Heart and great vessel structural abnormalities are the most common and severe form of congenital anomalies [1]. Congenital heart defects are accompanied with high morbidity and mortality in the neonatal period. This causes an economic and emotional burden on families and health system [2]. Moreover, the majority of Congenital Heart Diseases (CHDs) go unnoticed in the prenatal screening as the routine foetal ultrasounds are not targeted at screening of foetal heart for CHDs [1]. The prevalence of CHD and great vessel structural defects has been estimated at 3-8/1000 live births [1]. Only 10% of pregnant women with identifiable risk factors have evidence of foetal CHD, like presence of extracardiac malformations [3]. Although in the last few decades the foetal detection rate of CHD has significantly developed [4,5], the detection rate in low-risk pregnant women does not outstrip 35-40% [3].
However, major foetal cardiac malformations can be diagnosed by echocardiographic four-chamber view only [6]. Furthermore, if cardiac screening is achieved by a detailed echocardiographic examination the detection rate is nearly 100% [7]. Most of the neonatal heart diseases detected in families with no risk factors for CHD [7]. So, screening of the whole population is crucial if proper foetal detection of CHD is required [7]. Moreover, early recognition of foetal heart diseases will ensure ideal neonatal and surgical care if needed [3] which in turn will decrease the rate of neonatal mortality and morbidity [8].
The aim of the study was to estimate the efficiency of the screening program for the detection of foetal CHD in an unselected population of women and to identify the frequency and type of foetal CHD using foetal echocardiography.
Materials and Methods
This cross-sectional observational study was carried out in the echocardiography unit of Baghdad Teaching Hospital, Iraq over a period of 26 months from April 2016 to June 2018. All women aged between 18 and 45 year that underwent foetal echocardiography during the study period were included with a gestational age ranging from 20 to 40 weeks. Additionally, pregnant women who did not consent for the study were excluded. Moreover, they were categorised as high, low and no risk groups according to the indication for referral for foetal echocardiography which is released from the American Heart Association for the Diagnosis and management of Foetal Cardiac Diseases [9]. Approval was taken from the ethical committee of the University of Baghdad/College of Medicine (registration no. 15) and an informed consent was taken from the patients that registered in the study.
All foetal echocardiography was done by a single researcher and demographic data was collected from all the women through direct interview in addition to reviewing the recorded files of gynecological department if needed. A 2D and Doppler foetal echocardiography examination was done according to guidelines of International Society of Ultrasound in Obstetrics and Gynecology (ISUOG). Foetal echocardiography was accomplished by a trans-abdominal route using ‘vivid E9’ machine with 2-5 MHz convex probe.
Two-dimensional echocardiography was performed for all cases. However standard four chambers, five chambers, short axis and oblique views were taken, in addition to M-mode and Doppler echo including continuous wave Doppler, pulsed-wave Doppler and color flow mapping).
Furthermore, after delivery neonatal follow-up was carried out for selected cases based on the results of foetal echocardiography. Postnatal echocardiography was performed by using vivid E9 machine with a 12 MHz convex probe. Images and videos of all foetal abnormalities were recorded and saved in a digital media.
The data was presented in numbers and percentage.
Results
A total of 263 foetal echocardiographies were performed for pregnant women during a period of 26 months.
The gestational age at the time of referral ranged from 20 to 40 weeks, where 236 pregnant women underwent foetal echocardiography examination at a gestational age of ≥36 weeks and 27 pregnant women did the examination at a gestational age between 20 and 36 weeks.
However, out of 263 pregnant women 22 foetal cardiac abnormalities were presented in 14 foetal hearts as shown in [Table/Fig-1], as some fetuses presented with single cardiac anomaly while others had multiple anomalies.
Frequency of foetal cardiac abnormalities detected prenatally.
| Cardiac abnormality | Number (Total=263) | Frequency (%) | CHD in foetus with |
|---|
| High risk | Low risk | No risk |
|---|
| Hypoplastic Right Side Syndrome | 1 | 0.38 | 0 | 0 | 1 |
| Complete AV Canal | 2 | 0.76 | 2 | 0 | 0 |
| Aortic Stenosis | 1 | 0.38 | 1 | 0 | 0 |
| Tricuspid Valve Dysplasia | 1 | 0.38 | 0 | 0 | 1 |
| Ventricular Septal Defect | 3 | 1.14 | 1 | 0 | 2 |
| Atrial Septal Defect | 2 | 0.76 | 2 | 0 | 0 |
| Tricuspid Regurgitation | 3 | 1.14 | 2 | 0 | 1 |
| Pericardial Effusion | 1 | 0.38 | 1 | 0 | 0 |
| Hydrops Foetalis | 3 | 1.14 | 3 | 0 | 0 |
| Tachyarrhythmia (SVT) | 1 | 0.38 | 1 | 0 | 0 |
| Bradyarrhythmia | 3 | 1.14 | 3 | 0 | 0 |
| Left Ventricular Hypertrophy | 1 | 0.38 | 1 | 0 | 0 |
| Total | 22 | 8.36 | 17 | 0 | 5 |
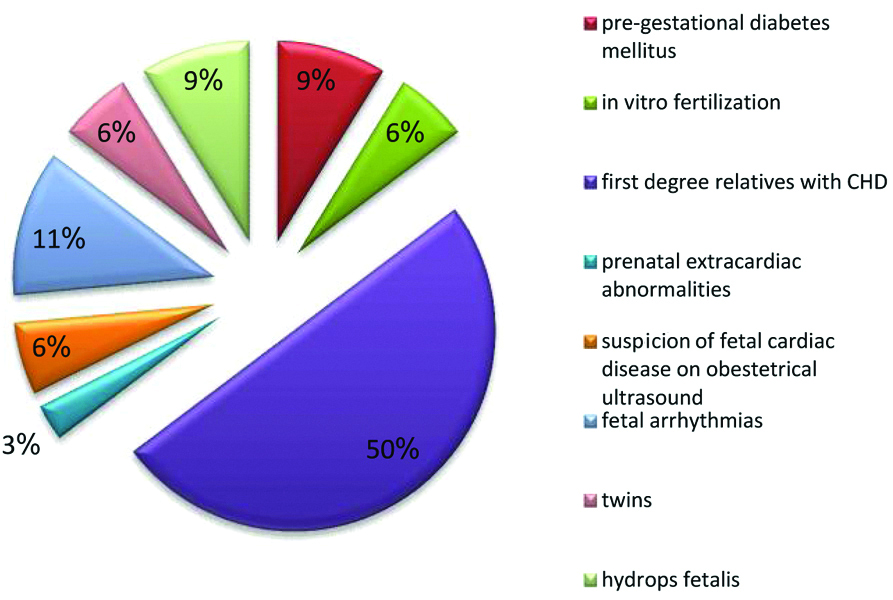
Seventeen out of 22 cases were classified as high risk group with 50% of them having family history of CHD [Table/Fig-2], where as, 5 were classified as no risk group. On the other hand, no women were categorised as low risk group in this study.
The described risk factors in high risk pregnant women.
This study showed that the incidence of foetal heart disease prenatally is 5.3%. Regarding 14 fetuses with cardiac anomalies, nine (3.4%) of them presented in high risk pregnant women, whereas the rest five (1.9%) cases were found in non-risk women. For example; among high risk pregnant women, three cases were diagnosed in this study as follows: the first case showed abnormal gynecological ultrasounds and was diagnosed as complete AV canal, the second case had a conjoined twin and diagnosed as single heart with complete AV canal, and the third case had fetus with bradycardia and was diagnosed as aortic stenosis.
Furthermore, 8 (3.04%) fetuses out of 14 cases were categorised with simple cardiac abnormality and 6 (2.2%) fetuses with complex cardiac disease as shown in [Table/Fig-3].
Cardiac disease detected in fetuses categorized as simple and complex cardiac abnormality.
| Fetuses With Simple CHD | No. | High/Low/No Risk Women | Fetuses With Complex CHD | No. | High/Low/No Risk Women |
|---|
| Single VSD | 1 | No Risk | Hypoplastic right side syndrome, TV dysplasia with tricuspid regurgitation and inlet VSD | 1 | No Risk |
| Single ASD | 2 | High Risk | Moderate aortic stenosis, VSD and bradycardia | 1 | High Risk |
| Bradycardia with normal cardiac structure | 2 | High Risk | Hydrops foetalis with supraventricular tachycardia | 1 | High Risk |
| Left ventricular hypertrophy | 1 | No Risk | Hydrops foetalis | 1 | High Risk |
| Tricuspid regurgitation | 2 | High Risk | - Complete AV canal with hydrops foetalis.- Complete AV canal in conjoined twin. | 2 | High Risk |
| Percentage | 3.04% | | Percentage | 2.2% | |
Only 10 fetuses which had CHDs were followed up postnatally as shown in [Table/Fig-4]. Some of the fetuses were lost to follow-up, whereas few died as shown in the [Table/Fig-4]. Complete agreement of 80% was seen between pre and post natal findings.
Foetal outcomes post-delivery.
| Case No. | Type of Prenatal CHD | Postnatal Outcomes |
|---|
| 1 | Hypoplastic right side syndrome | Neonatal death |
| 2 | Complete AV canal in conjoined twin | Missed follow-up |
| 3 | Aortic stenosis with bradycardia | Missed follow-up |
| 4 | Ventricular septal defect | Missed follow-up |
| 5 | Atrial Septal Defect (ASD) | Neonates with small ASD secundum |
| 6 | Atrial Septal Defect | Neonates with small ASD secundum |
| 7 | Tricuspid Regurgitation (TR) | Neonate with PFO and no TR |
| 8 | Tricuspid Regurgitation | Missed follow-up |
| 9 | Hydrops foetalis with tachyarrythmia | Neonate with small ASD secundum |
| 10 | Hydrops foetalis with complete AV canal | Neonate with dysmorphic features and complete AV canal |
| 11 | Hydrops foetalis | Neonatal death |
| 12 | Bradyarrythmias | Neonatal death |
| 13 | Bradyarrythmias | Intra Uterine Death |
| 14 | Left Ventricular Hypertrophy (LVH) | Neonate with LVH, small ASD secundum and bicuspid AV |
Discussion
CHDs are considered as one of the most common aspects of foetal congenital anomalies diagnosed in humans [8]. Based on the WHO studies, cardiac anomalies comprise 42% of infant deaths and have been considered as the leading cause of mortality in infants [10]. Additionally, the early recognition of CHDs in foetal period based on foetal echocardiography examination is of vital importance for management of these cases [8]. In the same way, the early diagnosis shows a significant improvement in the pregnancy outcome for the fetuses who are diagnosed with particular types of cardiac anomalies [11]. The prenatal ultrasounds, which are routinely carried out over pregnancy period, do not investigate CHDs, and this leads to majority of CHDs not being discovered during the foetal life [1].
Regarding the referral indications, it is worth to mention that 50% of the cases were referred for foetal echocardiography examination because of the family history of congenital heart defects, and those cases were considered as most common referral cause in high-risk group of this study. This result is similar to that found in Iftikhar M et al., who also pointed out that the common causes for foetal echocardiography referral in high risk group were a family history of CHDs was found [2]. In contrast, other studies disagreed with the finding of the current study, for instance, Rocha LA et al., Clur SAB et al., and Ozkutlu S et al., stated that the higher referral indication for foetal echocardiography were maternal metabolic diseases, increased nuchal translucency, extra-cardiac defects, and the history of intrauterine foetal death [12-14]. Additionally, further studies have emphasised on the main reason for referral indication of foetal echocardiography which is the abnormality of foetal ultrasound [15-17].
Rychik J et al., stated that the ideal period for performing a comprehensive foetal echocardiography examination is 18-22 weeks gestation [18]. A total of 236 out of 263 pregnant women underwent foetal echocardiography at a gestational age >36 weeks. This was in discordance to various studies, where the range was between 25 and 27 weeks of gestation [15,17,19,20] due to different time periods of referral indications.
Rocha LA et al., found that the incidence of complex cases is greater than the simple cases [12]. On the other hand, the finding of this study stated that the incidence of the simple foetal cardiac disease is about 3.04%, which is greater than the complex foetal cardiac disease by 0.84%, and this may be due to the involvement of both high and non-risk pregnant women, where as Rocha LA et al., dealt with only high risk pregnant women [12]. Moreover, the incidence for presenting a foetal heart disease in this study is 5.3%, which is close to those concluded by Iftikhar M et al., and Bakiler AR et al., of 6% and 5%, respectively [2,21]. However, Rocha LA et al., yielded that the prevalence percentage is about 9.96% and this is due to the reason that they involved only high risk pregnant women [12].
Additionally, this study concluded an agreement of 80% between prenatal and postnatal diagnosis of CHD, where as Sharma S et al., found an agreement of 68.17% between prenatal and postnatal findings and this is due to inclusion of larger sample of 1200 pregnant women in their study [1].
Finally, the results of this study showed that in comparison with high risk group, the no risk pregnant women yield great advantages from screening of foetal CHDs. This results correlated to Zhang YF et al., results [22].
Limitation
The prenatal CHD echocardiography screening results should not depend on single medical center or ultrasound modality and large multi-center studies are of vital importance.
Conclusion
The present study demonstrates that there is an increased incidence of CHDs within high risk pregnancies and no risk pregnancies compared to low risk. Furthermore, this study shows a high accurateness of prenatal echocardiography in identification of CHDs. So, we endorse foetal echocardiography to be categorised as a part of antenatal screening program for all pregnant women referred for antenatal follow-up irrespective of their referral cause.