Chronic Non-Specific Low Back Pain (CNSLBP) is defined as pain located between the costal margin and buttocks and lasts for longer than three months while particular causes of low back pain are unknown, accounting for <15% of all back pain cases [1]. About 85% of patients with isolated LBP cannot be given a specific pathoanatomical diagnosis. NSLBP has been defined as tension, soreness, and/or stiffness in the lower back region for which it is impossible to recognise a specific cause of the pain [2]. The condition has a high incidence and prevalence which has been explored in various systematic studies. Reviews explored that the lifetime incidence of LBP was >70% and one-year prevalence ranges 15% to 45% with point prevalence averaging 30% [3].
Here is an effort to check the impact of spinal manipulation connected with CNSLBP on which a great number of management reports have been recommended by European guidelines for the management of CNSLBP [4]. These guidelines hold up the use of spinal manipulation with high-velocity low amplitude thrust in patients with chronic low back pain suggest that spinal manipulation is probably useful [5] and cost-effective when applied alone or in combination with other techniques compared to common practitioner care or universal physical therapy [4].
While mechanisms responsible for the therapeutic effects of Spinal Manipulation (SM) remains unclear for patients with non-specific low back pain, different theories and mechanisms of action for spinal manipulation are still under conversation [6]. Manual therapists, osteopaths, and chiropractors are significantly oriented by biomechanical and physiological mechanism where mechanical forces are applied to specific vertebral regions may modify segmental biomechanics by releasing trapped menisci lesions, reducing adhesions and distortions of the annulus fibrosus [5]. This mechanism of action enables the vertebral segments to progress in a bigger range of motion and would diminish the mechanical pressure on paraspinal muscles, thus reducing pain and distress. However, the mechanisms underlying the effects of SM appears to be more difficult than a simple biomechanical oriented model and explained between a combination of biomechanical and non biomechanical effects [7].
Patients with low back pain have altered postural sway compared to healthy persons. It is hypothesised that the reduced proprioceptive perception originated from muscle or joint mechanoreceptors can be a reason of changed postural sway [8] as well as impaired quick-fix memory that leads to detain in processing postural control information [9].
It is generally accepted that low back pain has a negative impact on quality of life [10]. The quality of life of patients with non specific low back pain is lower in comparison to general population and much lower with chronic condition. This seriously affects the functional ability and working status of young and adult population. While affecting quality of life and disability the intensity of pain with CNSLBP is complete individual, psychosocial and work-related [11]. In the current study, spinal manipulation has been used to impact proprioceptive input on spinal tissues to improve sensorimotor function. As a result, this study might give evidence to sensorimotor mechanisms that cause the experimental functional deficits associated with LBP as well as the mechanism of action of SM [12].
Exercise therapy is the basic treatment for chronic low back pain but most of the effective exercise approach is still under discussion. A recent evaluation suggests that separately designed supervised exercise programs including stretching or strengthening may result from more functional development and pain relief than supervise exercise in CNSLBP [13].
The present study aimed to evaluate efficacy of spinal manipulation on postural sway, pain sensitivity and quality of life among patients with CNSLBP.
Materials and Methods
This randomised controlled trial was conducted from August 2015 to January 2017 at Outpatient Department (OPD), Department of Physiotherapy, Lovely Professional University, India. All therapeutic interventions were provided within OPD, Department of Physiotherapy, Lovely Professional University. Ethical approval has been granted by Institutional Ethical Committee (Ref. No-LPU/IEC/PTY/004; Dt.16/11/16) and CTRI Regn. Ref. No: NCT03016676
Patients with Enrollment
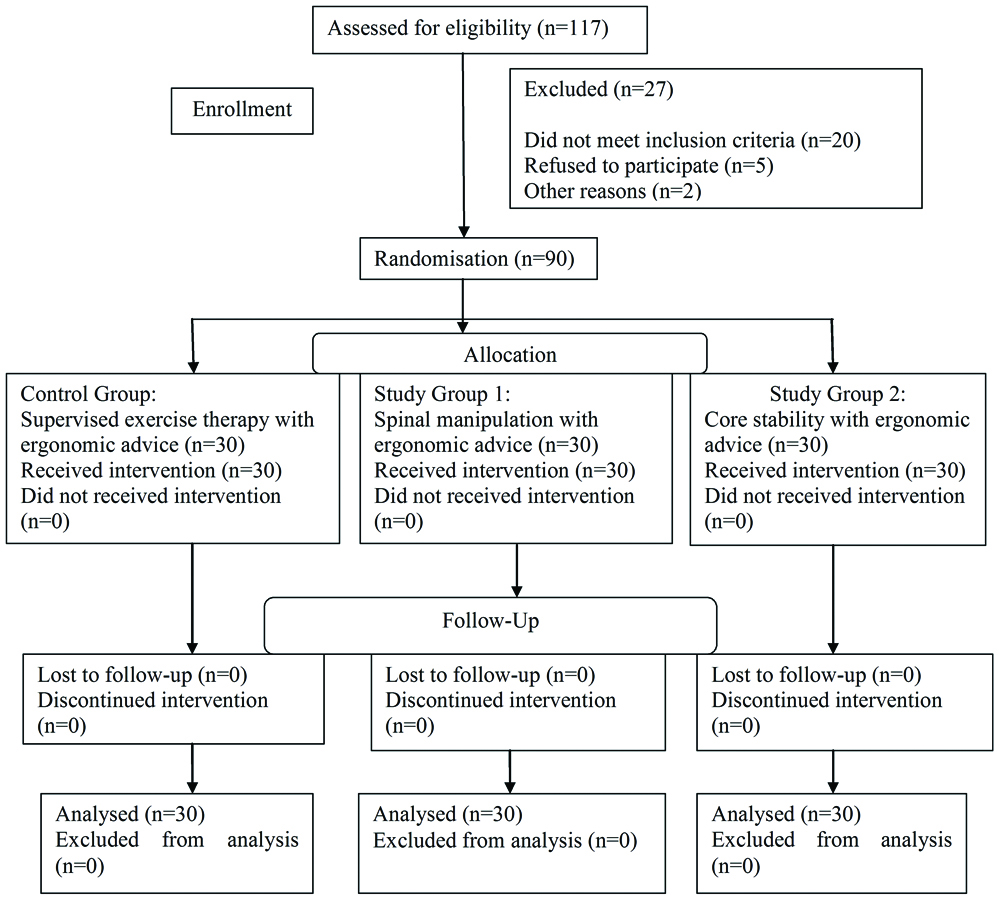
A consecutive convenient sample of 90 patients was recruited (out of 117 assessed for eligibility) from OPD, Department of Physiotherapy, Patients who participated in the trial were those suffered for more than three months with a history of CNSLBP, aged between 18-60 years, and less than three on 0 to 10 numeric pain rating scale. Participants were excluded if they have a baseline NPRS score [14] of less than three points, pain referred from the lumbar to lower extremities, serious spinal disorder, including malignancy, osteoporosis, ankylosing spondylitis, cauda equine compression and infection, previous spinal surgery, fracture of vertebrae, administered epidural injection.
Randomisation
All patients fulfilled inclusion/exclusion criteria and enrolled in the study after signing an informed consent document approved by the Institutional Ethical Committee. Restricted randomisation with a 1:1:1 allocation ratio has been applied using randomly block size and allocated in three groups. All participants fulfilled self-report and a physical examination. The following self-report questionnaires were fulfilled by patients at the baseline examination; demographic data (age, height, and weight), center of foot pressure (by Win Track platform) for postural sway, and pressure pain threshold (by digital algometer) for pain sensitivity, and EuroQol questionnaire [15] for health related quality of life. For self-report measures, the patients underwent a standardising historical and physical examinations (manual palpation of the lumbar and sacral areas to assess local tenderness of segmental dysfunction/hypomobility) which were replicated following achievement of two weeks treatment. Secret allotment of subjects was carried out with lacking perception of evaluators.
Intervention
The participants were assigned into three groups by consecutive convenient sampling, each group with 30 patients. All participants in the study received two weeks of treatment. The Control Group Supervised Exercise and Ergonomic Advice (SE+EA) had received supervised exercise with ergonomic advice alone; whereas Study Group 1 received spinal manipulation and ergonomic advice (SM+EA), and Study Group 2 received core stability exercise and ergonomic advice (CSE+EA) for 45 minutes per day for two weeks respectively.
Supervised Exercise and Ergonomic Advice (SE+EA)
The control group had received instruction for the supervised exercises with ergonomic advice (SE+EA) with 45 minutes sessions. Individualised sessions included advice and instruction on self-care measures, careful ergonomic recommendations for home and work, and demonstration of good lifting techniques. Simple stretching and strengthening exercises, including lumbar extension, bridging, and abdominal crunches, were demonstrated and practised. Participants were given a book and laminated cards describing these exercises and were encouraged to perform them at home on a daily basis [16]. The patients were followed-up in person two weeks later and then instructed to continue with the exercises on their own for the remainder of the intervention phase.
Spinal Manipulation and Ergonomic Advice (SM+EA)
The patients (n=30) of Study Group 1 received the protocol of spinal manipulation treatment in addition to ergonomic advice (described above). Spinal manipulation was delivered after a systematic physical examination that included manual palpation of the lumbar and sacral areas to assess local tenderness of segmental dysfunction/hypomobility to be manipulated. Spinal manipulation treatment technique for CNSLBP was generally performed on patients in a side-lying position on a treatment couch with the affected side facing upward. The therapists stood at the ventral aspect of the patient and held the upper spinous process of the affected segment with pulp of the thumb and the index finger as well as the spinous process of the lower vertebra of the affected segment with pulp and index finger of the other hand. Later, clinician held the arm of the patient and pulled it to create rotation and stopped as soon as the movement was perceived at the affected facet joints and applied the spinal manipulation (high velocity low amplitude thrust) by applying the force to the upper vertebra towards the couch and the lower vertebra away from the couch [17]. This thrust was often accompanied by an audible cracking or popping sound, which represents the creation and suspension of small gas bubbles within the joint cavity resulting from pressure, alters as the articular surfaces shortly split in response to the HVLA thrust [18].
Core Stability Exercises and Ergonomic Advice (CSE+EA)
The patients (n=30) of Group 2 received the protocol of core stability exercise in addition to ergonomic advice (described above). The protocol was delivered for duration of 45 minutes emphasising a high number of repetitions (two to three sets of 15 to 30 repetitions for each exercise) and progressive increase in muscle load. The patients were instructed to perform repetitions until they could no longer do so using proper form. For each exercise, the patients started at a level of difficulty that allowed them to complete a minimum of 15 repetitions at session. They then progressed to the next level of difficulty when they were able to perform the maximum 30 number of repetitions [19]. Core stability exercises were a plank, oblique plank, and hanuman. (1) Plank procedure was: i) presupposed a frontage sustain situation resting on subjects forearms with shoulders straight over the elbows; ii) set straight legs out behind and raised up hips to form a dead-straight line from shoulders to ankles. Subjects were balanced on forearms and toes, with lower abdomen and back working to keep the body straight. Holding was for one minute and 15 to 30 repetitions. (2) Oblique Plank: i) patient’s position was laying, balance on the right forearm with shoulder beyond the elbow; ii) with legs out directly to the left pelvis so that balance on forearm and feet. The patient’s body was in a direct line and feel the oblique muscles down the side trunk working to maintain the position; iii) hold times were for one minute and 15 to 30 repetitions then replicate on another side. 3) Hanuman: i) Position of the patients was balanced on the floor with hands and knees. Back was flat and hips were parallel to the floor; ii) elevated right arm out in front of subjects and elevated left leg out to maintain it directly; iii) hold time was for one minute and 15 to 30 repetitions than to be replicated on the other side.
Measurement of Centre of Foot Pressure (COFP)
The capability to maintain balance in an upright standing posture was supervised using a Win Track platform (Win-Track, company-Medicapteurs, n0-12k0022, Made in France), which measures the postural sway (i.e., the movement of the centre of foot pressure) in the anterior-posterior (X) and side-to-side (Y) directions. The subject stood quietly on either a solid platform (i.e., directly on the force plate) for a period of 30 seconds while blindfolded. The first 30 seconds of data were recorded at a sample rate of 1200 Hz using monitor data acquisition software (WinTrack Software) [20,21]. Stance positions; Each participant achieved stance positions with eyes open to allow for assessment of postural sway with and without visual input. The order of stance position testing was bipedal stance. For the eyes-open testing, participants were instructed to fix their vision on a large red dot placed at eye level about four meters in front of the force platform. All stance positions were assessed among participants in bare feet.
Pressure Pain Threshold (PPT)
The amount of pressure corresponding to a perception of pain has been measured by a digital pressure algometer (DA-112, Jagson scientific Industries, India). The device consists of a round probe (1 cm2) vertically to the patient’s skin and pressure was applied at a rate of 5 Newton/second. The patients were asked to say “stop” on the sensation of pressure or uneasiness feeling of pain. The mean of three trials was calculated and used for analysis. A 30-second resting period was allowed between each trial [22,23]. The reliability of digital algometer has been found to be high (ICC=0.93; 95%), confidence interval (CI: 0.89-0.96). PPT measured at lumbar levels L1 to L5 bilaterally.
Quality of Life
Health-related quality of life was measured by EuroQol questionnaire (EQ-5D-5L) a spacious established questionnaire which was tested before, after two weeks of intervention and after four weeks of follow-up after four weeks of intervention. The EQ-5D-5L evocative system comprises the following five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has five levels: no problems-1; slight problems-2; moderate problems-3; severe problems-4; extreme problems-5 [15].
Statistical Analysis
All statistical analyses were performed using SPSS software for Windows version 16.0. Significance was set at p≤0.05 for all analyses because authors were attempting to confirm an observation made in prior studies. Descriptive statistics were generated for continuous and categorical measures. Univariate analysis of variance (ANOVA) was performed followed by post-hoc Tukey’s multiple comparison test (SPSS version-16.0) to determine significant differences in Centre Of Foot Pressure (COFP) scores, PPT, and EuroQoL questionnaire scores between groups.
Results
In the current randomised controlled trial, there were 53 male and 37 female with a mean age of 24.20-years in Control Group (SE+EA), 25.10 years in Study Group 1 (SM+EA), and 24.93 years in Study Group 2 (CSE+EA). All groups were followed up at two and four weeks of intervention by comparing the scores of centre of foot pressure (WinTrac pre post reading), PPT (Algometer pre post reading), and quality of life (EuroQoL questionnaire pre post score). No attrition was reported [Table/Fig-1]. The demographic characteristics and the outcomes were alike at baseline [Table/Fig-2]. The study changeable followed a normal distribution (p<0.05). The statistical analysis of data comparisons of above scores of within and between the groups was carried out [Table/Fig-3].
Baseline measures of demographic with pain sensitivity, postural sway, and quality of life variables.
| Variables | SE+EA (n=30) | SM+EA (n=30) | SET+EA (n=30) | p-value |
|---|
| Age (years) | 24.20±6.78 | 25.10±7.75 | 24.93±8.46 | 0.891 |
| Height (cm) | 167.00±8.33 | 173.17±8.69 | 168.80±10.31 | 0.091 |
| Weight (kg) | 60.70±11.51 | 70.53±11.20 | 65.67±9.18 | 0.063 |
| Primary outcomes |
| Pain sensitivity (PPT) | 26.64±3.74 | 27.84±3.94 | 28.56±5.44 | 0.243 |
| Postural sway (COFP) | 661.48±32.78 | 666.78±56.92 | 679.48±75.07 | 0.464 |
| Secondary outcomes |
| Quality of life (EuroQoL Questionnaire) | 21.00±.98 | 21.20±1.19 | 21.20±1.03 | 0.349 |
COFP=Center of foot pressure, PPT=Pressure pain threshold, Quality of life assessed by EuroQoL Questionnaire; SE+EA (supervised exercise with ergonomic advice)=Control Group; SM+EA (spinal manipulation with ergonomic advice)=Study Group-1; CSE+EA (core stability exercise plus with ergonomic advice)=Study Group-2
Outcomes (Means and SDs) and effects of intervention (mean between-group differences, adjusted for baseline values, with 95% confidence intervals).
| Outcome | Control Group | Study Group 1 | Study Group 2 | Control group Vs Study group -1 | Control group Vs Study group -2 | Study group -1 Vs Study group -2 |
|---|
| Pain sensitivity (PPT) |
| Baseline | 26.64±3.74 | 27.84±3.94 | 28.56±5.44 | | | |
| Two weeks | 39.59±3.45 | 71.63±8.26 | 48.57±4.79 | -32.05 (-35.66, -28.44)p=0.001 | -8.98(-12.59,-5.37); p=0.03 | -23.07(-18.68, -17.46)p=0.02 |
| Four weeks | 39.57±4.53 | 75.78±9.24 | 51.72±5.46 | -36.19(-40.34,-32.06)p=0.001 | -12.15(-16.29,-8.01); p=0.01 | -24.05(-26.68,-19.91)p=0.01 |
| Postural sway (COFT) |
| Baseline | 661.48±32.78 | 666.78±56.92 | 679.48±75.07 | | | |
| Two weeks | 629.70±31.34 | 451.13±50.28 | 539.43±42.73 | 178.57 (145.71, 183.1)p=0.001 | 90.27 (64.30, 116.23); p=0.04 | 88.30 (62.33, 114.27)p=0.04 |
| Four weeks | 626.93±29.76 | 449.58±48.92 | 536.40±41.88 | 177.37 (152.15, 202.58)p=0.001 | 90.53 (65.31, 115.75); p=0.04 | 86.83 (61.62, 112.05)p=0.04 |
| Quality of life (EuroQoL Questionnaire) |
| Baseline | 21.00±.98 | 21.20±1.19 | 21.20±1.03 | | | |
| Two weeks | 16.57±.77 | 9.03±1.33 | 14.27±1.70 | 7.54 (6.72, 8.35)p=0.01 | 2.30 (1.49, 3.11)p=0.05 | 5.23 (4.42, 6.05); p=0.02 |
| Four weeks | 16.60±.49 | 8.03±.67 | 13.20±1.77 | 8.57 (7.87, 9.26); p=0.01 | 3.40 (2.70, 4.01); p=0.04 | 5.17 (4.47, 5.86)p=0.02 |
COFP=Center of foot pressure, PPT=Pressure pain threshold, Quality of life assessed by EuroQoL Questionnaire; Control Group = SE+EA (supervised exercise with ergonomic advice); Study Group-1=SM+EA (spinal manipulation with ergonomic advice); Study Group-2=CSE+EA (core stability exercise plus with ergonomic advice); p<0.05 for differences among groups
Post-hoc Tukey’s comparison analysis was carried out within control group, Study Group-1, and Study Group-2 at baseline, after two weeks of intervention and four weeks of follow-up. No significance has been found within group analysis. When comparisons of mean difference carried out within the groups on data of baseline, two weeks of intervention, and four weeks of follow-up, the Study Group-1 has shown significant improvement in PPT (p=0.001), centre of foot pressure (p=0.001) and quality of life (p=0.01) than Study Group 2 and Control Group after two weeks of intervention as well as four weeks of follow-up [Table/Fig-3].
Discussion
The spinal manipulation with ergonomic advice showed a greater improvement in postural sway (centre of foot pressure), pain sensitivity PPT, and quality of life compared to core stability exercise therapy with ergonomic advice, and supervised exercise with ergonomic advice after two weeks of treatment period and four weeks of follow-up.
The reduction of postural sway and pain sensitivity detected in this study may be due to spinal, supraspinal, or still nonspecific mechanisms that could mediate pain, as recommended by a theoretical model. This model advocates that a mechanical force from a SM begin a cascade of neurophysiological reply from both the peripheral and central nervous systems that would give upgrade explanation of clinical outcomes, such as postural away and pain sensitivity [24].
There were small, non-significant differences between the core stability exercises with ergonomic advice and supervise exercise with ergonomic advice groups. The group treated by spinal manipulation with ergonomic advice rated higher than that of supervised exercise with ergonomic advice at the end of treatment. This could be due to realignment of spinal structures regaining postural stability by increasing the capacity of stabilising system of spine to maintain the spinal neutral zones within physiological limits in order to prevent neurological deficit, major deformity and/or incapacitating pain [25].
A hypermobile spinal segment sometimes may predispose to recurrent derangements leading to chronic discodural involvements. Pain occurs due to instability of spinal segment as well as a fragment of the disc. Postural ligamentous pain appears when normal ligaments are subjected to abnormal mechanical stresses. This may occur all through the disturbance phase; some lack of turgor inside the disc and the lower in the inter-vertebral joint area motive a few laxities of the section and growth of the impartial zone. The facet joints trample upon, with the upper articular process sliping over the lower. The joints get extended and the posterior capsules gain overstretched leading to malpostural ligamentous pain [26].
In the present study, the PPT has been effectively reduced by spinal manipulation. This could be due to active stabilisation of the unstable segment and segmental control of the spine and increased distance between the two vertebral borders gives the fragment space to move and the force exerted by the posterior ligament pushes it back in place thereby improves the quality of life [14]. Recent findings claim that overall non specific chronic low back pain can be relieved by eight spinal manipulation sessions in between 46% and 57% of patients [27,28].
There is high-class procedural evidence to sustain the use of spinal manipulation in management of patients with CNSLBP. The intervention is also recommended by clinical practice guidelines for management of low back pain [4] and additional musculoskeletal disorders [29]. In this study, both groups had better improvement of postural sway and pain sensitivity from baseline to post treatment of two weeks. According to evidence-based clinical guidelines, both spinal manipulation and core stability are effective treatment options for CNSLBP [26]. Regarding spinal manipulation, little is known about optimal dosage and, to date, provider type (e.g., chiropractor, osteopath, or physical therapist) has not been related with any differential effect [30].
In the present study, only 6.85% of patients reported “No Problems at all” and as many as 93.3% of patients reported a moderate problem on at least one dimension of EQ-5D. This indicates that patients with non specific chronic low back pain have lower quality of life than the general population as well as the parameter defining the quality of life of patients with non specific chronic low back pain is a combination of physical and psychological problems as seen in study of Antonopoulou MD et al., [31].
Spinal manipulation, when applied to the joints and surrounding musculature, might alter afferent feedback to the central nervous system to increase proprioception, improve motor control and thereby improve postural sway. Manual therapy techniques have been seen to alter short-term motor neuron activity, enhance performance in proprioception dependant activities, increase range of motion, alter markers of autonomic nervous system activity, and facilitate an immediate increase in mean voluntary contraction of the paraspinal muscles [26,32]. It has been hypothesised that through these mechanisms spinal manipulation may influence postural sway [33,34]. Only a limited number of interventions for CNSLBP have been assessed in clinical trials; as a result, there is no recognised gold standard treatment. Authors chose exercise therapy an intervention because of the support of efficiency for adults with LBP [35].
Limitation and Strength
The study was limited to 90 subjects of 18-60 years of age. All prospective care was taken to make sure that the present study with a low risk of bias by including sufficient randomised trial, secret allotment, lacking perception of evaluators, comparison at baseline, calculation of sample size and purpose-to-treat analysis. Lacking perception of the evaluators was established by the truth that the evaluators were unable to estimate which patient was devoted to ergonomic advice. In differentiation, it was unobtainable to blind the clinician or the patients because of the nature of the interventions, which does not remove the risk of bias. Therefore, lack of blinding of the clinicians or patients could be elucidating as a limitation of this study. There has been no achievable impact of long term follow-up as an additional limitation.
Conclusion
The spinal manipulation has been effective on chronic non specific low back pain. Awareness of this therapeutic needs time to become popular among clinicians as well as clients.
COFP=Center of foot pressure, PPT=Pressure pain threshold, Quality of life assessed by EuroQoL Questionnaire; SE+EA (supervised exercise with ergonomic advice)=Control Group; SM+EA (spinal manipulation with ergonomic advice)=Study Group-1; CSE+EA (core stability exercise plus with ergonomic advice)=Study Group-2
COFP=Center of foot pressure, PPT=Pressure pain threshold, Quality of life assessed by EuroQoL Questionnaire; Control Group = SE+EA (supervised exercise with ergonomic advice); Study Group-1=SM+EA (spinal manipulation with ergonomic advice); Study Group-2=CSE+EA (core stability exercise plus with ergonomic advice); p<0.05 for differences among groups