Preterm birth is the most common cause of antenatal mortality and morbidity in the world. The data of scientific researches prove that the rate of preterm birth ranges between 5-20% out of the overall birth rates. It can be proved by the statistical data of the USA where 7.5% [1,2] of the birth rate belong to preterm birth. According to the WHO, about 1500 000 premature births occur annually in the world. Within the above data 15 million preterm births occur in Africa, Asia and Latin America, the lowest rate of preterm delivery occur in Europe-6.2% [3,4], and about 6.4% in Kazakhstan [3]. Majority of children, who were born before biologically normal term, suffers from long term unfavourable consequences of the preterm births. The most frequent outcomes are: motor system disorders such as lifelong disability; cognitive, sensor, and behavioural issues; visual/auditory apparatus problems including educational difficulties; additionally, socio-emotional problems [4-6].
It is possible to overwhelm the growth of the preterm birth rate by a broad implementation of modern reproductive technologies (multiple gestations) and the possibilities of modern gynaecology; by the birth term management for women with severe somatic diseases [7]. In spite of the recent achievements in medicine, technology rise and pharmacologic possibilities around the world, the preterm birth rate does not seem to decrease. A broad number of examinations and surveys in the fields of the diagnostic methods, effectiveness, treatment and prevention of the preterm birth is an important factor in determining the scale of current issue. The short cervix has been identified as a significant predictor of preterm birth. A number of biochemical and biophysical markers were proposed to determine the high risk of spontaneous preterm delivery. Now-a-days it is proved that cervical examination using ultrasound is more effective than vaginal manual examination. Besides, it also can help to identify patients at risk of preterm delivery until 34 weeks of gestation [8-12].
The risk of preterm birth is low in patients with a cervical length >30 mm and, therefore, it can help to avoid aggressive intervention of health care professionals. In contrast, patients with cervical shortening (25 mm or less) have a higher risk of preterm birth. In such cases, interventions of health care workers are necessary and justified (e.g., management of the short cervix, introduction of steroid drugs along with tocolytic therapy, transportation to specialised medical institutions). The risk of preterm birth is inversely proportional to the length of the cervix, the shorter the cervix, the higher the risk of premature birth and vice versa. Transvaginal cervicometry is an effective method for assessing the risk of preterm birth in asymptomatic patients at high risk of preterm delivery [6,12-17].
Different methods of the short cervix management have been studied within the recent 10 years: non-surgical and surgical. One of the non-surgical methods demands the usage of an obstetric pessary with and without vaginal progesterone. The Arabin obstetric pessary is cone-shaped and made of silicone. It has been claimed that obstetric pessary decreases the internal pressure by changing the angle of cervix canal inclination. That redirects the weight of the uterus and results in prevention of the preterm cervical dilatation and rupture of membranes. Additionally, there is an evidence that obstetric pessary is the immunologic barrier between the chorion and vagina which consequently contributes in the pregnancy prolongation [18].
Cervical cerclage is considered to be one of the well-studied surgical methods for the short cervix management. In the literature there are a lot of controversy about the optimal technique, timing of application and suture materials used for cervical cerclage [19-21].
Endogenous progesterone method is also necessary for maintenance and prolongation of pregnancy. Regarding the way of progesterone application, it should be noted that each method of managing has its advantages and disadvantages. Hence, the concentration of progesterone in blood plasma is three times higher in vaginal application than in oral intake, which is explained by the good absorption of the drug in the vaginal mucosa and the absence of the effect of the first passage through the liver. Also, the vaginal forms of taking progesterone are well tolerated and have fewer side effects. The disadvantages of vaginal administration include: discomfort, irritation and burning feeling after application, as well as inconvenience of managing during vaginal bleeding.
Materials and Methods
In total, 1806 women were examined (National Research Center for Maternal and Child Health; Astana Medical University, Department of Obstetrics and Gynecology), 125 women (6,9%) agreed to participate in the research and met the inclusion criteria. This was a prospective open-label non-randomised clinical trial with inclusion of 125 women. These women experienced a preterm birth history and had shortened cervix, determined by transvaginal ultrasound diagnosis in the current pregnancy.
Thus, after obtaining informed consent for participation in the study, three groups were formed out of 125 subjects, depending on the short cervix management methods: surgical and non-surgical.
Group I-Obstetric pessary of Dr. Arabin was used as a non-surgical method, the obstetric pessary sizes were selected in accordance with the table of instructions (62 subjects).
Group II-The Lyubimova and Mammadaliyeva method of management by cerclage with non-absorbent suture material was applied as a surgical treatment (31 subjects).
Group III-Progesterone with vaginal access at a dose of 200 mg/day was used as an alternative non-surgical method (32 subjects).
Prior to the intervention, the Ethicas Committee approval has been received.
The participants were chosen according to the following inclusion criteria: singleton pregnancy; preterm birth or presence of loss of pregnancy in the second trimester concerning the patient’s history (more than 16 weeks or less than 37 weeks of gestation); shortening of the cervix-length less than 25 mm (according to the results of transvaginal ultrasound based cervicometry).
The women with the following pathologies were excluded from the study: vaginal bleeding with unknown aetiology; suspicion of preterm prenatal rupture of membranes or the beginning of regular labour; abdominal pain which is not associated with preterm birth; chromosomal/structural abnormality of the foetus; severe extra genital pathology; malignant tumour with various localisation; presence of any contraindications to the used cervix management methods (allergic reaction, thromboembolic complications).
The participants have been informed about the management methods of the short cervix. As soon as the diagnosis had been established and informed consent had been received, the management of the cervix was performed. The ultrasound cervicometry follow-up was conducted according to the clinical situation and the indications.
The process was performed according to generally accepted standards in the IBM SPSS program 21. Quantitative variables were checked for the relevance of the distribution using descriptive statistics (kurtosis and asymmetry less than | 1 |), Shapiro-Wilk criteria (age, gestational age, cervical length). Quantitative variables with normal distribution were tested by the arithmetic mean, variance, standard error and 95% confidence interval while quantitative data calculated by 25% median and 75% quartile that not subject to the normal distribution law.
For categorical variables (rank), the frequency of occurrence, variance, standard error and 95% confidence intervals (term birth) were calculated.
The reliability between the quantitative indicators was estimated by the Student’s test for independent groups, the reliability of the revealed differences in categorical variables was estimated using the Fisher’s z-criterion, the significance level of the difference was p ≤0.05.
To apply the Student’s t-test, it is necessary that the initial data have a normal distribution. In case of applying a two-sample criterion for independent samples, it is also necessary to observe the condition of equality (homoscedasticity) of variances.
To compare the average values, the t-test of the Student is calculated by the following formula:
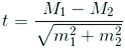
Where, M1 is the arithmetic mean of the first compared population (group), M2 is the arithmetic average of the second compared population (group), m1 is the average error of the first arithmetic mean, m2 is the mean error of the second arithmetic mean.
The Z-test (Fisher’s z-criterion) is usually used to test the equality of mean values for a known population variance or for estimating the sample mean of standardised values. Z-statistics is calculated as the ratio of the difference between the random variable and the mathematical expectation to the Standard Error (SE) of this random variable:
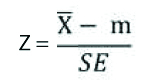
where, the random value of the sample mean, is the value of the mathematical expectation, which is the SE of this value.
Results
Median age of the participants in the group of obstetric pessary was Me-30.8, in the cerclage group Me-32.2, and in the progesterone group Me-31.5 years.
Comparing groups I and II by the age category, no significant differences were found. Comparison of groups I and III according to age groups showed significant differences between groups {CI (95%) 2-4.2} and a direct relationship between the onset of preterm delivery in the subjects (p<0.05) over 40-years-old. When comparing groups II and III, significant differences were found between the groups (CI (95%) 19.5-24.6) and the direct relationship between the onset of preterm delivery in the subjects (p<0.05) aged 31 to 34 years in the study groups.
Next, we compared the gestational age and the length of the cervix at treatment entry in the three groups. The mean gestational age at treatment entry in the obstetric pessary group was 21.7 weeks, while in the cerclage group it was 15.9 weeks, and in the progesterone group 21.4 weeks.
Comparison of the cervix length did not show statistically significant differences. The mean cervical length in the obstetric pessary group was 23.6 mm, while in the cerclage group it was 23.6 mm, and in the progesterone group 24.4 mm.
In group I (n=62), 100% of uterus short cervix management subjects were treated with obstetric pessary, without additional use of vaginal progesterone.
In group II (n=31), all subjects were stitched by Lyubimova and Mammadaliyeva seam with non-absorbent suture material as a surgical treatment, additional tocolytic therapy was performed in the hospital during post-operative period for 1-2 days.
In group III (n=32), vaginal progesterone was used by all pregnant women. In this group, because of shortening the cervix length for 15 mm an obstetric pessary was applied additional for 11 (34%) pregnant women.
The results of comparison show that in the group II the gestational age is significantly less than in the group I (p<0.05). The length of the cervix in the study groups did not have statistically significant differences. Between group I and III there were no significant differences. A comparison was made between group II and group III, in which the gestational age of cervical contraction in the group II was significantly less than in group III (p<0.05). Thus, in the II group, the gestational age of detection of the short cervix is significantly less than in group I and group III, which allows early detection and management of cervical shortening, but at the same time, this method of management of the short cervix is limited.
The result of the accomplished work was the outcome of pregnancy with a short cervix depending on the uterus short cervix management method, of the 125 subjects, delivered full-term-75 (60%), premature births over 34 weeks occurred in 31(24.8%), premature births less than 34 weeks occurred in 17 (13.6%) of the subjects. Pregnancy ended with a late miscarriage in 2 (1.6%) of the subjects.
Comparison of pregnancy outcomes between group I and group II [Table/Fig-1] did not reveal notable statistical differences in the rates of urgent labour, the premature births over 34 weeks long and interruptions of pregnancy with less than 22 weeks long are taken into account. Nevertheless, there were significantly more frequent cases of premature births on the term of less than 34 weeks (CI (95%) 13.7-18.4) in group II (p <0.05).
Outcomes of pregnancy depending on the uterus of short cervix management methods (Group I, Group II).
| Group I | Group II |
|---|
| M % | m | CI+95% | CI-95% | M % | m | CI+95% | CI-95% |
|---|
| Term birth | 63.0 | 6.1 | 75.3 | 50.7 | 58.0 | 8.9 | 75.7 | 40.3 |
| Preterm birth at more than 34 weeks of gestation | 24.0 | 5.4 | 25.4 | 22.6 | 23.0 | 7.6 | 25.8 | 20.3 |
| Preterm birth under 34 weeks of gestation | 11.0 | 4.0 | 12.0 | 10.0 | 16.0 | 6.6 | 18.4* | 13.7* |
| Late spontaneous miscarriage | 2.0 | 1.8 | 2.5 | 1.6 | 3.0 | 3.1 | 4.2 | 2.0 |
* statistically significant between the study groups (p<0.05).
Similar results were obtained when comparing pregnancy outcomes of groups I and III, so statically significant differences were found between groups I and III [Table/Fig-2], in the study of cases {CI (95%) 13.8-18.4} of preterm labour less than 34 weeks (p<0.05). Indicatively more often premature births within the term of less than 34 weeks occurred in groups II and III, comparing with the group I. Comparison of the outcomes of pregnancy in groups II and III did not demonstrated significant statistical differences between them [Table/Fig-3].
Outcomes of pregnancy depending on the uterus of short cervix management methods (Group I, Group III).
| Group I | Group III |
|---|
| M % | m | CI+95% | CI-95% | M % | m | CI+95% | CI-95% |
|---|
| Term birth | 63.0 | 6.1 | 75.3 | 50.7 | 56.0 | 8.8 | 73.5 | 38.5 |
| Preterm birth at more than 34 weeks of gestation | 24.0 | 5.4 | 25.4 | 22.6 | 28.0 | 7.9 | 43.9 | 12.1 |
| Preterm birth under 34 weeks of gestation | 11.0 | 4.0 | 12.0 | 10.0 | 16.0 | 6.5 | 18.4* | 13.8* |
| Late spontaneous miscarriage | 2.0 | 1.8 | 2.5 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 |
* statistically significant between the study groups (p<0.05)
Outcomes of pregnancy depending on the uterus of short cervix management methods (Group II, Group III).
| Group II | Group III |
|---|
| M % | m | CI+95% | CI-95% | M % | m | CI+95% | CI-95% |
|---|
| Term birth | 58.0 | 8.9 | 75.7 | 40.3 | 56.0 | 8.8 | 73.5 | 38.5 |
| Preterm birth at more than 34 weeks of gestation | 23.0 | 7.6 | 25.8 | 20.3 | 28.0 | 7.9 | 43.9 | 12.1 |
| Preterm birth under 34 weeks of gestation | 16.0 | 6.6 | 18.4 | 13.7 | 16.0 | 6.5 | 18.4 | 13.8 |
| Late spontaneous miscarriage | 3.0 | 3.1 | 4.2 | 2.0 | 0.0 | 0.0 | 0.0 | 0.0 |
Comparison of the outcomes of pregnancy in group II and III did not reveal statistically significant differences between the groups.
Discussion
In the present study, we intended to analyse the results of previous surveys in the field and compare them in some way with the results of current experiment. Dodd JM et al., conducted a study on the effectiveness of progesterone in preventing premature birth in the at-risk group. Thirty-six randomised controlled trials (8,523 women and 12,515 children) were included. Progesterone was applied to the group under study, and placebo to the control group. The relation progesterone versus placebo for women with the short cervix (the short cervix diagnosis was identified by ultrasound cervicometry) was associated with a statistically significant reduction in the risk of preterm births among women with less than 34 weeks of gestation (two studies: 438 women, 0.64, 95% CI 0.45 to 0.90), preterm birth up to 28 weeks (two studies: 1115 women, 0.59, 95% CI 0.37 to 0.93). Thus, a convincing evidence base for the effectiveness of the use of progesterone in preventing premature birth has been accumulated so far [22]. The meta-analysis by Conde-Agudelo A et al., [17] and the systematic review of the Cochrane community [23], combining the results of 36 clinical studies of micronised progesterone 17α-hydroxyprogesteronekapronate (17-OPC) involving 8523 patients and an assessment of the state of 12515 newborns were taken into account. The analysis of the results has shown that the use of vaginal progesterone reduces the risk of preterm birth before 34 weeks of gestation by more than 40%, reduces the neonatal morbidity by more than 40%, reduces the number of newborns requiring resuscitation more than two times, reduces the incidence of birth children weighing less than 2500 g by 52% [22,24]. Goya M et al., (n=385) has shown that obstetric pessary leads to a decrease in the number of preterm births <34 weeks of gestation compared with the control group (6% vs. 27%, odds ratio 0.18, 95% CI 0.08 to 0.37, p <0, 0001), moreover a significant difference is observed in neonatal outcomes [19]. Other researchers in their works have not revealed a significant difference in the onset of preterm birth up to 34 weeks of gestation with the preventive use of obstetric pessary in women with the short cervix. Preterm birth rate up to 34 weeks in the pessary group -9.4%, and in the group without application of pessary 5.5% (p=0.46) [25].
A meta-analyses of five randomised controlled trials has shown that vaginal progesterone seems to decrease preterm birth rates in short cervix ≤25 mm (RR = 0,58, 95% CI, 0,42- 0,80) [26]. Cochrane meta-analysis (2013) of 1556 women with the singleton pregnancy and short cervix less than 25 mm has concluded that women who had applied vaginal progesterone as the prophylactic measure in short cervix tend to be less prone to have preterm birth (RR 0.64; 95% CI 0.45–0.90) [10].
Preterm birth rate decreased significantly when applying obstetric pessary in women, with the anamnesis of preterm birth. Alfirevic Z et al., in the surveys on preventing preterm birth in singleton pregnancy [27,28] have compared three methods of the short cervix management and concluded that preterm birth more often happened in the cohort of vaginal progesterone application in comparison with obstetric pessary (32% against 12%, RR= 2,70, 95% CI, 1,10-6,67) [28].
Meta-analysis in 2011 presented the decrease of preterm birth rates under the 35 weeks of gestation, (OR 0.70; 95% CI 0.55–0.89) and unfavourable outcomes of pregnancy (0.64; 95% CI 0.45–OR 0,91) in the group of surgical cerclage in comparison with the group without cerclage [23].
Meta-analysis of the 12 studies done by Li Q et al., included 3328 pregnant women confirmed the lower probability of preterm birth (OR 0,80; 95% CI 0,69–0.9) in the group of cerclage in comparison with the control group. However, the researchers did not identify any significant antenatal morbidity and mortality rates decrease. Moreover, it was associated with the increased risk of side-effects (bleeding, hyperthermia, vaginal discharges) and caesarean section rates (RR 1.19; 95% CI 1.01–1.40) [29].
The mechanism of the cerclage consists of maintaining the biochemical barrier, protecting the inferior pole of the embryonic vesicle from the effects of ascending pathogens. According to the meta-analysis by Berghella V [2], among women with a singleton gestation, previous spontaneous preterm birth, and cervical length less than 25 mm before 24 weeks of gestation the percentage of preterm birth before 35 weeks of gestation was 28.4% (71/250), in the cerclage compared with 41.3% (105/254), in the no cerclage groups (relative risk 0.70, 95% confidence interval 0.55- 0.89). Cerclage also significantly reduced preterm birth before 37, 32, 28, and 24 weeks of gestation. Composite perinatal mortality and morbidity were significantly reduced (15.6% in cerclage compared with 24.8% in no cerclage groups; relative risk 0.64, 95% confidence interval 0.45– 0.91) [22].
In addition, all the authors mentioned above stated that cerclage has a number of complications: the eruption of the cervical issues by the filament, the infection of the ovum, the invasion of the pathogenic flora and the spread of infection along the filaments with the development of local inflammation, the outflow of amniotic fluid, spontaneous abortions, the failure of the sutures, the development of cervical or cervical-vaginal fistulas. The suture on the cervix is applied under local or intravenous anaesthesia.
Endogenous progesterone is necessary for the implantation of maintenance and prolongation of pregnancy. Pharmacokinetics and pharmacodynamics of progesterone are well studied, in 1935 progesterone was primarily synthesised. Currently, there are many studies on the effectiveness of progesterone in preventing premature births. Also, researchers are interested in the optimal ways of taking and dosing the progesterone. Another issue is the lack of randomised controlled trials.
Still the explorers cannot find out unitary conception on the choice of the optimal technique, suture material and the time of application of the cerclage and this might be the pressing problem of further surveys within the proposed topic [23].
Limitation
For an adequate assessment of the effectiveness of methods for managing the short cervix the scope of the samples has to be wider, also it is necessary to conduct multi-centered, randomised studies. Monotherapy is necessary for the evaluation of effectiveness: for example, the use of pessary or cerclage alone. In our work we also investigated the risk factors for the onset of premature birth, anamnestic data, the course of pregnancy (the number of antenatal hospitalisations, the prevention of respiratory syndrome in the foetus), extragenital diseases, etc., however, we only cited data on the effectiveness of methods, since our topic of the article is devoted to evaluating of the effectiveness of methods. Due to the difficulties of accounting, we did not analyse the time of treatment for such risk factors as daily risks in working hours (mental load, night, day, hard work, standing work), socio-economic aspects: family income. In our work we did not investigate the consequences of premature births for newborns.
Conclusion
The short cervix has been identified at the beginning and proved by the results of present survey as a significant predictor of preterm birth: its management helps find relevant solution in reducing the level of preterm birth and maternal mortality and morbidity. Now-a-days, the above mentioned surgical and non-surgical methods of preterm birth prevention in the short cervix, such as cerclage, obstetric pessary and progesterone, require further comparison in randomised studies, taking into account not only pregnancy outcomes but the outcomes for newborns. Ambiguities as for constructing the general tuned scheme of treatment of pregnant women in the group with a risk of preterm birth demand subsequent complex investigations of the short cervix management aimed on decreasing the level of preterm delivery all over the world.
* statistically significant between the study groups (p<0.05).
* statistically significant between the study groups (p<0.05)