The loss of continuity of the lower jaw following surgical excision destroys the balance and symmetry of mandibular functions. Prosthodontic rehabilitation has, therefore, become the treatment option to restore functions, aesthetics and to alleviate psychological status in such patients who deny further surgical intervention or in whom surgical reconstruction procedures are not indicated.
This case report describes a prosthodontic rehabilitation of a patient who has undergone a hemimandibulectomy with the overlay denture lined with the silicone liner to fulfil the patient’s needs and requirements.
Case Report
A 56-year-old male patient reported to the Department of Prosthodontics with the chief complaint of difficulty in chewing food due to missing teeth [Table/Fig-1]. The patient was diagnosed with squamous cell carcinoma of right buccal mucosa and had undergone mandibulectomy and radical neck dissection two years back. The patient also gave the history of postoperative radiation for six months.
Extraoral view showing deflection of mandible to affected right side.

Intraoral examination showed thick and freely movable soft tissue with scar in the lower right posterior region and loss of alveolar ridge with obliteration of buccal and lingual sulci, posterior to 41 region [Table/Fig-2]. Teeth missing in maxillary arch were 15,16,17 and in mandibular arch teeth present were 32,33,34,35,37 and 38. Eighteen teeth were present, but not considered in the treatment planning making it Kennedys class II condition [Table/Fig-3,4]. On occluding the maxillary and mandibular arches, the occlusal surfaces of left maxillary teeth were more buccal in position in relation to the occlusal surface of the mandibular left teeth. There was no contact of the occlusal surface of the left maxillary and mandibular teeth [Table/Fig-5].
Intraoral view of patient showing defect area.

Intraoral view of patient showing mandibular arch.

Intraoral view of patient showing maxillary arch.

Intraoral view of patient showing the occlusion.

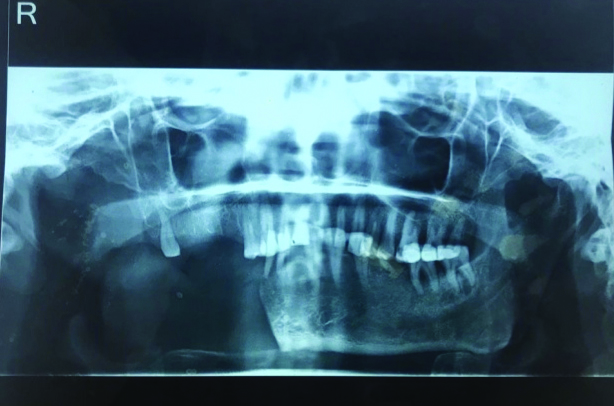
On extraoral examination, facial asymmetry and deviation of mandible on the right side was seen. Palpation disclosed absence of right condyle and ramus. Orthopantomogram [Table/Fig-6] showed the absence of the right mandible till the midline which makes it Class III mandibular defect as per the classification given by Cantor and Curtis [1].
The patient denied for any further surgical procedures such as reconstructive surgery, vestibuloplasty or implant therapy. And hence the treatment planned for this patient was a conventional removable partial prosthesis for maxillary arch and for mandibular arch complete denture prosthesis submerging the present teeth in the denture base and establishing new occlusal contacts to enhance the masticatory efficacy.
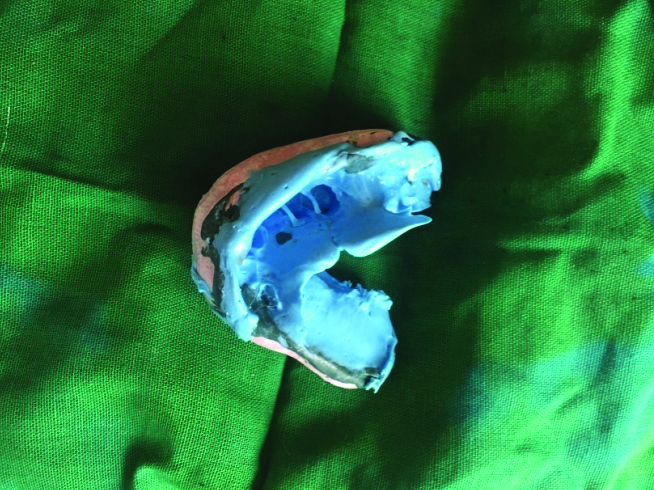
A stainless steel stock edentulous tray was modified by trimming buccal flange of the right half of the tray and the preliminary impression was made with the vinyl polysiloxane impression material (Zetaplus, Zhermack Spa, Italy) [Table/Fig-7]. The impression was poured in dental stone (Kalstone; KalabhaiKarson Pvt., Ltd.,) to obtain the primary models [Table/Fig-8]. The cast was retrieved and the mandibular custom tray was fabricated with autopolymerising acrylic resin (DPI Cold Cure; Dental products of India, Mumbai, India) with a thick spacer adapted over the entire mandibular ridge including the teeth and the defect area. The borders of the custom tray were adjusted to conform to the limiting structures, especially the defect area. A sectional border molding procedure was performed with low fusing impression material (DPI), starting with normal (left) side first, followed by the defect side.


Tissues in the defect area were recorded by asking the patient to perform tongue movements, wide opening and closing movements and swallowing maneuvers. This procedure of recording the defect area was repeated till the maximum acceptable stability was achieved. After border molding, the wash impression was made with light body elastomeric impression material (Zetaplus, Zhermack Spa, Italy) [Table/Fig-9].
Mandibular final impression.
The occlusal surfaces of maxillary teeth were more buccal in position due to which there was no contact of maxillary and mandibular teeth. Therefore, temporary record base was fabricated that covered the left mandibular posterior teeth and the wax rims were made over it to establish a new jaw relation at acceptable vertical jaw relation. To assess the vertical dimension of occlusion, the patient’s sense of comfort and tactile sense were used. The patient was then instructed to move his mandible as far as possible to the left side and close the mandibular jaw gently into position. This was done to record the functional maxillomandibular relationship [Table/Fig-10].
Jaw relation with occlusal rim.

Semi anatomic teeth were selected and were arranged in maximum intercuspation [Table/Fig-11,12 and 13]. However, the patient was presumed to masticate only on left side. Processing of denture was done in a conventional manner.
Try-in showing frontal view.

Try-in showing occlusion of left lateral side.

Try-in of overlay denture.

Resilient liner (PermaSoft Denture Liner; DentsplyAustenal, York, PA) was used to reline the intaglio surface of the mandibular denture while keeping mandible into centric occlusion. It helped to improve the tissue contact of the defect area and to utilise the maximum retention from available teeth on the lower left side. Moreover, it provided cushioning effect and minimised the stresses over the lower left teeth [Table/Fig-14].
Relined mandibular overlay denture.
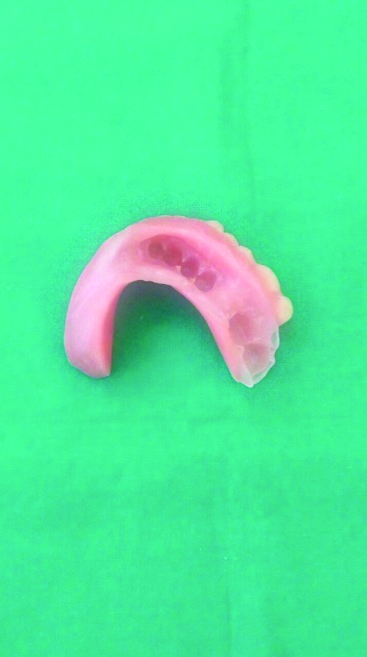
The removable partial denture was fabricated to replace 15,16 and 17 in a conventional manner. Upper removable partial denture and lower relined overlay denture was delivered and post-insertion instructions were given to the patient [Table/Fig-15]. The patient was recalled after 24 hours for necessary modifications. The patient was instructed to start eating a soft diet after 15 days of denture insertion from the left side so as not to hamper the retention and stability of the prosthesis and was asked to meticulously keep good oral hygiene. Deviation of the mandible was drastically improved with the prosthesis in place [Video-1].
Polished surface of mandibular overlay denture and maxillary partial denture.

The patient was adivsed to do simple exercises such as repeated opening and closing of the mandible. This helped the patient to learn to manipulate the mandible into proper position.
Discussion
Trauma, congenital deformity or neoplasm are the most common indications for the complete or partial mandibulectomy. Complete denture prosthesis is considered as one of the most difficult and unrewarding treatment options in dentistry. And this treatment option becomes more difficult in cases with the maxillofacial defects. The functional and esthetic oral rehabilitation of the resected mandible remains one the most chall enging procedures confronting the maxillofacial prosthodontist [2].
Discontinuity of the mandible leads to altered mandibular functions [3]. Such cases require an intervention by the physical therapy followed with prosthodontic treatment. Physical therapy such as simple opening and closing exercises of the mandible helps to establish the symmetrical arc of closure and thus helps to record proper centric relation at the time of jaw relation. Various prosthetic treatments are also employed to reduce deviation and improve the masticatory efficacy [4].
Retention of the prosthesis in such compromised cases can be gained from the remaining alveolar ridge after resection, the supporting structures, sulcus depth and remaining natural teeth if present [5]. The contracture of mucosa after surgical closure results into the scar formation which further threatens the denture stability.
In this case, the mandibular left teeth were present and were very lingual in relation to the maxillary posterior left teeth and hence the guide plane appliances for correction of the deviation of the mandible to the defected side could not be the treatment option. Palatal ramp prosthesis was also not indicated in this case due to the occlusion that was present in the patient. It is an established fact that occlusion influences the retention of the denture [6].
Occlusal scheme for mandibular defect varies in patients, depending on the extent of the defect and the teeth present on the non defect side. In this case, mandibular arch was treated as completely edentulous arch as the remaining mandibular left teeth were submerged completely in the denture base. It was not possible to develop bilaterally balance occlusal scheme in eccentric positions due to mesial movement of resected mandible and hence a new set of semi anatomic teeth were arranged in maximum intercuspation with the opposing maxillary teeth.
It has been reported that the overlay dentures not only improves the biting forces, stability and retention but also minimises the resorption of alveolar bone when compared to conventional complete dentures [7]. Proprioception is also maintained due to the presence of teeth and the negative psychological aspect of patients of being toothless is perished. Moreover, overlay dentures can be easily converted to complete denture over a period of time.
In 1978, Rissin L et al., carried out a study to evaluate the efficacy of masticatory performance [8]. He selected patients with natural dentition, complete dentures and overdentures and concluded that the natural dentition had highest masticatory efficiency followed by over-denture patients and lowest masticatory efficacy for the complete denture wearers.
Dhanaraj SP et al., reported a case in which he rehabilitated the resected mandible with the help of overlay dentures that helped to restore the normal functions, esthetics and symmetry [9].
The fabricated overlay complete denture was relined with resilient reliner that helped to distribute the forces evenly over the unresected alveolar ridge and the teeth that were covered under the denture. Denture relining is an economical means of improving a denture’s stability and retention [10]. Relining the denture also compensated for the discrepancies in the fit by engaging the undercuts and the close adaptation with the tissues. It has been well documented in the literature that soft liners absorbs the energy generated by the masticatory impact and increases the retention of the prosthesis by intimate contact with the tissues [11]. Moreover, in this case, the relined intaglio surface of the denture over the area of teeth gave a cushioning effect to teeth and reduced the stresses of masticatory impact over them. The relining also engaged the undercuts present in the teeth that added in the retention of the prosthesis.
Conclusion
Fabricating an overlay denture and relining it with soft liner is a novel way to minimise the trauma of compromised underlying denture-supporting tissues and to improve the retention of the prosthesis by maintaining intimate contact with the tissues.
Overlay dentures are an alternative treatment option preferred over the implant dentistry, especially in compromised conditions and when the patients are unwilling for the surgical treatment options. Overlay dentures and relining the dentures is one of the most practical measures used in preventive dentistry.
The treatment option opted in this case followed the DeVan’s golden statement that, perpetual preservation of what remains is more important than the meticulous replacement of what is missing.
[1]. Beumer J, Curtis T, Marunick MT, Maxillofacial rehabilitation: Prosthodontic and surgical consideration 1996 St.Louis, OKIshiyaku Euro America:184-188. [Google Scholar]
[2]. Taylor TD, Diagnostic considerations for prosthodontic rehabilitation of the mandibulectomy patient. In: Taylor TD, editorClinical maxillofacial prosthetics 2000 ChicagoQuintessence Publishing:155-70. [Google Scholar]
[3]. Prakash V, Prosthetic rehabilitation of edentulous mandibulectomy patient. A clinical reportIndian J Dent Res 2008 19:257-60.10.4103/0970-9290.4296118797105 [Google Scholar] [CrossRef] [PubMed]
[4]. Shetty P, Baliga M, Rodrigues S, Dixit S, Prosthetic management following mandibular resection: Clinical reportJ Nepal Dental Assoc 2009 10:57-60. [Google Scholar]
[5]. Sahin N, Hekimoglu C, Aslan Y, The fabrication of cast metal guidance flange prostheses for a patient with segmental mandibulectomy: a clinical reportJ Prosthet Dent 2005 93:217-20.10.1016/j.prosdent.2004.12.00715775921 [Google Scholar] [CrossRef] [PubMed]
[6]. Castillo RD, LaMar F Jr, Ercoli C, Maxillary and mandibular overlay removable partial dentures for the treatment of posterior open-occlusal relationship: a clinical reportJ Prosthet Dent 2002 87:587-92.10.1067/mpr.2002.12557812131878 [Google Scholar] [CrossRef] [PubMed]
[7]. Aruna U, Thulasingam C, Prosthodontic management of segmental mandibulectomy patient with guidance appliance and overlay dentureJ Indian Prosthodont Soc 2012 13(4):593-99.10.1007/s13191-012-0208-824431797 [Google Scholar] [CrossRef] [PubMed]
[8]. Rissin L, House JE, Manly RS, Kapur KK, Clinical comparison of masticatory performance and electromyographic activity of patients with complete dentures, overdentures, and natural teethJ Prosthet Dent 1978 39:508-11.10.1016/S0022-3913(78)80181-4 [Google Scholar] [CrossRef]
[9]. Dhanaraj SP, Annapoorni H, Rehabilitation of a hemimandibulectomy patient with an overlay denture- a case reportJ Clin Diagn Res 2018 12(9):ZD03-ZD05.10.7860/JCDR/2018/34939.12034 [Google Scholar] [CrossRef]
[10]. Garcia LT, Jones JD, Soft linersDent Clin North Am 2004 48(3):7099-720.10.1016/j.cden.2004.03.00115261801 [Google Scholar] [CrossRef] [PubMed]
[11]. Shim JS, Watts DC, An examination of stress distribution in a soft lined acrylic resin mandibular complete denture by finite element analysisInt J Prosthodont 2000 13:19-24. [Google Scholar]