An Overview on the Protocols used in the Management of Infertility
Kundan V Ingale1, Anoop Laxminarayan Hajare2, Swati Uday Naik3
1 Infertility Specialist, Department of Obstetrics and Gynecology, Nirmiti Clinic, Pune, Maharashtra, India.
2 Senior Manager, Department of Medical Services, Emcure Pharmaceuticals Ltd., Pune, Maharashtra, India.
3 Head and Associate Director, Department of Medical Services, Emcure Pharmaceuticals Ltd., Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anoop Laxminarayan Hajare, House No. 9-880, Shahabazar, Gulbarga, Karnataka-585103, India.
E-mail: Anoop.Hajare@Emcure.co.in
Infertility is currently a huge burden in India. Artificial Reproductive Techniques (ART) are helpful for the couples in various cases of infertility. Various drugs are available today which includes ovulation inducing agents like clomiphene or letrozole, gonadotropins like Follicle Stimulating Hormone (FSH) and menotropins (Human Menopausal Gonadotropin; HMG) for follicular growth. Also, certain drugs are available, used for controlling the ovarian stimulation or causing hyperstimulation which includes Gonadotropin Releasing Hormone (GnRH) analogues.
GnRH analogues especially the antagonists (e.g., Cetrorelix, Ganirelix) are the commonly used drugs for down regulating the gonadotropin production from the pituitary which eventually helps in avoiding the premature Luteinizing Hormone (LH) surges. These hormonal preparations like FSH, HMG are available as urinary (uFSH), Highly Purified (HP-FSH) and/or recombinant (rFSH) preparations. Even with the availability of so many drugs today, infertility management is a challenge to the doctors. Choosing a right protocol is still a widely debated topic and requires years of clinical experience. Currently there are no guidelines recommending the use of drugs which are available today. This overview helps in understanding the commonly used protocols in the management of infertility.
Antagonist, Cetrorelix, Follicle stimulating hormone, Gonadotropin releasing hormone
Infertility is becoming a healthcare and social menace across the globe. National Institute for Health and Care Excellence (NICE), 2013 recommends In-Vitro Fertilisation (IVF) to be a definitive treatment for infertile patients who failed with other treatment options [1]. The number of babies born with the use of ART exceeded five million [2]. It is studied and observed that the success of IVF treatment depends on obtaining an adequate or sufficient number of eggs to obtain high-quality of transferable embryos without exposing the patient to the risks of excessive ovarian stimulation [2].
Controlled Ovarian Hyperstimulation (COH) is established as a pre-requisite in ART as it helps in achieving twin objective of IVF treatments, one to have sufficient number of transferable embryos and second to minimise the risk of excessive ovarian stimulation or OHSS as a result of COH [3]. It has also been studied that higher the oocyte yield, higher the probability to achieve a live birth after utilisation of all cryopreserved embryos [4].
Controlled Ovarian Stimulation (COS) comprise three basic elements [4]:
Exogenous gonadotropins for multi-follicular development;
Regulation of pituitary function and/or to prevent premature ovulation: Co-treatment with GnRH analogues;
GnRH agonist or
GnRH antagonist
Final oocyte maturation trigger: 36-38 hours prior to oocyte retrieval.
The success of any COH protocol depends upon choosing individualised COS protocol. GnRH analogues whether agonist or antagonist are widely employed with the ultimate aim of down regulating the cycles. However, recently GnRH antagonist protocols are widely used due to the fear of OHSS which is comparatively more likely with GnRH agonists and Human Chorionic Gonadotropin (HCG). An overview of these protocols is as follows.
Stimulation Protocols:
GnRH analogues are widely used in stimulation protocols either to down regulate the cycle or to prevent the premature LH surge.
GnRH agonist:
Long agonist protocol;
Short agonist protocol;
Micro-dose flare protocol.
Ultrashort protocol.
GnRH antagonist:
Single dose fixed;
Multiple dose:
Flexible antagonist protocol;
Fixed antagonist protocol.
A combination of two protocols (Agonist+Antagonist protocol).
Long Agonist Protocol [
5]
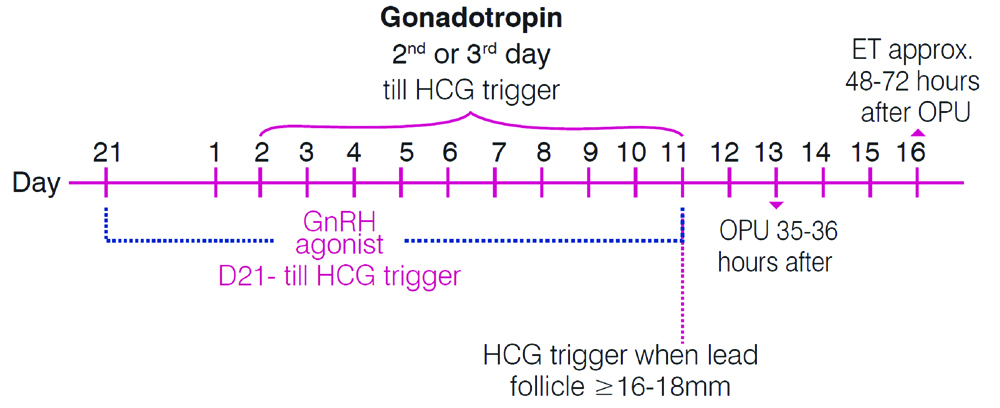
In this protocol as the name indicates agonist agents like triptorelin at a dose of 0.1 mg is started on the 21st day of the previous cycle. Gonadotropins are initiated at 150-225 International units (IU) daily either from the second or the third day of the subsequent cycle. Follicular growth helps in evaluating the dose adjustment of the gonadotropins. Both the GnRH agonist and the gonadotropins are continued till the size of the dominant follicle reaches 16-18 (mm). HCG injection is then administered for the final maturation and the trigger [Table/Fig-1] [6].
GnRH long agonist protocol; ET: Embryo transfer; OPU: Ovum pick-up.
Short Agonist Protocol
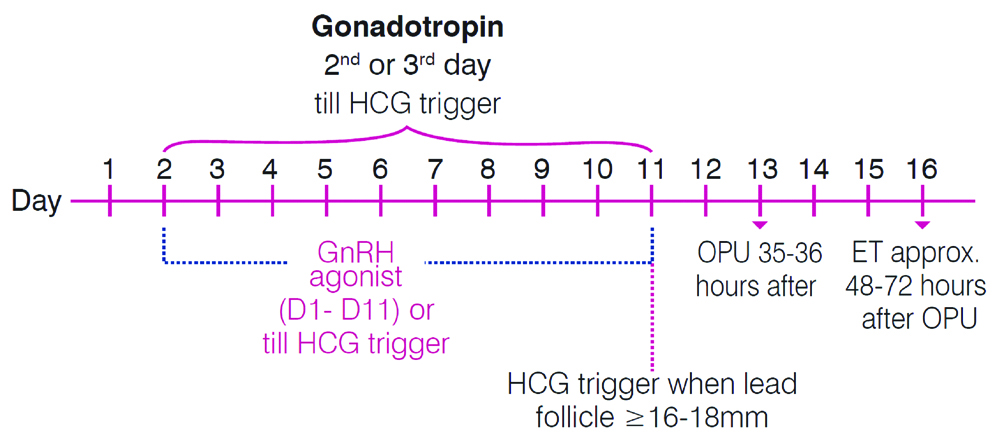
Micro-dose flare up agonist protocol [7]: This protocol is preferred in older women. A pretreatment of Oral Contraceptive Pills (OCPs) followed by a low dose of GnRH agonist (e.g., Leuprolide 40 μg twice a day) from day 2 of the withdrawal bleed till HCG trigger (or till the lead follicle reaches 16-18 mm) [Table/Fig-2].
Micro-dose flare up agonist protocol.
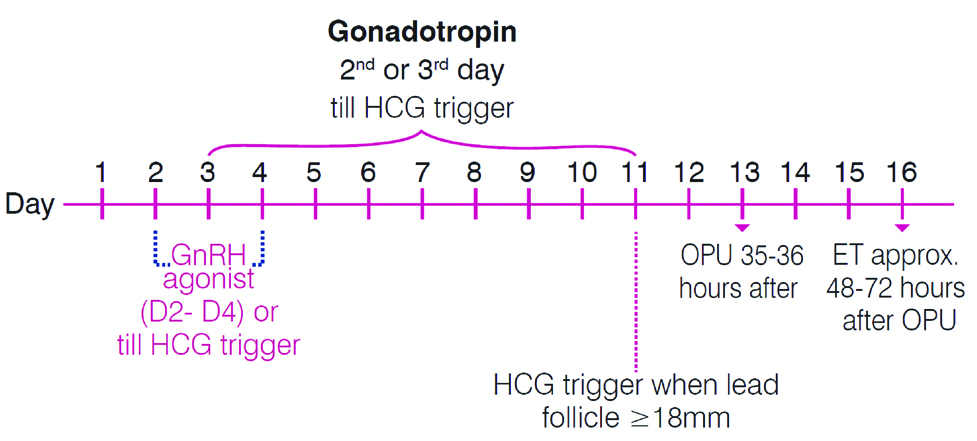
Ultra short agonist protocol [8]: In ultra-short treatment protocol GnRH agonist (e.g., buserelin) is administered on days 2, 3 and 4 of the stimulated cycles with gonadotropin being administered from day 2 or 3 till HCG trigger. Patients received 10000 IU HCG when at least two follicles that were ≥17-18 mm in diameter were observed by ultrasonography [Table/Fig-3].
Ultra short agonist protocol.
These are the protocols which are widely preferred today compared to the agonist protocols. Stimulation with gonadotropins is initiated on day 2 or 3 as done in the earlier mentioned protocols.
Single dose fixed [9]: This is also known as French protocol. Here a single dose of antagonist (e.g., Cetrorelix at a dose of 3 mg) [10] is administered on the sixth or seventh day of stimulation. Usually after administration, suppression of LH can be seen around four days by which criteria for trigger are satisfied. In cases where the criteria for trigger/final maturation is not met then a daily dose of antagonist can be administered accordingly.
Multiple dose [11]: This protocol is also known as Lubeck protocol. Gonadotropins (FSH or HMG) are administered from second or third day of the menstrual cycle and continued till the size of the lead follicle reaches to a diameter of 16-18 mm. GnRH antagonist like cetrorelix initiated in either of the two ways mentioned below.
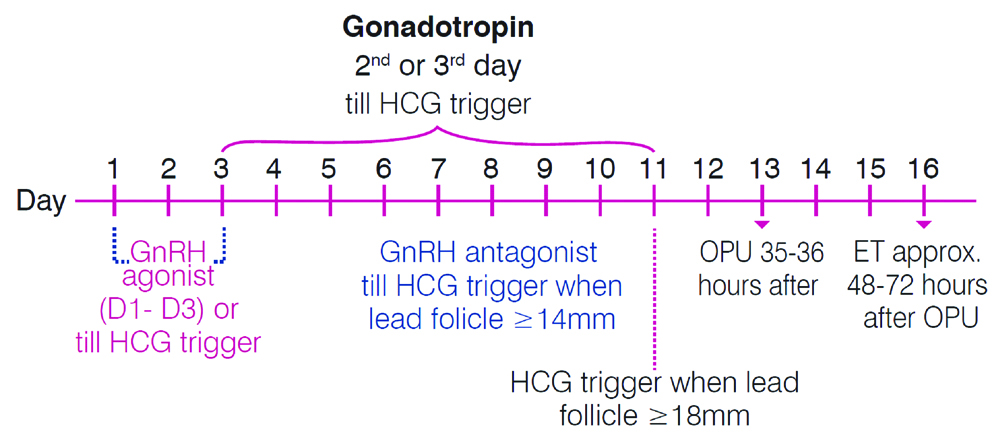
Flexible antagonist protocol: Here administration of cetrorelix at a dose of 0.25 mg daily is begun when the lead follicle reaches to a size of 14 mm and continued till the day of HCG trigger i.e., when the size of the lead follicle reaches to a diameter of 16-18 mm [Table/Fig-4].
Flexible/Fixed antagonist protocols.
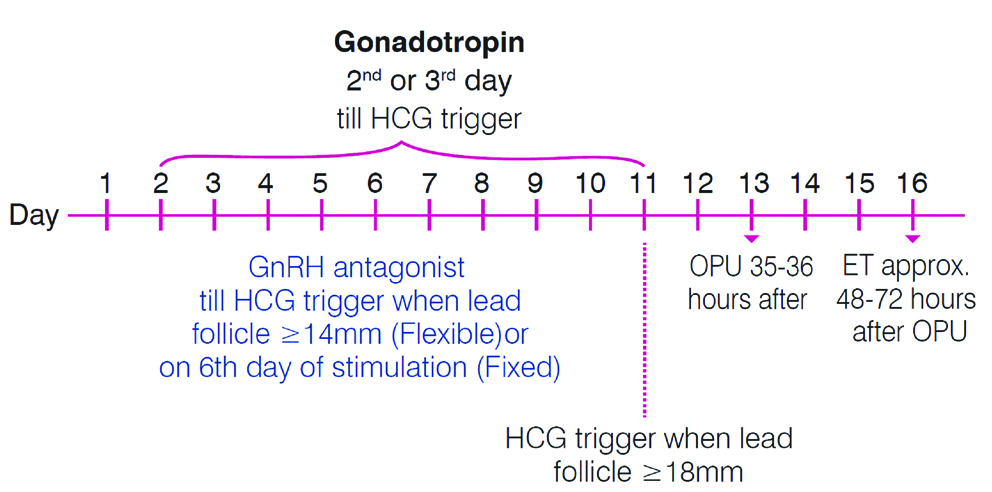
Fixed antagonist protocol: Here administration of cetrorelix at a dose of 0.25 mg daily is begun on sixth day of the gonadotropin stimulation (e.g., If FSH or HMG is initiated on the second day then on the seventh day single dose GnRH antagonist will be administered irrespective of the size of the follicle) [Table/Fig-4].
Combination of Two Protocols (Agonist+Antagonist Protocol) [
7]
In this protocol GnRH agonist (e.g., Buserelin at a dose 0.5 mg per day) is administered from the first day of the menstrual cycle, which is continued for three consecutive days. Gonadotropins (either FSH or HMG) are initiated on either the second or the third day of the cycle. GnRH antagonist like cetrorelix will be administered at a dose of 0.25 mg when the size or diameter of the dominant follicle reaches to 14 mm (similar to flexible protocol) [Table/Fig-5]. Cetrorelix administration is continued till the lead follicle reaches to 16-18 mm diameter. Once the size of the lead follicle reaches to a diameter of 16-18 mm then cetrorelix is discontinued and instead HCG injection is administered at a dose of 5000-1000 IU for causing maturation and trigger.
Ultra short agonist+flexible antagonist protocol.
Funding: This publication was supported by Emcure Pharmaceuticals Ltd.
[1]. Fertility: assessment and treatment for people with fertility problems. February 2013 NICE Clinical Guideline https://www.nice.org.uk/guidance/cg156/evidence/full-guideline-pdf-188539453. Accessed on 22/11/18 [Google Scholar]
[2]. Gallos ID, Eapen A, Price MJ, Sunkara SK, Macklon NS, Bhattacharya S, Controlled ovarian stimulation protocols for assisted reproduction: a network meta-analysisCochrane Database of Systematic Reviews 2017 3:CD01258610.1002/14651858.CD0125866473393 [Google Scholar] [CrossRef] [PubMed]
[3]. Siristatidis C, Salamalekis G, Dafopoulos K, Basios G, Vogiatzi P, Papantoniou N, Mild versus conventional ovarian stimulation for poor responders undergoing IVF/ICSIIn Vivo 2017 31(2):231-38.10.21873/invivo.1105028358705 [Google Scholar] [CrossRef] [PubMed]
[4]. Drakopoulos P, Blockeel C, Stoop D, Camus M, de Vos M, Tournaye H, Conventional ovarian stimulation and single embryo transfer for IVF/ICSI. How many oocytes do we need to maximize cumulative live birth rates after utilization of all fresh and frozen embryos?Hum Reprod 2016 31(2):370-76.10.1093/humrep/dev31626724797 [Google Scholar] [CrossRef] [PubMed]
[5]. Shrestha D, Xiaolin LA, Feng HL, Comparison of different stimulation protocols used in in vitro fertilization: a reviewAnn Transl Med 2015 3(10):137 [Google Scholar]
[6]. Palatnik A, Strawn E, Szabo A, Robb P, What is the optimal follicular size before triggering ovulation in intrauterine insemination cycles with clomiphene citrate or letrozole? An analysis of 988 cyclesFertil Steril 2012 97(5):1089-94.e1-3.10.1016/j.fertnstert.2012.02.01822459633 [Google Scholar] [CrossRef] [PubMed]
[7]. Eftekhar M, Mohammadian F, Yousefnejad F, Khani P, Microdose GnRH Agonist flare-up versus ultrashort gnrh agonist combined with fixed gnrh antagonist in poor responders of assisted reproductive techniques cyclesInt J Fertil Steril 2013 6(4):266-71. [Google Scholar]
[8]. Marcus SF, Brinsden PR, Macnamee M, Rainsbury PA, Elder KT, Edwards RG, Comparative trial between an ultra-short and long protocol of luteinizing hormone-releasing hormone agonist for ovarian stimulation in in-vitro fertilizationHum Reprod 1993 8(2):238-43.10.1093/oxfordjournals.humrep.a1380308473427 [Google Scholar] [CrossRef] [PubMed]
[9]. Tarlatzis BC, Fauser BC, Kolibianakis EM, Diedrich K, Rombauts L, Devroey P, GnRH antagonists in ovarian stimulation for IVFHuman Reproduction Update 2006 12(4):333-40.10.1093/humupd/dml00116567347 [Google Scholar] [CrossRef] [PubMed]
[10]. Olivennes F, Alvarez S, Bouchard P, Fanchin R, Salat-Baroux J, Frydman R, The use of a GnRH antagonist (Cetrorelix) in a single dose protocol in IVF-embryo transfer: a dose finding study of 3 versus 2 mgHum Reprod 1998 13(9):2411-14.10.1093/humrep/13.9.24119806259 [Google Scholar] [CrossRef] [PubMed]
[11]. http://www.fogsi.org/wp-content/uploads/2015/05/pdf/editor/dr_reshma_pai/7.pdf. Accessed on 13th Aug, 2018 [Google Scholar]