
| Albumin (g/dL) | 2.5 (1.6-3.3) | 2.15 (1.5-3.7) | 2.3 (1.5-3.4) | 0.972 |
| INR | 1.53 (1.3-1.84) | 1.29 (0.81-2.45) | 1.29 (1.04-2.96) | 0.211 |
| Creatinin (mg/dL) | 0.88 (0.6-0.94) | 0.86 (0.53-6.62) | 1.51 (0.52-13.58) | 0.058 |
| Total Bilirubin (mg/dL) | (0.7-2.4) | 1.36 (0.39-7.8) | 1.4 (0.29-29.8) | 0.675 |
| CTP score | 8 (7-9) | 8.5 (5-12) | 9 (7-12) | 0.144 |
Spearman correlation test result of correlation between NLR and CTP score among decompensated liver cirrhotic patients.
Discussion
This cross-sectional study was conducted to prove whether there was a significant correlation between NLR and CTP score, without describing the actual outcome or prognosis. Based on the study, it was observed that NLR had a significant correlation with Child-Turcotte Pugh score; thus the scoring system could be used as severity predictor among decompensated liver cirrhotic patients. It provides evidence that a patient with high NLR value tends to have higher CTP score. CTP score consists of five indicators which also relate to prognosis of liver cirrhotic patients [22,23].
NLR was found higher among decompensated patients compared to the compensated cirrhosis patients in a study conducted by He et al [24]. It is because that advanced or decompensated cirrhosis is proposed as an entity with complex association between systemic inflammation process and immune system [25]. In compensated cirrhosis, immune system will recognise ligands from damaged hepatocyte, mentioned as damage-associated molecular patterns (DAMPs) [26]. The result of the condition is sterile systemic inflammation. Meanwhile, in decompensated cirrhosis, ligands produced from bacterial translocation or bacterial component are shifted from the intestinal tract into circulation via static portal circulation and fragility of gut wall [27].
In general, high neutrophil levels could indicate on-going systemic inflammation while lymphocyte level positively correlated with endotoxin released by the pathogenic organism and cirrhotic severity [28-30]. NLR is ratio of neutrophil and lymphocyte, its levels are associated with certain conditions including autoimmune and other diseases [20,21], this also could be a limitation of NLR use in general population. Nevertheless, its applicability on daily clinical basis is certain since the time-saving and non-invasive interpretation could directly be made by clinician [31]. Other than that, the importance of identifying high NLR patients is to give new severity and mortality predictor. Kalra A et al., found NLR is associated with cirrhosis stage and liver-related death, similarly, decompensated liver cirrhotic patients had been used as the inclusion criteria by identifying lowest MELD within 90 days of the samples’ death [29]. Leithead JA et al., also suggested NLR as a new prognostic factor for prioritising liver transplant patient [32].
Based on the authors’ knowledge, the first correlation study of NLR and CTP score among cirrhotic patients in Indonesia was conducted by Probowati W et al., and it was found that NLR positively correlated with CTP score among 33 patients [33]. Biyik M et al., found that NLR is an independent predictor of mortality in Cox Regression models and significant correlation was obtained with CTP score (r=0.25; P=0.002) [13]. In other studies, NLR had a linear relationship with CTP score as the prognostic factors for Hepatocellular Carcinoma (HCC) in a different population with HCC [34]. In addition, Kwon JH et al., proved that high NLR was associated with one-month survival after admission among CTP class C patients independently [35]. The exact mechanism of NLR to explain its association with prognosis and correlation with CTP score remains elusive [11].
Limitation
The study did not escape limitation. The point-time approach measurement of several variables was performed. The induced susceptibility to certain confounding factor could affect NLR value, as the outcome and laboratory results were measured cross-sectionally.
Conclusion
Based on the study, it can be concluded that NLR and CTP score has a positive correlation. NLR could indicate some responses of systemic inflammatory response although the cytokine might have certain role in inflammatory condition (not measured in the study). While CTP score, as severity predictor, is independent of NLR and remains inconsistent in several studies. NLR threshold levels and its confounding condition must be determined in future studies including cohort studies, to identify high-NLR patient progress to decompensated stage. Therefore, high-NLR value could be used as predictor of mortality among decompensated liver cirrhotic patients, regardless of the CTP score.
Data is depicted in above table, as in column n consists of *mean±SD or median (interquartile range); INR: International normalised ratio; HBsAg: Hepatitis B surface antigen; Anti HCV: Anti Hepatitis C virus
[1]. Verhelst X, Geerts A, VanVlierberghe H, Cirrhosis: Reviewing the literature and future perspectivesEuropean Medical Journal Hepatology 2016 1:111-17. [Google Scholar]
[2]. Nishikawa H, Osaki Y, Liver cirrhosis: evaluation, nutritional status, and prognosisMediators of Inflammation 2015 2015:87215210.1155/2015/87215226494949 [Google Scholar] [CrossRef] [PubMed]
[3]. Elgouhari HM, Abu-Rajab TT, Carey WD, Hepatitis B virus infection: understanding its epidemiology, course, and diagnosisCleveland Clinic Journal of Medicine 2008 75(12):881-89.10.3949/ccjm.75a.0701919088007 [Google Scholar] [CrossRef] [PubMed]
[4]. Kwon YC, Ray RB, Ray R, Hepatitis C virus infection: establishment of chronicity and liver disease progressionEXCLI Journal 2014 13:977 [Google Scholar]
[5]. Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysisBMC Medicine 2014 12(1):14510.1186/s12916-014-0145-y25242656 [Google Scholar] [CrossRef] [PubMed]
[6]. Biselli M, Gitto S, Gramenzi A, Di Donato R, Brodosi L, Ravaioli M, Six score systems to evaluate candidates with advanced cirrhosis for orthotopic liver transplant: which is the winner?Liver Transplantation 2010 16(8):964-73.10.1002/lt.2209320677287 [Google Scholar] [CrossRef] [PubMed]
[7]. Zhao H, Gu X, Zhao R, Shi Y, Sheng J, Evaluation of prognostic scoring systems in liver cirrhosis patients with bloodstream infectionMedicine 2017 96(50):e884410.1097/MD.000000000000884429390273 [Google Scholar] [CrossRef] [PubMed]
[8]. Garcia-Tsao G, The Child-Turcotte Classification: from gestalt to sophisticated statistics and backDig Dis Sci 2016 61(11):3102-04.10.1007/s10620-016-4319-727696097 [Google Scholar] [CrossRef] [PubMed]
[9]. Peng Y, Qi X, Guo X, Child-Pugh versus MELD score for the assessment of prognosis in liver cirrhosis: a systematic review and meta-analysis of observational studiesMedicine 2016 95(8):e287710.1097/MD.000000000000287726937922 [Google Scholar] [CrossRef] [PubMed]
[10]. Aguiar MI, Braga VA, Almeida PC, Garcia JH, Lima CA, Severity of liver disease and quality of life in liver transplantationActaPaulista de Enfermagem 2016 29(1):107-14.10.1590/1982-0194201600015 [Google Scholar] [CrossRef]
[11]. Hong SH, Kim JE, Cho ML, Heo YJ, Choi JH, Choi JH, Comparison of the Child-Turcotte-Pugh classification and the model for end-stage liver disease score as predictors of the severity of the systemic inflammatory response in patients undergoing living-donor liver transplantationJournal of Korean Medical Science 2011 26(10):1333-38.10.3346/jkms.2011.26.10.133322022187 [Google Scholar] [CrossRef] [PubMed]
[12]. Durand F, Valla D, Assessment of the prognosis of cirrhosis: Child-Pugh versus MELDJournal of Hepatology 2005 42(1):S100-07.10.1016/j.jhep.2004.11.01515777564 [Google Scholar] [CrossRef] [PubMed]
[13]. Biyik M, Ucar R, Solak Y, Gungor G, Polat I, Gaipov A, Blood neutrophil-to-lymphocyte ratio independently predicts survival in patients with liver cirrhosisEuropean Journal of Gastroenterology & Hepatology 2013 25(4):435-41.10.1097/MEG.0b013e32835c2af323249602 [Google Scholar] [CrossRef] [PubMed]
[14]. Liu D, Huang Y, Li L, Song J, Zhang L, Li W, High neutrophil-to-lymphocyte ratios confer poor prognoses in patients with small cell lung cancerBMC Cancer 2017 17(1):882 [Google Scholar]
[15]. Chen S, Zhang L, Yan G, Cheng S, Fathy AH, Yan N, Neutrophil-to-lymphocyte ratio is a potential prognostic biomarker in patients with ovarian cancer: a meta-analysisBioMed Research International 2017 2017:794346710.1186/s12885-017-3893-129268698 [Google Scholar] [CrossRef] [PubMed]
[16]. Sato Y, Gonda K, Harada M, Tanisaka Y, Arai S, Mashimo Y, Increased neutrophil-to-lymphocyte ratio is a novel marker for nutrition, inflammation and chemotherapy outcome in patients with locally advanced and metastatic esophageal squamous cell carcinomaBiomedical Reports 2017 7(1):79-84.10.3892/br.2017.92428685065 [Google Scholar] [CrossRef] [PubMed]
[17]. Morriello F, Neutrophils and inflammation: unraveling a new connectionBiology and Medicine 2016 8(6):110.4172/0974-8369.1000325 [Google Scholar] [CrossRef]
[18]. Chen SS, Yu KK, Ling QX, Huang C, Li N, Zheng JM, Factors associated with significant liver necroinflammation in chronic hepatitis B patients with cirrhosisScientific Reports 2016 6:3309310.1038/srep3309327615602 [Google Scholar] [CrossRef] [PubMed]
[19]. Zhang H, Sun Q, Mao W, Fan J, Ye B, Neutrophil-to-lymphocyte ratio predicts early mortality in patients with HBV-related decompensated cirrhosisGastroenterology Research and Practice 2016 2016:439465010.1155/2016/439465026949385 [Google Scholar] [CrossRef] [PubMed]
[20]. Castro C, Gourley M, Diagnostic testing and interpretation of tests for autoimmunityJ Allergy ClinImmunol 2010 125(2 Suppl 2):238-47.10.1016/j.jaci.2009.09.04120061009 [Google Scholar] [CrossRef] [PubMed]
[21]. Riley LK, Rupert J, Evaluation of patients with leucocytosisAmerican Family Physician 2015 92(11):1004-11. [Google Scholar]
[22]. Tanoglu A, Karagoz E, Neutrophil-to-lymphocyte ratio: an emerging prognostic factor of cirrhosis?European Journal of Gastroenterology & Hepatology 2014 26(3):36210.1097/MEG.000000000000002124463541 [Google Scholar] [CrossRef] [PubMed]
[23]. Kim HJ, Lee HW, Important predictor of mortality in patients with end-stage liver diseaseClinical and Molecular Hepatology 2013 19(2):10510.3350/cmh.2013.19.2.10523837134 [Google Scholar] [CrossRef] [PubMed]
[24]. He Q, He Q, Deng Y, He Y, Xie L, Li T, Qin X, Li S, The relationship between inflammatory marker levels and HBV-related cirrhosis severityInt J Clin Exp Med 2016 9(11):22200-5.10.1155/2016/297847928090206 [Google Scholar] [CrossRef] [PubMed]
[25]. Arroyo V, Moreau R, Jalan R, Ginès P, Study EC, Acute-on-chronic liver failure: a new syndrome that will re-classify cirrhosisJournal of Hepatology 2015 62(1):S131-43.10.1016/j.jhep.2014.11.04525920082 [Google Scholar] [CrossRef] [PubMed]
[26]. Dirchwolf M, Ruf AE, Role of systemic inflammation in cirrhosis: From pathogenesis to prognosisWorld Journal of Hepatology 2015 7(16):197410.4254/wjh.v7.i16.197426261687 [Google Scholar] [CrossRef] [PubMed]
[27]. Martínez-Esparza M, Tristán-Manzano M, Ruiz-Alcaraz AJ, García-Peñarrubia P, Inflammatory status in human hepatic cirrhosisWorld Journal of Gastroenterology 2015 21(41):1152210.3748/wjg.v21.i41.1152226556984 [Google Scholar] [CrossRef] [PubMed]
[28]. Zubieta-Rodríguez R, Gómez-Correa J, Rodríguez-Amaya R, Ariza-Mejia KA, Toloza-Cuta NA, Hospital mortality in cirrhotic patients at a tertiary care centerRevista de Gastroenterología de México (English Edition) 2017 82(3):203-09.10.1016/j.rgmxen.2016.10.005 [Google Scholar] [CrossRef]
[29]. Kalra A, Wedd JP, Bambha KM, Gralla J, Golden-Mason L, Collins C, Neutrophil-to-lymphocyte ratio correlates with proinflammatory neutrophils and predicts death in low model for end-stage liver disease patients with cirrhosisLiver Transplantation 2017 23(2):155-65.10.1002/lt.2470228006875 [Google Scholar] [CrossRef] [PubMed]
[30]. Zhang J, Feng G, Zhao Y, Zhang J, Feng L, Yang J, Association between Lymphocyte-To-Monocyte Ratio (LMR) and the mortality of HBV-related liver cirrhosis: a retrospective cohort studyBMJ Open 2015 5(8):e00803310.1136/bmjopen-2015-00803326297362 [Google Scholar] [CrossRef] [PubMed]
[31]. Peng Y, Li Y, He Y, Wei Q, Xie Q, Zhang L, The role of neutrophil to lymphocyte ratio for the assessment of liver fibrosis and cirrhosis: a systematic reviewExpert Review of Gastroenterology & Hepatology 2018 12(5):503-13.10.1080/17474124.2018.146315829629626 [Google Scholar] [CrossRef] [PubMed]
[32]. Leithead JA, Rajoriya N, Gunson BK, Ferguson JW, Neutrophil-to-lymphocyte ratio predicts mortality in patients listed for liver transplantationLiver International 2015 35(2):502-09.10.1111/liv.1268825234369 [Google Scholar] [CrossRef] [PubMed]
[33]. Probowati W, Bayupurnama P, Ratnasari N, Correlation between neutrophil to lymphocyte ratio with child turcotte pugh in liver cirrhosis patientsActaInterna: The Journal of Internal Medicine 2016 6(1):28-35. [Google Scholar]
[34]. Oh BS, Jang JW, Kwon JH, You CR, Chung KW, Kay CS, Prognostic value of C-reactive protein and neutrophil-to-lymphocyte ratio in patients with hepatocellular carcinomaBMC Cancer 2013 13(1):7810.1186/1471-2407-13-7823409924 [Google Scholar] [CrossRef] [PubMed]
[35]. Kwon JH, Jang JW, Kim YW, Lee SW, Nam SW, Jaegal D, The usefulness of C-reactive protein and neutrophil-to-lymphocyte ratio for predicting the outcome in hospitalized patients with liver cirrhosisBMC Gastroenterology 2015 15(1):14610.1186/s12876-015-0378-z26498833 [Google Scholar] [CrossRef] [PubMed]