Incidence of SAM, which is one of the major factors contributing to infant and under five mortality, is approximately 6.4% [1]. The number of under-five children in India suffering from SAM is, therefore, a staggering 80 lakh children. It is not possible to admit so many children in paediatric wards because India does not have sufficient hospital beds for offering inpatient care to all SAM children. Therefore, only children of SAM with complications are admitted. These children have to be discharged from the hospital after 2-3 weeks of hospitalisation after 15% weight gain from his original admission weight [2]. Their remaining recovery has to take place at home. It has been reported that the rate of weight gain at home is less than satisfactory (<5 g/kg/day) [3,4]. In Africa, Ready to Use Therapeutic Food (RUTF) which is a lipid-based formula with milk powder, electrolytes, micronutrients and offer same nutrients as F-100 has been used with remarkable success for home-based management of SAM patients [5]. According to WHO guidelines for management of SAM patients in NRC [2], LTF is used along with F-100-a Milk formula with high protein-energy content is used in rehabilitation phase of SAM. Earlier F-75 is given in stabilisation phase, during hospitalisation for nutritional rehabilitation of severely malnourished children [2]. However, no special diet is given after discharge for home-based management after discharge. So, it is desirable to introduce a diet which is cost-effective and also effective for weight gain for post discharge nutritional rehabilitation of SAM children. Government of India/UNICEF guidelines recommends use of LTF children at Village Child Nutrition Centre (VCNC), at Anganwadi level to SAM children without complications [2]. This LTF (non-milk based) has a longer shelf life since it does not contain milk powder.
Milk-based LTF has been recommended by Government of India /NRHM Guidelines (2012). For inpatient treatment of SAM during admission in NRC [2]. This diet has been used in a study in Goverment Medical College, Baroda, for treatment of SAM patients after discharge with significantly improved growth rate. One major limiting factor however, was that it needed weekly instead of fortnightly follow-up since it (Milk-based LTF) gets rancid after 8-10 days on account of containing milk powder. Present study was therefore planned to see if non-milk based LTF can provide a sufficient rate of weight gain in post discharge period.
Materials and Methods
The present study was a Randomised Clinical Trial conducted in Nutritional Rehabilitation Centre of Sir Sayaji General Hospital (SSGH), Vadodara, Gujarat, India. Study was conducted between February 2016 and September 2016. Permission to conduct the trial was obtained from Institutional Ethics Committee (IEC) and Scientific Review Committee (SRC) before it was started. (Registration No: ECR/85/inst/Gj/2013). Based on a previous study (in Press) conducted in our department, It was decided to enrol patients over a period of at least six months and to enrol at least 60 patients (30 in each arm), however, authors could enrol a total of 80 patients (40 in each arm).
Authors enrolled children having SAM of age group six months to five years who were discharged from NRC of the present Institute (Goverment Medical College, Baroda). Authors excluded children with history suggestive of allergy against peanut protein, those who were likely to leave study within next few months and those having underlying major chronic systemic illness like congenital heart disease or CNS malformations.
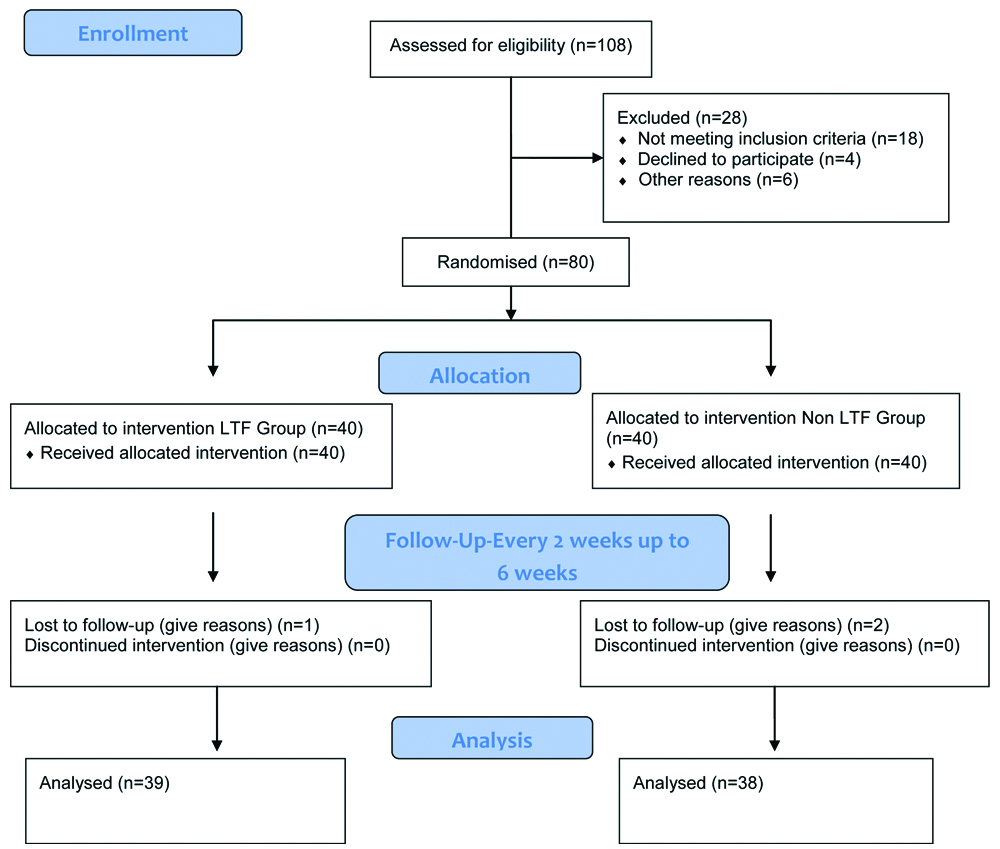
Patients were enrolled after obtaining valid informed consent. The [Table/Fig-1] shows the study flowchart. In this study a total of 80 SAM children were enrolled after discharge from NRC. These children were followed-up for total six weeks after discharge. After discharge from NRC after receiving initial nutritional rehabilitation as per Indian Academy of Paediatrics management guidelines [6], SAM children were divided into two groups.
First group: Those patients who were discharged in March, May, July and September were given non-milk based LTF (Composition as per [Table/Fig-2]) after discharge and on every follow-up (total three follow-ups every two weeks to be consumed at home along with home-based diet.
Composition of non-milk based Local Theraputic Feed (LTF).
| Ingredient | Quantity (grams) | Kcal | Protein (grams) | Fat (grams) |
|---|
| Wheat flour | 30 | 102 | 3.63 | 0.51 |
| Groundnut | 60 | 342 | 15.7 | 23.8 |
| Sugar | 30 | 119 | 0.03 | 0 |
| Oil | 30 | 270 | 0 | 30 |
| Total | 150 | 833 | 19.36 | 54.3 |
Second group: Those patients who were discharged in the months of February, April, June, August, did not receive LTF. They were discharged only with advice on home-based diet like Khichdi, Milk, Daal, Rice, Roti and cooked vegetables, Upama and Seasonal fruits according to Infant and young child feeding guidelines [7]. Weight gain, MUAC, Height and weight for height is compared between these two groups on three follow-ups carried out every two weeks after discharge.
At the time of discharge, this LTF was given to children according to their weight in Ziplocked plastic pouches to be consumed at their home along with home-based diet and multivitamin and mineral supplements. Total amount recommended was as per [Table/Fig-3] divided into three or more feeds. Parents were explained about the advantages of giving this LTF to their child at home. Parents were asked to bring empty pouches back on follow-up to ensure the compliance.
Amount of LTF to be consumed at home after discharge [2].
| Weight of child | Amount of LTF given per Day |
|---|
| 3-4.9 kg | 100-130 g/day |
| 5-6.9 kg | 200-250 g/day |
| 7-9.9 kg | 250-400 g/day |
| >10 kg | 400-450 g/day |
LTF preparation was carried out by “ANNAPOORNESHWARI” trust in collaboration with Department of Paediatrics. Non-milk based LTF was prepared according to State Nutrition mission guidelines for Mission Balam Sukham, Health and family Welfare, ICDS [8].
Statistical Analysis
The data were entered into Microsoft excel sheet and data were checked for accuracy. Data were analysed by applying unpaired t-test using MEDCAL C software (version 12.5.0). The p-value of <0.05 was considered significant.
Results
A total of 80 cases were included in the study as per inclusion and exclusion criteria. Out of these, 40 patients were provided LTF along with home-based diet after discharge and 40 were discharged only on home-based diet. Patients were followed-up every two weeks for six weeks (total of three follow-ups). A baseline characteristic of the study subjects has been described in [Table/Fig-4]. Among 80 patients, maximum numbers of patients were in age group 6-12 months (total of 42 patients). In age group 13-24 months there were 30 patients and in >24 months age group there were eight patients. Among 80 patients 42 were male and 38 were females (1.1:1). There was not much significant difference found between prevalence of SAM in male and female. In this study, patients were more or less evenly distributed between rural and urban areas, while 13.7% of patients were from the tribal areas.
Baseline characteristics.
| Variables | Milk Based LTF group n=39 mean (±SD) | Non LTF group n=38 mean (±SD) |
|---|
| Male | 22 | 18 |
| Female | 17 | 20 |
| Lost follow-up | 01 | 02 |
| Age in months | 14.15 (6.99) | 17.08 (10.11) |
| Weight (kg) | 6.2 (1.25) | 6.93 (1.18) |
| Height (cm) | 69.08 (7.18) | 72.55 (7.63) |
| Wt/Ht % | 77.43 (6.38) | 79.32 (5.39) |
| Wt/age % | 73.85 (9.35) | 77.25 (8.21) |
| Ht/age % | 90.63 (7.22) | 91.81 (5.94) |
| MUAC (cm) | 11.20 | 11.50 |
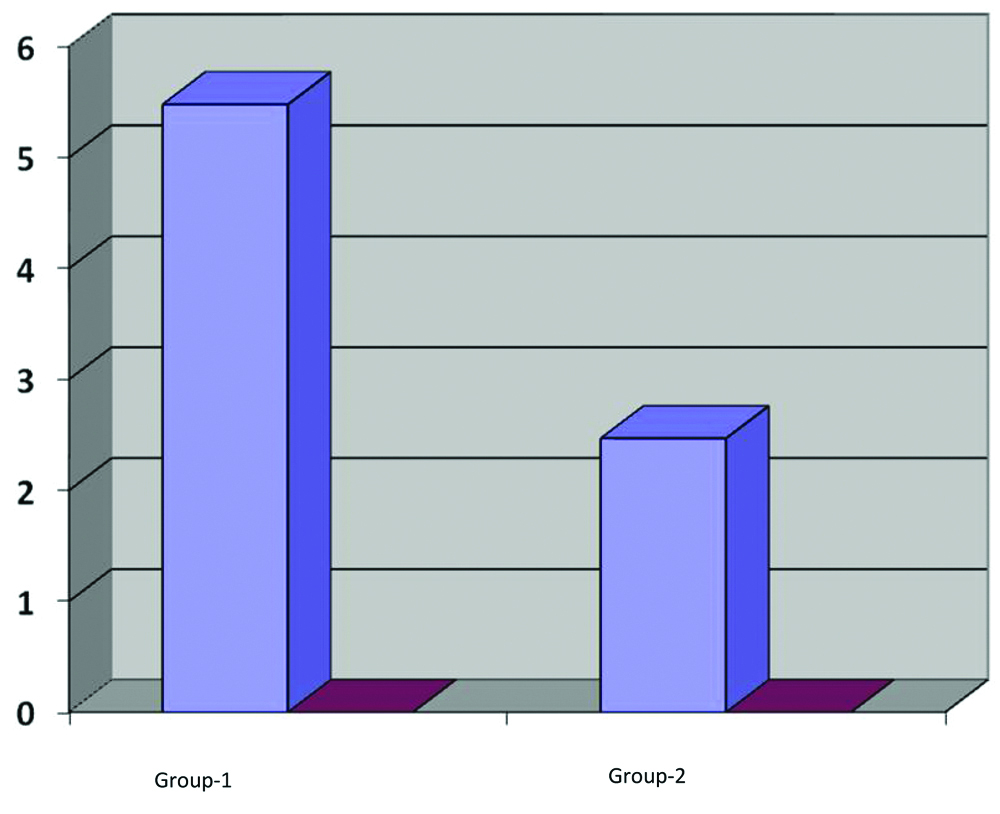
This study shows that rate of weight gain in group receiving LTF with home-based diet was 5.48±0.55 g/kg/day. While in those receiving only home-based diet, rate of weight gain was 2.47±0.36 g/kg/day [Table/Fig-5]. Significant difference of weight gain was observed in those receiving LTF with home-based diet. The findings of this study show an average height gain of 1.59±0.72 cm during the six week period of study in intervention group compared to 1.08±0.54 cm in control group. This study was conducted over a six week period and mainly addressed the problem of acute malnutrition. Height, on the other hand, was a measure of chronic malnutrition. It was therefore not expected to affect the height of the child much. Still, the findings suggest that the height gain in intervention group was significantly more than the height gain in control group (p=0.0007). Moreover, it was nearly in concordance with the expected height gain in normal children over a six week period during that age.
Comparison of weight gain (g/kg/day) between group 1 and group 2.
X-axis-patient groups, Y-axis-weight gain in g/kg/day.
In group 1 mean weight gain was 5.48 g/kg/day (SD 0.55), while in group 2 it was 2.47 g/kg/day (SD 0.36) with a p-value of <0.0001.
The findings of MUAC are depicted in [Table/Fig-6]. A 57.5% of patients in group 1(LTF+Home-based diet) had MUAC<11.5 cm to begin with. At the end of six weeks period none had MUAC<11.5 cm. Majority in fact (53.48%) had even crossed 12.5 cm. In comparison in Group 2 (only home-based diet) 28.94% were still severely wasted (MUAC<11.5 cm) while majority (65.78%) still were moderately wasted. (MUAC 11.5-12.5 cm).
Mid-upper arm circumference comparison.
| MUAC | Group-1 | Group-2 |
|---|
| Total number of patients on discharge (40) (%) | Total number of patients after 3 follow-up (39) (%) | Total number of patients on discharge (40) (%) | Total number of patients after 3 follow-up (38) (%) |
|---|
| <11.5 cm | 23 (57.5%) | 0 (0) | 13 (32.5%) | 11 (28.94%) |
| 11.5-12.5 cm | 17 (42.5%) | 18 (46.15%) | 25 (62.5%) | 25 (65.78%) |
| >12.5 | 0 (0) | 21 (53.84%) | 2 (5 %) | 2 (5.28%) |
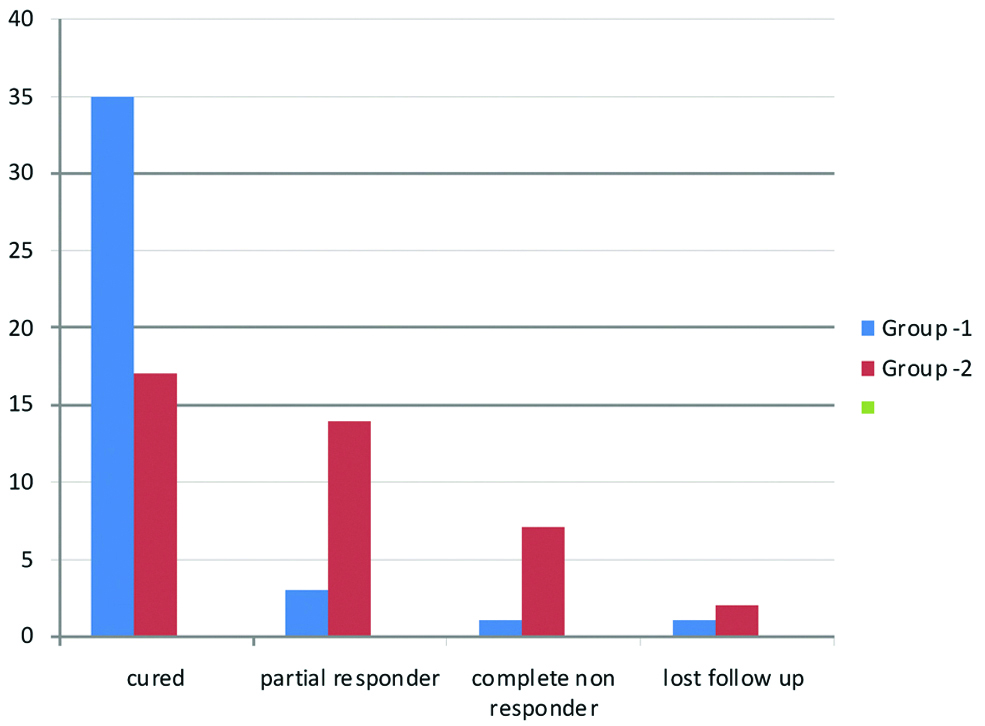
The [Table/Fig-7] shows distribution of both groups as per weight for height criteria. After three follow-ups (six weeks) 89.74% had crossed -2SD weight for height in Group 1 compared to 44.73% in Group 2. The [Table/Fig-8] depicts outcome comparison between the two groups. X-axis denotes outcome in both groups as explained in the figure. Y-axis shows no. of patients in each category. Recovery rates were significantly higher (35 out of 40 i.e., 87.5%) in LTF group compared to non-LTF group (17 out of 40 i.e., 42.5%) (p=0.049). A large number of patients in non-LTF group remained either severely or moderately wasted at the end of six weeks.
Weights for height comparison between two groups.
| Weight for height | Group-1 | Group-2 |
|---|
| On discharge (%) | After 3 follow-ups (%) | On discharge (%) | After 3 follow-ups (%) |
|---|
| <-3SD | 21 (52.5%) | 1 (2.56%) | 17 (42.5%) | 7 (18.43%) |
| -3SD to -2SD | 14 (35%) | 3 (7.69%) | 17(42.5%) | 14 (36.84%) |
| >-2SD | 05 (12.5%) | 35 (89.74%) | 6 (6%) | 17 (44.73%) |
Outcome comparison.
X-axis-categories of patients, y-axis-number of patients
Categories-*Cured=Patients who are having weight/height >-2Sd after 3 follow-ups
**Partially responders=Patients who have achieved their target weight but still having weight/height between -2SD and -3SD after 3 follow-ups
***Completely non responders Patients who are still having weight/height <-3SD after 3 follow-ups
****Defaulter=patients who have interrupted treatment in between follow-ups are considered as defaulter
Discussion
Severe acute malnutrition is a preventable and treatable cause of childhood morbidity and mortality. According to guidelines for management of SAM by Government of India, Milk-based LTF is given for inpatient management of SAM but not after discharge from NRC [6]. The findings of present study clearly show that non-milk based LTF can improve outcome of SAM patients if it is given after discharge at home.
Use of milk-based LTF in treatment of SAM patients after discharge has been restricted by shorter shelf life needing weekly follow-ups. Findings of present study using non-milk based LTF clearly demonstrate that significantly higher weight gain is achieved in these patients compared to control group with a good shelf life of 15 days.
The patients of SAM have poor weight gain after discharge if they are offered only home-based diet [3-5]. Several attempts have been made to find solution to this issue. Commercially prepared Ready to Use Therapeutic Foods (RUTF) such as “plumpy nut” has been used in Africa and is reported to have given very good results [5]. Manary MJ, compared RUTF with traditional Soya, Maize based diet and found that the weight gain in first group was much higher (7 g/kg/day) than the second group. (3.9 g/kg/day) [3]. Ciliberto MA et al., from Malawi, Africa, have also reported marginally superior weight gain (3.5 g/kg/day) with locally prepared RUTF compared to those offered only home-based diet (2 g/kg/day) [5]. Its use in India is however limited by the high-cost and apprehension that it may interfere with the prevailing traditional feeding practices in the community.
Not many studies are available which have assessed outcome of use of L-RUTF (like LTF) in comparison to home available foods in Indian literature. Wasnik VR and Rathi M, from Amravati have reported higher weight gain rates (11.8 g/day) in patient receiving commercially prepared “Mushpro” health drink powder as compared to rate of (2.6 g/day) in home-based diet group. This study was carried out in patients who were never admitted and given outpatient treatment [9]. Singh AS et al., carried out a study in preschool children with mild/moderate malnutrition given L-RUTF daily by teachers in school and found superior weight gain of 0.54 kg compared to 0.38 kg in home-based diet over three months period [4].
However, in Sandige H et al., at Malawi, carried out a quasi-randomised trial using imported RUTF (Plumpy Nut) versus locally made RUTF in SAM children aged 6-60 months. Recovery rate was reported more in locally prepared RUTF group (80%) as compared to Plumpy Nut (78%). However, the difference was not found to be statistically significant [10].
Bhandari N et al., in a recently concluded multicentric trial compared results of centrally produced RUTF (C-RUTF), locally prepared RUTF (L-RUTF) and augmented energy-dense Home Prepared Foods (A-HPF) in a community-based study [11]. Results of the study showed that both C-RUTF and L-RUTF resulted in faster recovery rates compared to A-HPF, 47.5%, 56.9% and 42.8% respectively. Significant was the fact that L-RUTF had even better recovery rate than C-RUTF [11]. The finding of efficacy of locally produced RUTF is similar to the locally prepared LTF used in the present study which has compared locally prepared non-milk based LTF with home-based therapy and reported significantly improved weight gain rate, MUAC and higher recovery rates after discharge from NRC [4,10,12]. The present study, patients were neither indoor nor were they called daily in Anganwadi or school. No commercial formula was used and follow-up was required only once in 15 days.
Community-based management of malnutrition is being recommended for majority (around 85%) of uncomplicated SAM [12]. Even complicated SAM after treatment of complication and initial rehabilitation on having to be treated in the community. There are recent reports that spontaneous recovery in these children is higher than expected (25-30%) and mortality lower than expected (1.2-2.7%) [13]. Caution should, however, be exercised in interpreting these findings. Even considering low mortality there would be more than 270,000 child deaths due to SAM in India [12].
There certainly is need for better community based management of SAM children in India. Many states have adopted the three-tier approach to community based management of SAM Government of Gujarat has started “Mission Balam Sukham” in which Village Child Nutrition Centre (VCNC) takes care of the village level management of malnutrition. Children are referred to higher centres i.e., Child Malnutrition Treatment Centre (CMTC) and NRC as per the requirements [6]. In a study from Vadodara, Gujarat, Zalavadiya DI et al., have found that nutritional status of malnourished children treated of VCNC and in ordinary Anganwadi did not differ significantly after three months of follow-up. There are many gaps still in the implementation of this program [14].
In view of the problems faced in community-based management of these children, the findings of the present study are very remarkable and have the potential to make significant contribution in fight against this intractable public health problem of malnutrition. What applies to discharged patients of NRC can also be applied to SAM patients who may not require admission at all.
From this study, it was also found out that Non-milk based LTF has a good shelf life of >15 days. It costs around nine rupees per 100 g which is cost-effective also. In this previous study (in press) at SSG Hospital milk based LTF was used, which had a short shelf life of just over seven days due to which frequently follow-ups were required for SAM children after discharge. And cost of milk based LTF was 19 rupees per 100 g. The average weight at the time of discharge was about 6 kg in both the groups in this study. As seen in [Table/Fig-2], a patient of 6 kg will need 200-250 g of non-milk based LTF per day. At a rate of 9 rupees/100 g this would cost 9×2=18 rupees/day for a child of 6 kg. In comparison milk based LTF would cost 19×2=38 rupees/day which is nearly double.
Limitation
The limitations of the study were relatively small sample size and this study has data from single centre. Another limitation of the study was that since the LTF was handed over to the parents it could not be monitored at home. Some of the food may have been consumed by the siblings.
Conclusion
In conclusion, the findings of the study show that giving non-milk based LTF to SAM patients on discharge from NRC significantly improve their rate of weight gain at home as compared to children who are given only home-based diet. Because non-milk based LTF also has a longer shelf life and can be given to the patient in follow-ups every two weeks, it is a practically feasible, economically affordable and logistically implementable strategy on a larger scale. It also does not require use of any commercial preparation. It can resolve one of the most difficult problems in management of SAM i.e., unsatisfactory weight gain after discharge.