Hepatitis B Virus (HBV) is an infectious and most common cause of acute and chronic liver disease, cirrhosis, and hepatocellular carcinoma. Globally, two billion people are estimated to have HBV infection, resulting in over 350 million cases of chronic infection and more than two million deaths annually [1]. In India prevalence of Hepatitis B Surface Antigen (HBsAg) in general population varies from 2% to 8%. Sero-prevalence in HCWs is 2-4 times higher than general population [2].
Occupational exposure includes percutaneous injury, contact with blood or other potentially infectious body fluids. The risk after a single exposure is 6%-30%. In India 40%-65% of HBV in HCWs have been attributed to occupational exposures [3]. Occupational Safety and Health Administration (OSHA) recommends employers to bear responsibility of HCW protection against HBV [3]. However, it is often found that a large proportion of HCWs are still not vaccinated or partially vaccinated due to lack of awareness. Centers for Disease Control and Prevention (CDC) clearly recommends that if non protective after first series of vaccination (1st, 2nd and 3rd), HCWs should be administered 2nd series of vaccination (4th, 5th and 6th), following, titres should be checked after 6-8 weeks of last dose. If non protective after 2nd complete series of vaccination (and HBsAg, anti-HBc negative) HCWs are termed as non-responders to vaccination and should be given counselling as of how to prevent HBV transmission to others and also regarding the treatment options [4].
Housekeeping staff are exposed to more risk as they are also involved in handling of inappropriately discarded bio medical waste. The vaccination coverage is low among them because of their low educational and socio-economic status. Structured questionnaire is the best way to assess lacunae in KAP and it further helps in planning educational and interactive sessions. To the best of our knowledge this is the first study conducted in India, to do KAP assessment using Turning point technology, an innovative method using clickers. Turning point has been widely employed in medical education and training, which will ease the process of assessment and analysis and most of all, data will be more precise [5]. The aim of the study is to assess the impact of educational intervention on vaccination coverage among housekeeping staff.
Materials and Methods
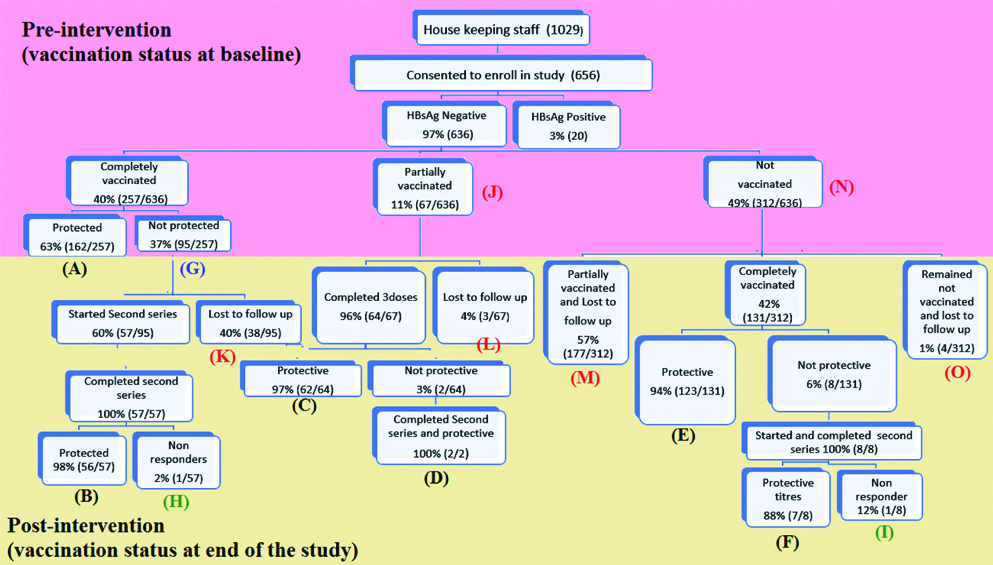
The present study was a case control study which was conducted in two phases as shown in [Table/Fig-1].
Hepatitis B vaccination status among housekeeping staff (pre and post intervention phases).
Box A-F: Completely vaccinated and protected
Box G: Completely vaccinated (1st series) and not protected
Box H-I: Completely vaccinated (2nd series) and not protected (Non Responders)
Box J-M: Partially vaccinated (1st or 2nd series)
Box N-O: Not vaccinated
This study was conducted at Office of Hospital Infection Control Committee (HICC) and Department of Microbiology for six months, from April-September 2017. The study was approved by undergraduate research monitoring committee and Institute ethics committee with registration No. PRO1176_V1.
Inclusion Criteria
The study participants are all the housekeeping staff who is outsourced under company named Service Master Class (SMC). Written consent was taken from all the housekeeping staff at the beginning of the study.
Exclusion Criteria
The housekeeping staff who didn’t consent or didn’t turn at baseline were excluded from the study.
Sample Size
The sample size was estimated using the statistical formula for comparing two related proportions. The minimum expected difference in proportion between the pre and post knowledge was kept as 0.30 (10% v/s 40%). The sample size was estimated at 5% level significance and 90% power. The sample size calculated for the given study was 457. However, during the study 656 housekeeping staff gave consents to enroll in the study and was included in the study for their betterment.
Preparation of Materials for Educational Intervention
A structured power point presentation was designed for conducting educational intervention on hepatitis B vaccination comprising of various areas of hepatitis B viral disease, its mode(s) of transmission, prevention of HBV by vaccination and post-exposure prophylaxis of HBV. Apart from that, informative leaflets and individual and group discussions were done.
Study Procedure
Phase-1 (interventional phase): The participants were divided into smaller groups of 30-50 and multiple sessions were conducted.
Pretest: Comprised of structured questionnaire on KAP of hepatitis B vaccination, was conducted in power point using Turning point application, an interface for polling in power point, which helps in instant valuation of the results and further displays the results in a graphical format immediately. By using this we could achieve 100% response rate for the questionnaire.
Educational intervention: After pretest, the educational intervention was carried out which covered various areas of hepatitis B such as: i) symptoms, organ affected; ii) its mode(s) of transmission; iii) prevention of HBV by vaccination; and iv) post-exposure prophylaxis of HBV.
Vaccination follow-up: The baseline vaccination status of the housekeeping staff was recorded in a HBV vaccination card.
Phase 2 (post-interventional phase): Phase 2 included the subsequent visits, during which the following activities were carried out.
Post-test: After one month, the post test was conducted using the same questionnaire. Knowledge on HBV was tested before and after educational intervention, whereas attitude and practice regarding prevention of transmission on HBV was analysed only before educational intervention.
Vaccination follow-up: Participants were followed up for impact.
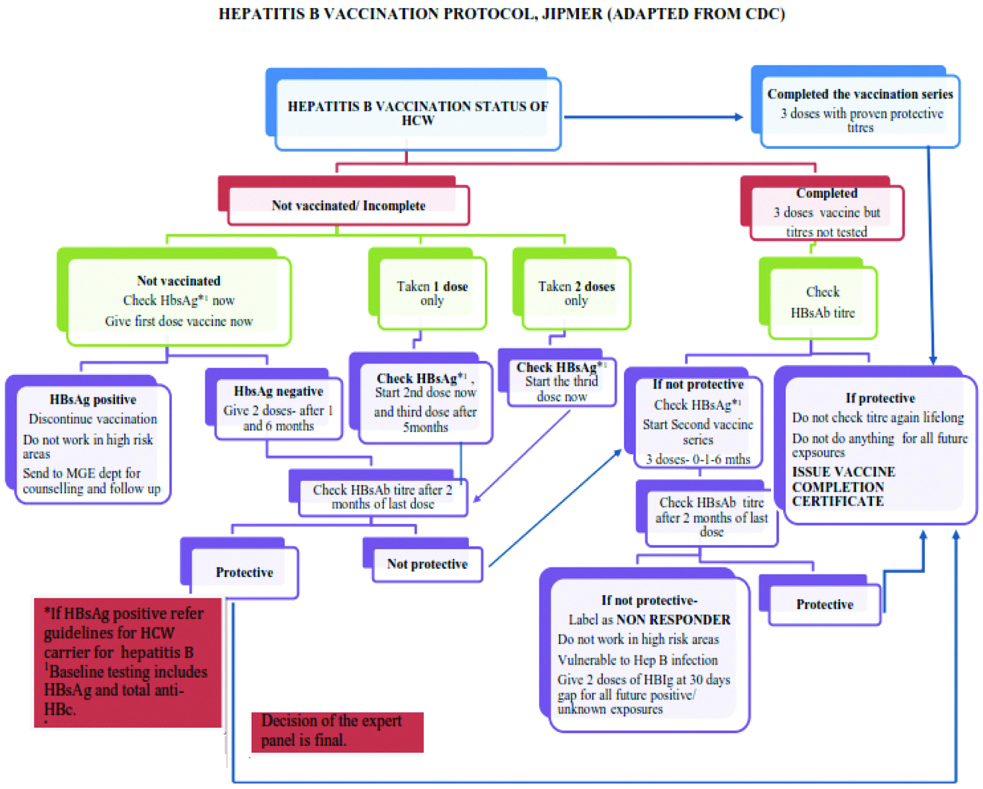
Hepatitis B vaccination strategy: Hepatitis B vaccination as per Hepatitis B vaccination protocol is described in [Table/Fig-2].
Hepatitis B vaccination protocol at JIPMER (adapted from CDC).
Vaccination Categorisation Definitions
The following definitions were used to categorise the study participants.
Completely vaccinated and protective: Participants who have taken complete course i.e., three doses of hepatitis B vaccine (0, 1, 6) and anti-HBs titre >10 mIU/mL.
Protected at base line: Tested previously and produced documented report of anti-HBs titre.
Protected at end of the study: Tested for anti-HBs titre during the study period.
Partially vaccinated:Partially vaccinated at base line: Participants who has taken 1 or 2 doses of vaccine at base line.
Remained partially vaccinated at end of the study: participants who has taken 1 or 2 doses of vaccine during the study period but did not complete the series at the end of study due to loss to follow-up.
Not vaccinated:Not vaccinated at baseline: Participants who had not taken any dose of vaccine at base line.
Remained not vaccinated at end of the study: Participants who enrolled in the study but remained not vaccinated at the end of study due to loss to follow-up.
Non responders to hepatitis B vaccination: Participants whose titres remained not protective after 2 complete series (6 doses) of vaccine and HBsAg and anti HBc tested negative.
Non-responders at base line: Tested for anti-HBs titre previously.
Non-responders at end of the study: Tested for anti-HBs titre during the study period.
Lost to follow-up: They include the participants who enrolled in the study but lost to follow-up. This include both:
Remained partially vaccinated at end of the study (refer definition category 2b).
Remained not vaccinated at the end of the study (refer definition category 3b).
Results
Out of 1029 housekeeping staff, 656 were given their consent to enroll in the study.
None of the housekeeping staff had documentation of Anti HBs titre, HBsAg was tested among all housekeeping staff as an institute policy. A 3.1% (20/656) of housekeeping staff tested positive for HBsAg. This staffs were excluded from educational intervention and were referred to medical gastroenterologist for follow-up and treatment. The remaining 636 study participants were included for intervention.
Knowledge on Disease, Transmission, Prevention and Post Exposure Prophylaxis for HBV
From the [Table/Fig-3], it is evident that only 54% (344/636) of study participants were familiar with the term HBV. It’s surprising to see that only 11% (73/636) knew that there is no definitive treatment for HBV. Also, it can be noted that only 52% (329/636) were aware that HBV is a transmissible through needle stick, sharps and splash injury from infected body fluid.
Knowledge on disease, transmission, prevention and post exposure prophylaxis of hepatitis B (N=636).
| Response to knowledge based questionnaire | Correct response% (n) | Improvement% (p-value) |
|---|
| Pre intervention | Post intervention |
|---|
| Knowledge on hepatitis B viral disease (N=636) |
| 1 | Familiarity with the term hepatitis B viral disease | 54 (344) | 87 (557) | 33 (p<0.0001) |
| 2 | There is no definitive treatment for HBV | 11 (73) | 51 (325) | 40 (p<0.0001) |
| 3 | Common symptoms | 8 (52) | 89 (566) | 81 (p<0.0001) |
| 4 | Complications such chronic liver disease | 20 (129) | 69 (438) | 49 (p<0.0001) |
| 5 | Longstanding HBV cause cancer | 17 (110) | 82 (523) | 65 (p<0.0001) |
| Average response on Hepatitis B viral disease | 22 | 76 | 54 (p<0.0001) |
| Knowledge on hepatitis B viral transmission (N=636) |
| 1 | Transmissible between persons | 69 (438) | 93 (589) | 24 (p<0.0001) |
| 2 | Transmission through needle stick injury; sharps or splash with blood and body fluid | 52 (329) | 87 (551) | 35 (p<0.0001) |
| 3 | Transmission from mother to foetus during pregnancy | 25 (159) | 69 (438) | 44 (p<0.0001) |
| 4 | Transmission through sexual route | 51 (323) | 91 (576) | 40 (p<0.0001) |
| 5 | Non transmission through inhalation or oral route | 30 (191) | 82 (523) | 52 (p<0.0001) |
| Average response on Hepatitis B viral transmission | 45 | 82 | 37 (p<0.0001) |
| Knowledge on prevention of HBV (N=636) |
| 1 | Availability of vaccine for prevention of Hepatitis B | 47 (298) | 98 (623) | 51 (p<0.0001) |
| 2 | HBV vaccination is administered in 3 doses | 42 (268) | 95 (603) | 53 (p<0.0001) |
| 3 | 1 or 2 dose does not provide lifelong protection | 30 (189) | 92 (583/) | 62 (p<0.0001) |
| 4 | Full vaccination (3 doses), does not necessarily mean it offers protection for life time | 23 (146) | 88 (561) | 65 (p<0.0001) |
| 5 | Availability of testing method to check for protection | 36 (232) | 78 (498) | 42 (p<0.0001) |
| Average response on prevention of HBV | 36 | 90 | 54 (p<0.0001) |
| Knowledge on post-exposure prophylaxis of HBV (N=636) |
| 1 | If titres protective (documented), no need of revaccination irrespective of source status | 23 (146) | 70 (448/636) | 47 (p<0.0001) |
| 2 | If titres not protected and exposed to source unknown or positive, immunoglobulin plus vaccine is recommended | 14 (89) | 62 (395/636) | 48 (p<0.0001) |
| 3 | Immunoglobulin must be taken within as soon as possible following exposure | 39 (245) | 67 (424/636) | 28 (p<0.0001) |
| 4 | One dose of immunoglobulin does not give life time protection | 21 (132) | 57 (363/636) | 36 (p<0.0001) |
| 5 | Vaccination is much more cost effective than immunoglobulin | 32 (205) | 94 (596/636) | 62 (p<0.0001) |
| Average response on Post-exposure prophylaxis of HBV | 26 | 70 | 44 (p<0.0001) |
Only 36% (232/636) was aware that anti- HBs titre can be tested to determine the lifetime protection status. This clearly signifies the role of educational intervention to enhance the awareness for hepatitis B vaccination.
The average response on knowledge about post-exposure prophylaxis of HBV was 26%.
One month post educational intervention, knowledge based questions were reassessed and significant improvement was noted. Average correct response on hepatitis B viral disease increased to 76% from 22%, HBV transmission raised to 82% from 45%, prevention of HBV response escalated to 90% from 36%, post-exposure prophylaxis response improved from 26% to 70%.
Attitude/Practice towards Prevention of Hepatitis B Vaccination
In the present study, 49% (312/636) participants were not vaccinated against HBV and their predominant reason was owing to the fact that they were not aware of existence of vaccine against HBV (60%)(184/312). A 51% (324/636) housekeeping staff had started first dose of HBV vaccine; prime reason of their awareness was influence from their colleagues 43% (138/324) followed by advice by the HICC team 28% (91/324).
An 11% (67/636) of HCWs had discontinued HBV vaccine and hence were partially vaccinated, due to forgetfulness (49%) followed by the myth that one dose suffices to protect lifetime against HBV. We noted that 257 (56%) study participants had taken 3 doses of HBV but were not tested for anti HBs titre and reason being their unawareness of the anti HBs titre testing.
Hepatitis B Vaccination Status
At baseline, 40% (257/636) were completely vaccinated, 11% (67/636) partially vaccinated and 49% (312/636) were not vaccinated against HBV. Out of 257 HCWs who were completely vaccinated 63% (162/257) were protected and 37% (95/257) were not protected. Among 95 HCWs who were not protective, second series of HBV vaccine was initiated for 57 HCWs and rest (38) remained lost to follow-up. Following completion of second series (57), only one HCW was termed non responder to HBV.
Among 67 HCWs, who were partially vaccinated at baseline, vaccination was completed for 64. The second series was initiated for 2 non-protective HCWs and both were tested protective after completion of second series of vaccination.
As shown in [Table/Fig 4], 312 HCWs were not vaccinated against HBV at the baseline and among them, 131 received complete three doses (out of which 123 were tested protective); 177 HBV vaccination was initiated but later they remained lost to follow-up; four remained not vaccinated (lost to follow-up) till end of study period. Second series was initiated in eight HCWs who were not protective after first series of vaccine, only one was termed non responder.
Response to attitude and practice based questionnaire (N=636).
| Attitude and practice based questions | Response% (n/N) |
|---|
| 1. Reason for not being vaccinated (HCWs not vaccinated at baseline, N=312) |
| a | Was not aware of vaccine for HBV | 60 (184/312) |
| b | Did not know the availability of vaccine in our hospital | 23 (73/312) |
| c | Was under belief that vaccine is very expensive | 12 (38/312) |
| d | Don’t believe that vaccine will give protection | 5 (16/312) |
| e | For religious region (e.g. Pentacostal and Jheova Christians do not take injections) | 0.3 (1/312) |
| 2. Reason for starting vaccination (HCWs completely or partially vaccinated at baseline, N=324) |
| a | Suggested by colleague or friends to start vaccine | 43 (138/324) |
| b | Was advised in HICC office | 28 (91/324) |
| c | Was advised by doctors | 8 (26/324) |
| d | Was enforced by housekeeping supervisor | 20 (65/324) |
| e | Had a needle stick injury and then got the awareness | 1 (4/324) |
| 3. Reason for discontinuation of second or third dose? (HCWs partially vaccinated at baseline, N=67) |
| a | Lack of time | 9 (6/67) |
| b | Forgot to take on the due date | 49 (33/67) |
| c | Thought one/two dose was/were sufficient | 31 (21/67) |
| d | Vaccine was not available on the due date | 3 (2/67) |
| e | Had side effects after first dose | 7 (5/67) |
| 4. Reason for not checking anti-HBs titre (HCWs completely vaccinated at baseline, N=257) |
| a | Was not informed to check titre during vaccination | 56 (143/257) |
| b | Was told to check titre, but forgot later | 11 (28/257) |
| c | Was not aware of where to go for titre checking | 4 (11/257) |
| d | Was not aware that test is free | 12 (31/257) |
| e | Believed that fully protected if finished full vaccination | 17 (44/257) |
*The HCW who were completed vaccinated did not have the titres checked at baseline.
As summarised in [Table/Fig-5], 65% (414/636) of the housekeeping staff were protected against HBV at the end of the study; 26% (162/636) were found protective at baseline and 41% (412) became protective during the study period) and 0.6% (4) remained not vaccinated (49% at baseline) by the end of the study period.
Response to hepatitis B vaccination.
| Pre intervention % (n/N) | Post intervention % (n/N) | p-value |
|---|
| Completely vaccinated | 40 (257) | 65 (414) | p<0.0001 |
| Completely vaccinated and protected | 26 (162)(Box-A)* | 64.7 (412) (Box-A to F)* | p<0.0001 |
| Completely vaccinated (1st series) and not protected | 15 (95/636)(Box-G)* | 0 | p<0.0001 |
| Completely vaccinated (2nd series) and not protected (Non Responders) | Not applicable** | 0.3 (2)(Box-H to I) | - |
| Partially vaccinated (1st or 2nd series) | 11 (67)(Box-J)* | 34.2 (218)*** (Box-K to M)* | p>0.05 |
| Not vaccinated | 49 (312)(Box-N)* | 0.6 (4)***(Box-O)* | p<0.0001 |
*Refer to the boxes in [Table/Fig-1]
**Not applicable as the study participants were not received second series at baseline
***Study participants who remained partially vaccinated (218/636) or non-vaccinated (4/636) till the end of the study are categorized as ’Lost to follow up’ as they could not be followed up for vaccination till the end of the study period.
In our study, we also analysed various demographic characteristics [Table/Fig-6]. Among the vaccinated group, majority were females (87%). Vaccination compliance was poor in low educated HCWs (21%). Majority of the not vaccinated group (96%) was from rural locality.
Influence of sociodemographic characteristics, job experience and knowledge at baseline on vaccination among housekeeping staff.
| Variables | Vaccinated (N=324) % (n/N) | Not vaccinated (N=312) % (n/N) | Total (N=636) % (n/N) |
|---|
| Gender |
| Male | 13 (42/324) | 30 (95/312) | 22 (137/636) |
| Female | 87 (282/324) | 70 (217/312) | 78 (499/636) |
| Basic education |
| Low educated | 21 (69/324) | 38 (118/312) | 29 (187/636) |
| Educated | 79 (255/324) | 62 (194/312) | 71 (449/636) |
| Locality |
| Urban | 18 (58/324) | 4 (14/312) | 11 (72/636) |
| Rural | 82 (266/324) | 96 (298/312) | 89 (564/636) |
| Job experience |
| <1 year | 13 (41/324) | 26 (82/312) | 19 (123/636) |
| >1 year | 87 (283/324) | 74 (230/312) | 81 (513/636) |
| Knowledge on HBV at baseline |
| Poor Knowledge (<30%) | 26 (85/324) | 80 (249/312) | 53 (334/636) |
| Good knowledge (>30%) | 74 (239/324) | 20 (63/312) | 47 (302/636) |
We categorised knowledge based questionnaire results into score and we divided into 2 groups; poor knowledge (score <30%), good knowledge (score ≥30%). It is evident from the [Table/Fig-6] that HCWs with good knowledge (74%) were more compliant to vaccination compared to HCWs with poor knowledge (26%).
Discussion
The most important approach for the prevention of occupational HBV infection is by improving the compliance of HCWs to HBV vaccine. Housekeeping staff accounts for the lowest compliance to vaccination because of their lack of awareness. We found that 3% (20/656) were HBsAg positive. In various study conducted from India, hepatitis B prevalence in HCWs has reported to be 1% by Sukriti et al., and 0.4% by Singhal V et al., [6,7]. Numerous study has illustrated that risk of contracting HBV is two to four times higher in HCWs than other adult population [7-11].
When we analysed HBV vaccination status among HCWs, it was noted that 40% (257/636) were completely vaccinated, but did not have documentation of protective titres; 11% (67/636) had taken one or two doses of vaccine, but had missed subsequent doses and 49%(312/636) were non vaccinated. Concordance to our study Pathak R et al., also reported 40% full vaccination coverage, 20% were partially vaccinated and 40% were not vaccinated among HCWs in a tertiary hospital in north India [2]. Singhal V et al., [9] conducted a study in 2008 and reported HBV vaccination coverage of 56.5% which improved to 97.5% after applying well-planned and clear policy for vaccination [11].
In spite of constant effort to educate all HCWs, we saw that study group HCWs had poor knowledge on HBV (22%), its transmission (45%), prevention (36%) and post exposure prophylaxis (26%). Based on this, we planned educational sessions. In post intervention questionnaire response we saw drastic rise in response to awareness on Hepatitis B which reflects on successful educational sessions. Mesfin YM et al., analysed KAP towards hepatitis B among medical students in Haramaya University, and concluded that there was poor knowledge on transmission and prevention of HBV [12]. There is no study in India of such magnitude, which has analysed role of educational intervention on improving the knowledge and compliance of hepatitis B vaccination.
We found that vaccination coverage was more among females (87%), maybe due to higher representation of females in our study. Similar findings were observed by Pathak R et al., and Pathoumthonga K et al., Vientiane, Laos. Educated HCWs had better compliance [2,13]. van der Veen YJ in a Turkish Dutch survey, reported that highly educated HCWs have better knowledge and hence better compliance to vaccination [14]. We also found that urban locality population has better compliance similar to study by ul Haq N et al., [15]. In the present study percentage of HCWs protected from HBV increased from 26% to 39%.
Limitation
Study was conducted in a single institute in Southern India. Further studies need to be done for providing adequate comparison.
Conclusion
Authors conclude that HBV vaccination compliance and awareness on prevention of HBV can be drastically improved by well-planned educational intervention. Study of this magnitude is first of its kind in South Asia, structured to analyse the role of educational intervention by novel turning point technology, to increase vaccination compliance. We consider that all cadre of HCWs ranging from doctors, nurses or housekeeping staff have right to be protected against hepatitis B in view of their increased risk from occupational exposure. Having institutional protocol, availability of vaccine and test for Anti HBs titre will largely influence the vaccination compliance.