Cutaneous infections in man have become a public health problem affecting all age groups especially of tropical wet regions, where moisture plays an important role in growth of the fungi [1]. Millions of cutaneous fungal infections are observed in humans annually in which dermatophytosis ranks the first with about 10-20% of the population is affected by dermatophytes worldwide [2,3]. Epidermophyton, Microsporum and Trichophyton are the three main genera of dermatophytes that cause dermatophytosis. The different species of dermatophytes that are responsible for most human infections include Trichophyton rubrum, Trichophyton mentagrophytes, Trichophyton verrucosum, Trichophyton violaceum. Trichophyton tonsurans, Epidermophyton floccosum, Microsporumaudouinii, Microsporumcanis, Epidermophyton floccosum, Microsporumgypseum [4,5]. Dermatophytes due to its high affinity towards keratinized layers of skin, hair and nail causes superficial infections in both man and animals [6]. There has been a striking rise in the incidence of dermatophytes due to increase in number of immunocompromised patients and wide spread use of broad spectrum antibiotics [7,8]. Dermatophytes possess affinity for keratinized tissue, invade these tissues by keratinases, which produce dermal inflammatory response with burning, intense itching and redness which is mainly of cosmetic importance [6]. Dermatophytosis or Tinea infections caused by dermatophytes such as Epidermophyton, Microsporum and Trichophyton commonly called as ringworm is a progressing infection with an outer ring of active lesion and central healing. Dematopyhtic conditions ranges from mild to severe. The severity of infection also varies from chronic to high inflammatory lesions based on variety of factor such as site of infection, causative agent, etc., High prevalence rate of skin infection especially Tinea has been strongly linked to low socio-economic conditions [1,3,9]. Poor hygiene among low socio economic group, environment and climatic conditions plays a vital role in causing the infection. Early diagnosis and identification is the key for prevention and treatment of dermatophytosis among such population [10]. The prevalence of dermatophytosis also varies based on other factors such as type of population, individual’s susceptibility, life style and cultural practices. India being a sub-continent with varied topography situated in the tropical and sub-tropical regions supports the growth of especially dermatophytes. Studies have shown, there is vast difference in isolation of different species of dermatophytes from different parts of India and it varies based on the geographical pattern [11]. Although reports published so far unequivocally shows Trichophyton rubrum to be the most common dermatophyte isolated. Few reports have shown Trichophyton mentagrophytes and Trichophyton violaceum as the predominant dermatophyte. Puducherry has got hot and humid temperature exceeding 40°C-43°C [12]. This climatic condition favours dermatophytes. Moreover, the incidence and the infections caused by dermatophytes have also increased considerably [13]. Even though many works have been published on the incidence of dermatophytes from different parts of India there is not much data on these subjects residing in the coastal regions in and around Puducherry in the last two decades. Hence, the present study was undertaken to investigate the age and genderwise seasonal prevalence of dermatophytosis visiting the tertiary care hospital Puducherry.
Materials and Methods
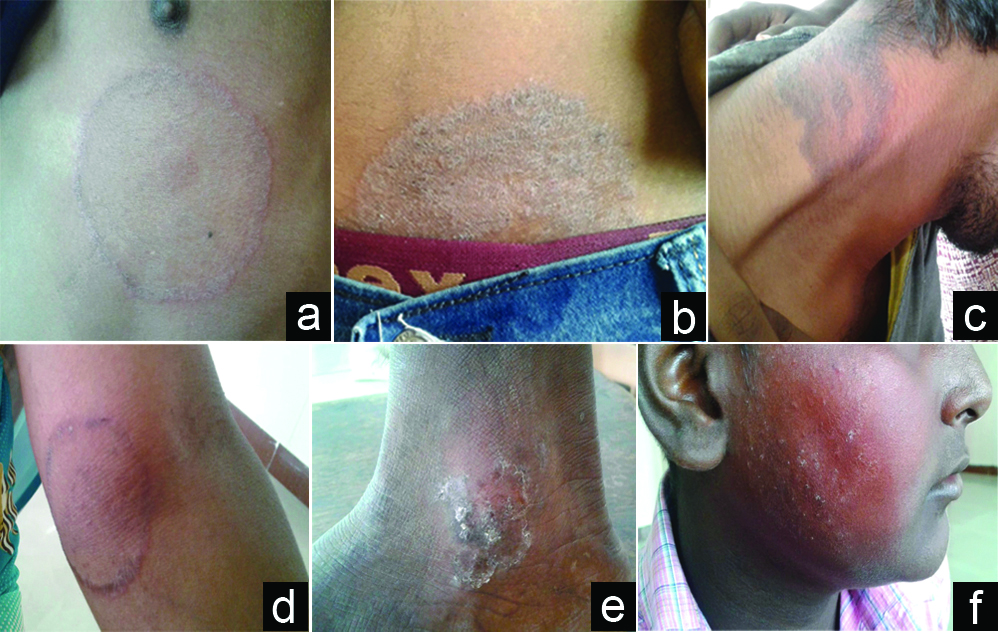
A cross sectional study conducted on patients who attended the Dermatology outpatient department of SLIMS, Puducherry over a period of one year extending from April 2015 to March 2016. A total of 356 patients presenting with skin infection (itchy and scaly skin rashes), nail infection (brittle and discolored nails) and hair infection (pruritic, bald patches/scaling areas with hair loss on the head) clinically suspected with dermatophytoses were included in the study [Table/Fig-1,2]. The duration of the symptoms were varied, nail infection was present since six months, skin and hair infection since three and one month respectively. Inclusion criteria: all skin, hair and nail samples of patients clinically suspected with dermatophytosis of both the sexes and of all age groups were included in this study. Exclusion criteria: Infants and those who were on any systemic or oral antifungal therapy or any tropical antifungal agent were excluded from this study. The dermatologist explained about the study and then informed consent was obtained from all the patients enrolled in this study. Institute ethical clearance (No.IEC/C-P/17/2015) for the study was obtained. A detailed clinical and medical history including age, sex, occupation, date of reporting, family history, drug history, type of lesion, site of lesion and clinical examination of affected site was recorded in all cases. The patients were categorised based on clinical material collected from different sites of infection as Tinea corporis (non-hairy skin), Tinea unguium (nails), Tinea cruris (groin), Tinea capitis (scalp and hair), Tinea pedis (feet), Tinea manuum (hand) and Tinea barbae (beard) [Table/Fig-3a-f]. The itchy scaly skin lesions, infected scalp, the brittle and discolored nails were cleaned with 70% ethyl alcohol, before clinical materials such as skin scrapings from the border of the lesion, infected hair, nail clippings and debris from under the edges of the infected nails were collected. A total of 82 nail specimens, 68 hair samples and 206 skin scrapings were collected from the different affected sites of all cases enrolled in this study. The collected materials was then dissolved in 10% KOH for the specimens such as skin scales and crust, while 40% KOH was employed for hair, nail specimens and examined for fungal elements [9,11]. The samples were cultured on Sabouraud’s dextrose agar slopes and dermatophyte test medium for selective isolation of dermatophytes. The culture tubes were incubated at 28°C for 4 weeks before labeling as negative. Dermatophytes were identified based on the colony morphology and microscopy by lactophenol cotton blue mount for the presence of vegetative hyphae, microconidia and macroconidia. Urease test was also done for species identification. Development of a deep red color through the medium was taken as a positive reaction given by Trichophyton mentagrophytes, Epidermophyton flocossum, Microsporumgypseum, Trichophyton violaceum, Trichophyton tonsurans [14-16].


a) Tinea corporis in chest; b) Tinea corporis in waist; c) Tinea corporis in neck; d) Tinea corporis in hand; e) Tinea pedis; f) Tinea faciei.
Results
This study includes 223 (62.6%) male patients and 133 (37.4%) female patients clinically suspected with dermatophytosis. It is evident from [Table/Fig-4], out of 82 (23%) nail specimens collected 23 (28%) were positive by culture and only 18 (22%) were positive by KOH/direct microscopy. Of the 68 (19.1%) hair samples collected, 18 (26.5%) showed positive culture and 7 (10.3%) were positive by direct microscopy. Among the 206 (57.9%) skin scrapings collected, 98 (47.6%) were culture positive whereas only 64 (31.06%) were positive by direct microscopy. [Table/Fig-5] reveals the genderwise distribution of various dermatophytosis. There was a high prevalence of dermatophytosis among males 223 (62.6%) with male to female ratio being 1.67:1. Similarly males predominated in all clinical types, except in Tinea unguium and Tinea manuum there was female preponderance 58 (70.7%), 9 (69.2%) compared to male patients 24 (29.3%), 4 (30.8%) respectively. The most common clinical type among males was Tinea corporis with 71/223 cases. Tinea capitis 53/223 was the second most common dermatophytic infection among males. Tinea unguium was the most common clinical type among female patients with 58/133 cases followed by Tinea corporis 36/133. Out of 356 patients maximum no. of dermatophytic cases was in the age group 21-30 years 98 (27.5%) and 31-40 years 82 (23.0%), followed by patients in the age group 41-50 years 71 (19.9%). The prevalence was low in two extremes of age; below 10 years with 33 (9.3%) cases and above 50 years with 27 (7.6%) cases. The youngest patient in this study was 1 year 6 months and the oldest patient was 64 years. In the present study, Tinea corporis was more common in the age group 21-30 years with 53 cases out of 107. Whereas, Tinea cruris 14/26 and Tinea pedis 5/10 was found to be more reported in the age group 11-20 years. In the age group 1 to 10 years Tinea capitis was common with 23/68 cases. Majority of cases affected with Tinea unguium 28/82 and Tinea barbae 18/42 was in the age group 41-50 years. Tinea mannum was found to be more reported in the age group 31-40 years with 8/13 cases [Table/Fig-6]. Out of 98 skin scrapings which were positive by culture, Trichophyton rubrum was the most common isolate 41/98. Other species of dermatophytes such as Trichophyton mentagrophytes, Trichophyton tonsurans, Microsporum gypseum, Epidermophyton floccosum, Trichophyton verrucosum and Trichophyton violaceum were also isolated, although in less numbers as represented in [Table/Fig-7]. Of 23 nail specimens positive by culture Trichophyton mentagrophytes was the major isolate 11/23 followed by Trichophyton tonsurans 7/23 and Trichophyton rubrum 5/23. Trichophyton mentagrophytes was the common dermatophyte isolated from hair specimens 14/18 followed by Microsporum gypseum 2/18, Trichophyton violaceum and Trichophyton rubrum 1 each [Table/Fig-7]. The overall prevalence of dermatophytosis in the present study was reported maximum during the months of April to June 127 (35.7%) cases followed by 81 (22.8%) cases during the pre-monsoon season from July to September. While during the winter season/colder months from October to December 76 (21.3%) cases were recorded and during the post-monsoon period from January to March 72 (20.2%) cases were encountered. In the summer months and the pre-monsoon period cases with Tinea corporis was recorded high 68/127 and 22/81 respectively. Whereas, in the colder months and in the post-monsoon period number of cases with Tinea unguium was encountered more 33/76 and 31/72 respectively [Table/Fig-8].
Distribution of dermatophytic cases based on clinical samples.
| Samples | Total number of cases | Number of culture positive cases | Number of cases positive by KOH |
|---|
| Nail | 82 (23.0%) | 23 (28%) | 18 (22%) |
| Hair | 68 (19.1%) | 18 (26.5%) | 7 (10.3%) |
| Skin | 206 (57.9%) | 98 (47.6%) | 64 (31.06%) |
| Total | 356 (100%) | 139 (39.0%) | 89 (25%) |
Genderwise distribution of dermatophytic cases.
| Sl. No | Clinical types | Total No. of cases | No. of Males (%) | No. of Females (%) |
|---|
| 1 | Tinea corporis | 107 | 71 (66.4%) | 36 (33.6%) |
| 2 | Tinea unguium | 82 | 24 (29.3%) | 58 (70.7%) |
| 3 | Tinea cruris | 26 | 15 (57.7%) | 11 (42.3%) |
| 4 | Tinea capitis | 68 | 53 (77.9%) | 15 (22.1%) |
| 5 | Tinea pedis | 10 | 7 (70%) | 3 (30%) |
| 6 | Tinea manuum | 13 | 4 (30.8%) | 9 (69.2%) |
| 7 | Tinea barbae | 42 | 42 (100%) | 0 (0%) |
| 8 | Tinea faciei | 8 | 7 (87.5%) | 1 (12.5%) |
| Total | 356 | 223 (62.6%) | 133 (37.3%) |
Male: Female=1.67:1
Agewise distribution of various clinical types.
| Clinical types | No. of cases | Age in years |
|---|
| 1-10 | 11-20 | 21-30 | 31-40 | 41-50 | ≥51 |
|---|
| Tinea corporis | 107 | 3 | 12 | 53 | 28 | 6 | 5 |
| Tinea unguium | 82 | 1 | 3 | 18 | 24 | 28 | 8 |
| Tinea cruris | 26 | 0 | 14 | 9 | 3 | 0 | 0 |
| Tinea capitis | 68 | 23 | 11 | 8 | 6 | 15 | 5 |
| Tinea pedis | 10 | 3 | 5 | 1 | 0 | 1 | 0 |
| Tinea manuum | 13 | 0 | 0 | 0 | 8 | 3 | 2 |
| Tinea barbae | 42 | 0 | 0 | 8 | 12 | 18 | 4 |
| Tinea faciei | 8 | 03 | 0 | 1 | 1 | 0 | 3 |
| Total (%) | 356 (100%) | 33 (9.3%) | 45 (12.7%) | 98 (27.5%) | 82 (23.0%) | 71 (19.9%) | 27 (7.6%) |
Correlation of clinical samples and dermatophyte SPP.
| Organism Isolated | Type of Specimen | Total No. of Isolates |
|---|
| Skin | Nail | Hair |
|---|
| Trichophyton rubrum | 41 | 5 | 1 | 47 |
| Trichophyton mentagrophytes | 35 | 11 | 14 | 60 |
| Epidermophyton floccosum | 3 | 0 | 0 | 3 |
| Trichophyton verrucosum | 3 | 0 | 0 | 3 |
| Trichophyton tonsurans | 8 | 7 | 0 | 15 |
| Trichophyton violaceum | 3 | 0 | 1 | 4 |
| Microsporum gypseum | 5 | 0 | 2 | 7 |
| Total | 98 | 23 | 18 | 139 |
Seasonal distribution of dermatophytic cases.
| Clinical types | Total No. of cases | No. of cases from Jan-Mar (Post monsoon) | No. of cases from April-June (Summer) | No. of cases from July-Sep (Premonsoon) | No. of cases from Oct to Dec (Winter) |
|---|
| Tinea corporis | 107 | 12 | 68 | 22 | 5 |
| Tinea unguium | 82 | 31 | 7 | 11 | 33 |
| Tinea cruris | 26 | 2 | 15 | 8 | 1 |
| Tinea capitis | 68 | 16 | 11 | 18 | 23 |
| Tinea pedis | 10 | 1 | 4 | 2 | 3 |
| Tinea manuum | 13 | 4 | 1 | 1 | 7 |
| Tinea barbae | 42 | 4 | 21 | 17 | 0 |
| Tinea faciei | 8 | 2 | 0 | 2 | 4 |
| Total | 356 | 72 (20.2%) | 127 (35.7%) | 81 (22.8%) | 76 (21.3%) |
By Fisher’s-exact test p-value<0.001
Discussion
Mycotic infections are worldwide in distribution, with superficial mycoses being more prevalent in the tropical and subtropical countries, including India, where heat and moisture play an important role in promoting the growth of these organisms. Superficial skin infections caused by dermatophytes resulting in local inflammation are common in humans. In recent years, there is a worldwide increase in people getting affected by these Tinea infections [11]. The present work was conducted to determine the most common clinical presentation along with the causative agent and to compare the outcome of microscopic evidence and culture findings of clinical specimens used in the study. Attempts were made to assess the age and genderwise seasonal distribution of dermatophytoses in Puducherry, India. In the present study, skin infections were found to be the commonest clinical presentation (57.9%) followed by nail infection (23.0%) and hair infection (19.1%). Similar observation has been made by Patel P et al., and Kannan et al., in their study who reported dermatophytic skin infection to be more common compared to dermatophytic nail and hair infections [17,18]. The high prevalence of skin infection is probably due to severe itching associated with it inducing the patient to seek early medical advice as well as environmental conditions such as hot and humid weather characteristic of this study area and their nature of clothing which adds to increase in warmth of the skin, providing a suitable area for dermatophytes to grow on skin [19,20]. In this study identification/demonstration of dermatophytes and was comparatively better viewed by culture than by direct Microscopy using KOH preparation from all the three types of specimens and it was also found that mycological evidence of dermatophytes was low for hair specimens. However this finding was in contrast to studies conducted by Patel P et al., Patel KD et al., and Singh S et al., who reported in their studies that direct examination by microscopy was highly efficient screening technique and identification rate was also better than culture [17,21,22].
No race in any geographical location is totally free of dermatophytoses. Although, it is universal, the distribution of this group of fungal infections varies depending upon the environment, the host, the agent. In addition the geographic location, temperature, humidity, factors like age, gender, local customs and traditions also play a major role in determining the incidence and prevalence of the disease [11]. A high prevalence of dermatophytoses in males (62.6%) was reported than in females (37.3%) with male to female ratio being 1.67:1. This finding has been endorsed by various studies in India and abroad [23-26] owing to physical outdoor labor, their nature of work and frequent interactions with different people of society [27,28]. Correlating gender variability with the clinical type of dermatophytosis, in the present study, a male dominance was seen with all clinical types, except with Tinea manuum and Tinea unguium where the gender ratio was reversed showing female preponderance. Similar finding has been reported in studies conducted by authors [19,29]. Male preference was observed in Tinea cruris, Tinea corporis, Tinea capitis, Tinea pedis, Tinea barbae and Tinea faciei which correlates with greater physical activity, their occupations and strenuous work. Prolonged hours under the scorching heat predispose them to certain dermatophyte infections. Females are more involved in household activities and their frequent exposure to moist conditions might be the reason for increased Tinea unguium and Tinea manuum in this gender [20,30].
Dermatophyte infection is most common in the 3rd and 4th decade of life, as has been reported by several studies in India [17,31], this finding has been upheld in the present study accounting for 27.5% cases and 23.0% cases respectively. In the present study, it was found almost all ages were susceptible to various dermatophytic infections with preference in age to certain type of dermatophytosis. Kanwar AJ et al., in his study also stated a wider range of age during which dermatophyte infection is prevalent i.e., 16-45 years [23]. Tinea corporis was the most common clinical pattern among 21-30 years and 31-40 years in this region. As declared by several authors the increased prevalence in this age group could be connected to strenuous outdoor manual work with excessive perspiration in this age group compared to torpid behavior in the later years [9,17]. Whereas, in 11-20 years Tinea cruris was found common and in 1-10 years of schoolgoing age, Tinea capitis was common. This finding has been accepted universally that Tinea capitis, an infection preferably found in children. Tinea unguium was found to be common among 41 to 50 years and above 51 years of age.
In this study, the predominant dermatophyte isolated was Trichophyton mentagrophytes and it was 60/139. The most common dermatophyte isolated from skin scrapings was Trichophyton rubrum followed by Trichophyton mentagrophytes. This is in accordance with study carried out by authors in which Trichophyton rubrum is the chief isolate from skin scales [18,26,32,33]. In this study it was found that skin infection was caused by all species of dermatophytes of all three genera. This finding is in accordance with that observed by authors [9,17,27]. Other species of dermatophytes such as Epidermophyton floccosum, Trichophyton verrucosum and Trichophyton violaceum were also isolated although in small numbers whereas most common dermatophytes isolated from hair and nail samples were Trichophyton mentagrophytes. Similar results were observed by others, the authors opined that Trichophyton rubrum and Trichophyton mentagrophytes are the common species infecting the nails [16,33]. Microsporum nail infections are rare [34], this finding has been upheld in the present study. However, Microsporum audouinii was isolated in a study by Adhikari L et al., in Sikkim [35].
Dermatophytosis was reported throughout the year and in all seasons in this locality but still the overall prevalence was maximum 35.7% during the months of April to June and least 20.2% during the months of January to March. Puducherry experiences hot and humid climate throughout the year which provides a fertile ground for the abundant growth of dermatophytes. Jain N et al., in their study on dermatophytoses in Jaipur opined that their summers are hot and dry while the monsoons are associated with high humidity. These climatic conditions favour the occurrence of fungal infections [28]. Sen SS et al., was of the opinion that Assam receives heavy rainfall during the monsoon months and the humidity remains high almost throughout the year [36]. This high humidity thus makes the skin a conducive site for growth of dermatophytes and hence increased prevalence. Tinea corporis cases were recorded high during the summer and pre-monsoon season i.e., from April to September, whereas the colder months from October to December and the post-monsoon season cases with Tinea unguium were recorded more. From the present study it is evident that dermatophytosis pose a significant health problem in this locality due to its hot and humid climate for a major part of the year. Hence, there is need for frequent monitoring and to create awareness regarding the adequate preventive measures in this locality.
Limitation
In the present study, predisposing factors contributing to dermatophytosis such as lack of hygiene, poor nutrition, lower socioeconomic standard, their occupation, living conditions were not presented in the present manuscript due to space constraint. This study also recommends future studies involving areawise studies for a longer duration in order to get a clearer picture of seasonal prevalence in this region.
Conclusion
The commonest clinical presentation in this study was patients having skin infection frequently caused by Trichophyton rubrum compared to other dermatophytosis and Trichophyton mentagrophytes being the most common isolate from hair and nail specimens. Mycological diagnosis/evidence of dermatophytes in hair was low. Male preponderance was seen in most clinical types except in Tinea manuum and Tinea unguium, where the gender ratio was reversed, female preponderance was seen. Almost all ages were found susceptible to dermatophytosis with maximum number of patients in the 3rd decade of life and variation in the type of dermatophytosis according to age was noted. Dermatophytosis has been reported throughout the year in this locality chosen for studying and an increase in prevalence of certain clinical types in specific seasons was found. Hence, it’s essential to educate precautionary measures to curtail the prevalence of dermatophytosis among the population at risk in this locality.
Male: Female=1.67:1
By Fisher’s-exact test p-value<0.001