Oesophageal Schwannoma: A Postoperative Diagnosis
Aditya Sharma1, Hirdaya Hulas Nag2, Phani Kumar Nekarakanti3, Vidya Sharada Bhat4, Monika Sharma5
1 Senior Resident, Department of Gastro Surgery, GB Pant Hospital, Delhi, India.
2 Professor, Department of Gastro Surgery, GB Pant Hospital, Delhi, India.
3 Senior Resident, Department of Gastro Surgery, GB Pant Hospital, Delhi, India.
4 Senior Resident, Department of Gastro Surgery, GB Pant Hospital, Delhi, India.
5 Senior Resident, Department of Pathology, GB Pant Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hirdaya Hulas Nag, Professor, Department of Gastro Surgery, GB Pant Hospital, Delhi, India.
E-mail: hirdayanag@gmail.com
Oesophageal schwannomas are rare benign tumours with very few case reports in the literature. It is very difficult to diagnose these tumours preoperatively and is often confused with other benign tumours like leiomyomas and GIST. Hereby, a case of 42-year-old male is described who presented to us with the complaint of progressive dysphagia for the past two and a half year that posed a challenge regarding preoperative diagnosis. The patient was operated on the lines of oesophageal leiomyoma, later on which histopathology came out to be schwannoma.
Dysphagia, Oesophageal leiomyoma, Oesophageal tumour
Case Report
A 42-year-old male patient presented to the Department of Gastro Surgery with a complaint of progressive dysphagia for the past two and a half year.
The patient was a known smoker for 30 years. The patient had chronic obstructive pulmonary disease and was on treatment. There were no significant findings on physical examination.
Oesophageal barium study showed an eccentric compression in mid oesophagus suggestive of submucosal lesion.
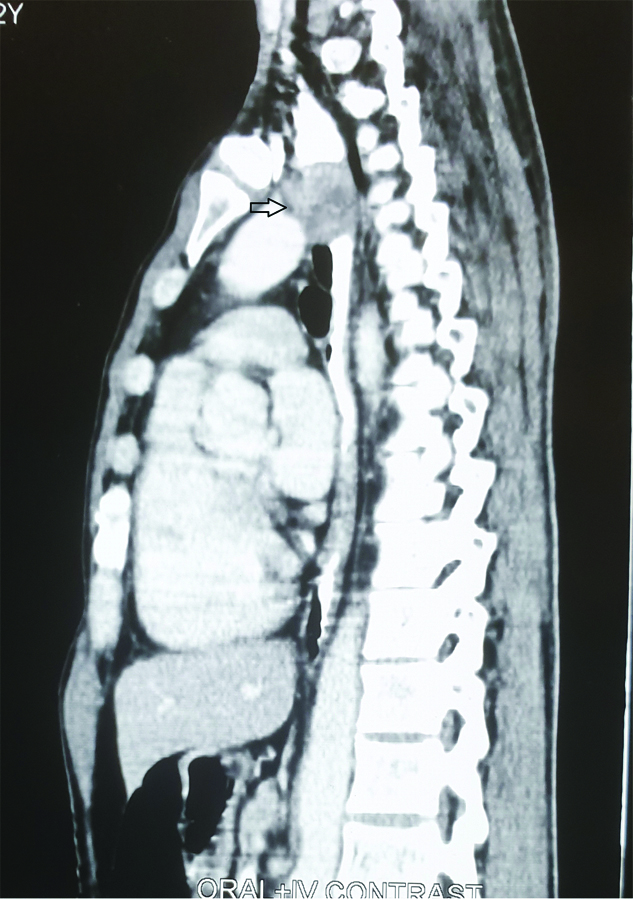
On Upper GI endoscopy, smooth mucosal bulge was seen from 24 to 27 cm with luminal compromise, however the scope was negotiable beyond the lesion. On CECT chest, a well-defined (28×18 mm) eccentric submucosal heterogenously enhancing soft tissue lesion was seen along the left lateral wall at the level of D3-D4 vertebrae with proximal hold up of oral contrast [Table/Fig-1,2].
Axial cut of the CECT showing the heterogeneously enhancing lesion adjacent to trachea.
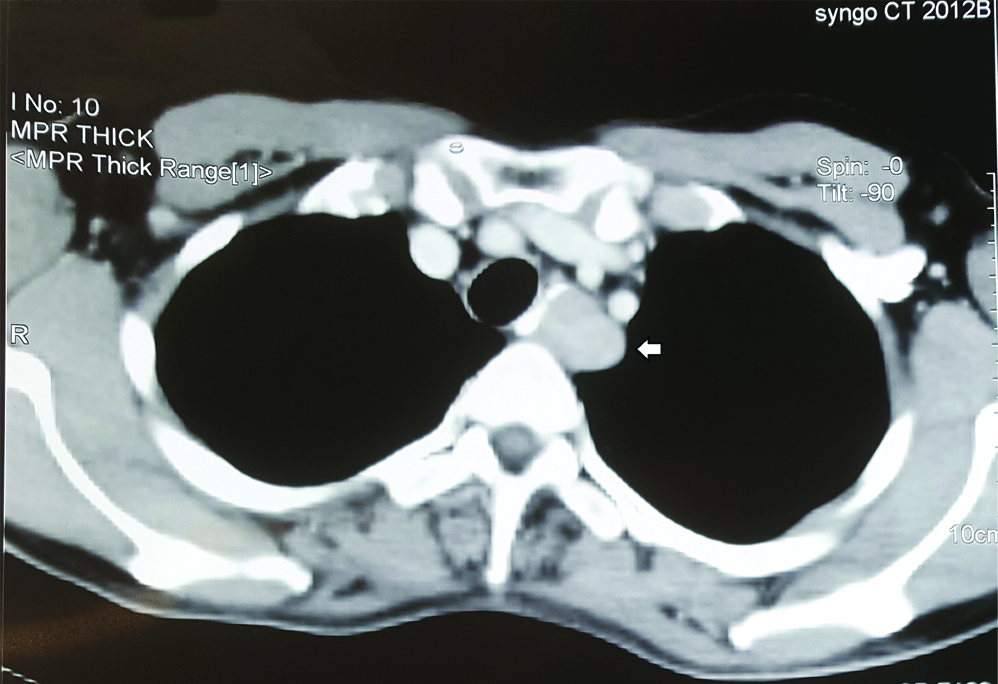
Figure showing heterogenously enhancing lesion at the level of D3-D4.
The lesion was seen to be arising from fourth layer of oesophagus with increased vascularity on Endoscopic ultrasound. Endoscopic ultrasound guided FNAC of the lesion was done. The report showed spindle cells suggestive of leiomyoma but with possible malignant degeneration.
After optimising his chest condition, the patient was taken up for thoracoscopic enucleation of the tumour with preoperative diagnosis of oesophageal leiomyoma. He was placed in left lateral position and thoracoscopic enucleation was attempted. However, thoracotomy was done as the tumour was 2 cm proximal to the carina, located more towards the left side and safe dissection was difficult and risky. While in the same position a thoracotomy incision was given in the right fifth intercostal space. The oesophagus was minimally mobilised around the tumour. The adventitia, longitudinal and circular muscular layers were incised over the lesion. A 3×3 cm pearly white tumour was enucleated. The mucosal integrity was confirmed and remaining outer layers were closed with 3-0 vicryl (polygalactin). Postoperative course was uneventful.
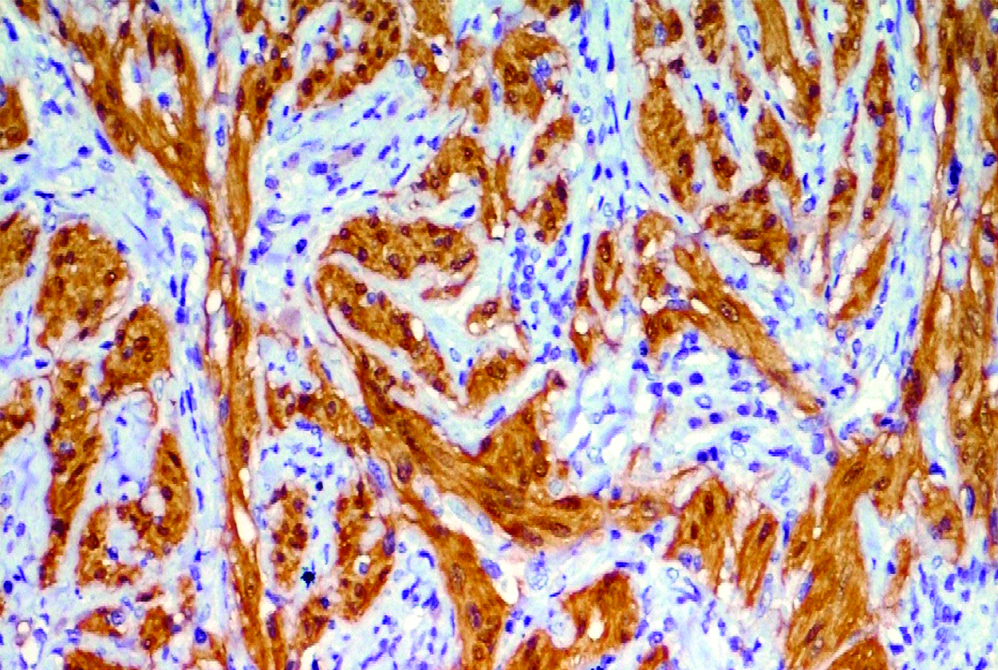
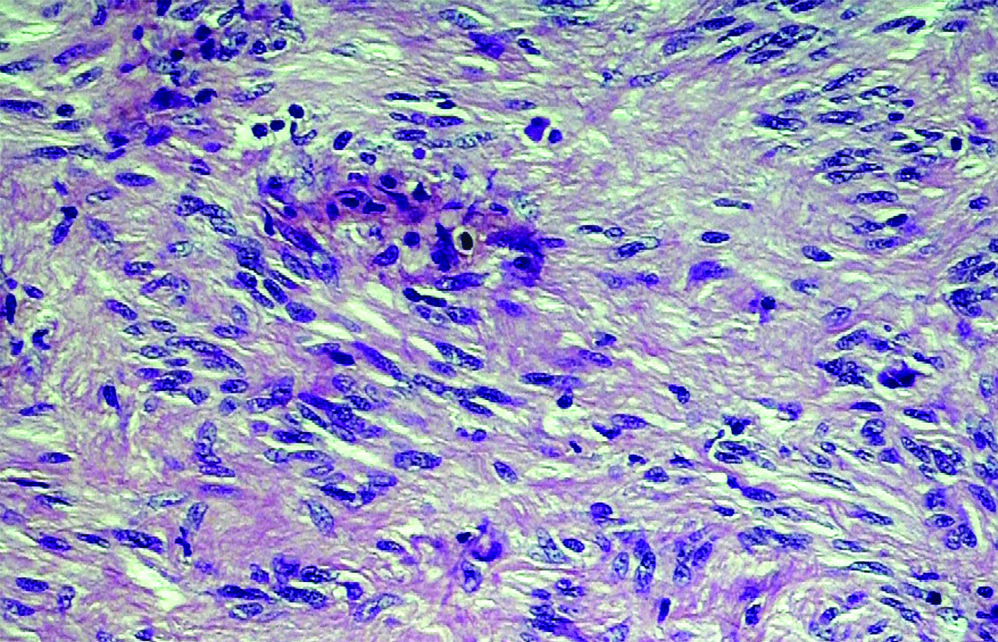
On histopathological examination, it was diagnosed as Schwannoma. The eosin-haematoxylin staining of the multiple sections of the tumour showed presence of spindle cell tumour arranged in intersecting fascicles and at places forming the hypercellular and hypocellular areas. In the hypercellular areas the tumour cells showed nuclear palisading with no significant mitosis and necrosis. On IHC, the tumour cells were strongly positive for S-100 and negative for CK [Table/Fig-3,4].
Figure showing tumour cells with strong s-100 positivity (x100).
Tumour cells showing nuclear palisading without mitosis and necrosis H and E staining (x100).
Discussion
Benign oesophageal tumours are rare and account for around 2% of all the oesophageal tumours. Most common of them are leiomyomas while schwannoma and GIST are very uncommon [1], malignant oesophageal schwannoma are even more rarer [1]. Most of the patients with oesophageal schwannoma present between 40-60 years of age with a female to male ratio of 4.1:1. Of the 25 reported cases reviewed by Kassis ES et al., sixteen cases were from Asian institutions. Most of the patients present with the complaints of dysphagia although they can present with the complaints of dyspnea too. Rare presentation can include chest pain, cough, pain in epigastrium and palpable neck mass [2]. Preoperative diagnosis of primary oesophageal schwannoma is often very difficult. Most of the times, an initial diagnosis of leiomyoma or GIST is made [2]. Preoperative investigations include upper GIendoscopy which shows eccentric bulge in the oesophageal lumen with normal overlying mucosa. Endoscopy is followed by CECT. On CT the lesion is usually well-defined and heterogenous in attenuation which may or may not show enhancement. It is very difficult to distinguish it from oesophageal leiomyoma. Endoscopic ultrasound guided FNA although very useful but is not able to detect oesophageal schwannomas every time, as true in present case too [3].
There are three surgical approaches for oesophageal schwannoma consisting of oesophagectomy, local resection and enucleation. The operative approach depends on various factors like tumour location, size and patient condition. Oesophagectomy is a radical approach and is associated with many complications such as recurrent laryngeal nerve paralysis, pulmonary dysfunction or chylothorax [4]. Local resection is preferred to radical approach, oesophagectomy, with minimal morbidity and equivalent results [5]. The location and origin of Schwannoma outside the mucosal layer makes enucleation a better approach but enucleation of very large tumours is associated with higher rates of oesophageal strictures [6].
In most of the reported cases a definitive diagnosis was made only after resection of the tumour. Microscopic appearance of these tumours included palisading spindle cells, very few mitotic figures and no necrosis as shown in this case too [7,8]. As schwann cells are strongly positive for S-100, oesophageal schwannoma is diagnosed by strong S-100 positivity and CK negative nature on IHC [2].
Conclusion
Oesophageal schwannoma is a rare benign tumour of the oesophagus which poses diagnostic difficulties preoperatively. Most of the cases are diagnosed postoperatively with tumour cells showing strong S-100 positivity.
[1]. Wang S, Zheng J, Ruan Z, Huang H, Yang Z, Zheng J, Long-term survival in a rare case of malignant esophageal schwannoma cured by surgical excision.Ann Thorac Surg 2011 92(1):357-58.10.1016/j.athoracsur.2011.01.04521718879 [Google Scholar] [CrossRef] [PubMed]
[2]. Kassis ES, Bansal S, Perrino C, Walker JP, Hitchcock C, Ross P, Giant asymptomatic primary esophageal schwannomaAnn Thorac Surg 2012 93(4):e81-e83.10.1016/j.athoracsur.2011.10.05422450109 [Google Scholar] [CrossRef] [PubMed]
[3]. Kitada M, Matsuda Y, Hayashi S, Ishibashi K, Oikawa K, Miyokawa N, Esophageal schwannoma: a case reportWorld J Surg Oncol [Internet] 2013 11:25310.1186/1477-7819-11-25324088647 [Google Scholar] [CrossRef] [PubMed]
[4]. Akaogi E, Mitsui K, Sohara Y, Endo S, Ishikawa S, Hori M, Treatment of postoperative chylothorax with intrapleural fibrin glueAnn Thorac Surg 1989 48(1):116-18.10.1016/0003-4975(89)90193-8 [Google Scholar] [CrossRef]
[5]. Asteriou C, Konstantinou D, Lalountas M, Kleontas A, Setzis K, Zafiriou G, Nine years experience in surgical approach of leiomyomatosis of esophagusWorld J Surg Oncol 2009 7:10210.1186/1477-7819-7-10220030817 [Google Scholar] [CrossRef] [PubMed]
[6]. Shien K, Nozaki I, Kobatake N, Ohta K, Kubo Y, Tanada M, Two case reports of esophageal schwannoma and literature review of case reportsJpn J Gastroenterol Surg 2010 43:1106-11.10.5833/jjgs.43.1106 [Google Scholar] [CrossRef]
[7]. Zhang W, Xue X, Zhou Q, Benign esophageal schwannomaSouth Med J 2008 101:450-51.10.1097/SMJ.0b013e3181683fd818391742 [Google Scholar] [CrossRef] [PubMed]
[8]. Matsuki A, Kosugi S, Kanda T, Komukai S, Ohashi M, Umezu H, Schwannoma of the esophagus: a case exhibiting high 18F-fluorodeoxyglucose uptake in positron emission tomography imagingDis Esophagus 2009 22(4):E6-E10.10.1111/j.1442-2050.2007.00712.x19473209 [Google Scholar] [CrossRef] [PubMed]