Paraurethral Leiomyoma as an Uncommon Cause for Female Urethral Obstruction: Report of Two Cases
Vilvapathy Senguttuvan Karthikeyan1, Subramanian Ekambaram Sivanandam2, Jeyaraj Veena3, Venugopal Mohan4, Aswathaman Karthikeyan5
1 Consultant, Department of Urology, Sri Narayani Hospital and Research Centre, Vellore, Tamil Nadu, India.
2 Senior Consultant, Department of Urology, Sri Narayani Hospital and Research Centre, Vellore, Tamil Nadu, India.
3 Consultant, Department of Pathology, Sri Narayani Hospital and Research Centre, Vellore, Tamil Nadu, India.
4 Consultant and Head, Department of Radiology, Sri Narayani Hospital and Research Centre, Vellore, Tamil Nadu, India.
5 Senior Consultant and Head, Department of Urology, Sri Narayani Hospital and Research Centre, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subramanian Ekambaram Sivanandam, Senior Consultant, Department of Urology, Sri Narayani Hospital and Research Centre, Vellore-632055, Tamil Nadu, India.
E-mail: urosiva@gmail.com
Paraurethral Leiomyomas (PL) are rare benign mesenchymal tumours. Here, authors, report two premenopausal women presenting with obstructive urinary symptoms and a paraurethral vaginal swelling. They had firm mobile paraurethral masses. On magnetic resonance imaging, they were well-defined and no urethral invasion was noted. Surgical excision was performed in both women and histopathological examination confirmed benign spindle cell neoplasm suggestive of leiomyoma. After catheter removal, the patients voided well with maximum flow-rate of 27 mL/second and 25 mL/second respectively. Long-term follow-up is required as late recurrences and transformation to leiomyosarcoma have been reported.
Leiomyoma, Lower urinary tract symptoms, Urethral diseases
Case Report
Two premenopausal ladies, both mother of two children, aged 35 and 40 years, presented with a swelling in the vagina and weak urinary stream for six months and nine months respectively. They did not have frequency, nocturia, urgency, dysuria, urinary incontinence, haematuria or vaginal discharge. They did not have any comorbidities. Menstrual history was unremarkable in both women.
On examination, both patients had firm mobile masses, measuring 5 cm×5 cm×4 cm and 3 cm×3 cm×3 cm respectively, at the introitus posterior to the external urethral meatus. Serum creatinine was normal. Upper urinary tracts and urinary bladder on Ultrasound (US) were normal. On uroflowmetry, maximal flow rate (Qmax) was 9 mL/second in first patient and 11 mL/second in the second patient. Magnetic Resonance Imaging (MRI) showed a well-defined lesion measuring 4.9 cm×3.5 cm×3.4 cm [Table/Fig-1] and 3.9 cm×3.2 cm×3.3 cm [Table/Fig-2] respectively, between the urethra and lower one-third of anterior vaginal wall, hypointense on T1-Weighted Images (T1WI) and iso- to hypointense on T2-Weighted Images (T2WI). There was no urethral invasion. A provisional diagnosis of paraurethral leiomyoma was made.
Patient 1: Magnetic resonance imagjng showing relationship of paraurethral leiomyoma to the urethra in: a) Axial; and b) Sagittal sections (U=Urethra; L-Leiomyoma).
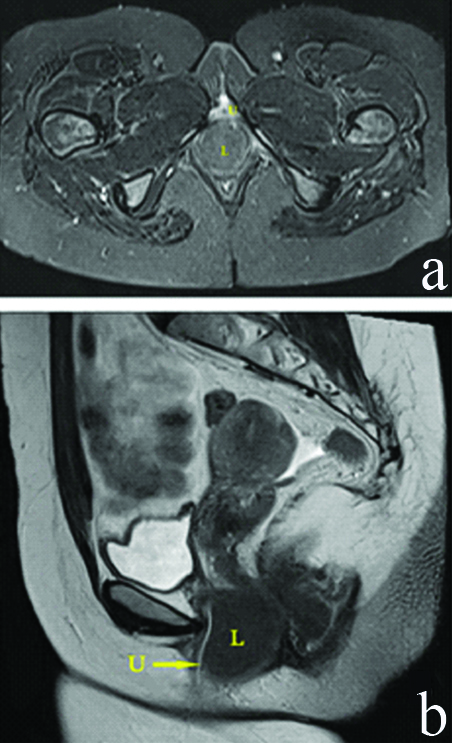
Patient 2: Magnetic resonance imaging showing relationship of paraurethral leiomyoma to the urethra in: a) Axial; and b) Sagittal sections (U=Urethra; L-Leiomyoma).

Intraoperatively, the swelling was noted in anterior vaginal wall near the introitus and a 16 French periurethral Foley catheter was placed [Table/Fig-3]. An elliptical vaginal incision was made. Tumour was separated from the urethra by sharp and blunt dissection and complete excision was done. Urethrocystoscopy after excision revealed intact urethra. Vagina was closed with 2-0 vicryl sutures. They voided well with Qmax of 27 mL/second and 25 mL/second respectively, after periurethral foley catheter removal. On gross examination, the specimen was a bosselated, encapsulated tumour with soft to firm solid finely trabeculated glistening cut surface. On microscopy, the circumscribed tumour was composed of interlacing fascicles of spindle shaped cells with individual cells showing oval nuclei with inconspicuous nucleoli exhibiting mild nuclear pleomorphism and abundant eosinophilic cytoplasm and mitotic activity of 1/10 HPF, suggestive of spindle cell neoplasm Immunohistochemistry (IHC) was positive for desmin and smooth muscle antigen in first and second patients respectively [Table/Fig-4,5]. Final diagnosis was benign paraurethral spindle cell neoplasm suggestive of leiomyoma. Both women are voiding well, without recurrence of tumour at 24-months follow-up.
Paraurethral leiomyoma with foley per urethral catheter demonstrating the location of mass posterior to the external urethral meatus. a) Patient 1; b) Patient 2 (scale demonstrating the size).

Patient 1: Photomicrographs: a) Interlacing fascicles of spindle shaped cells with individual cells showing oval nuclei with abundant eosinophilic cytoplasm and low mitotic activity (H&E, x100); b) Immunohistochemistry showing tumour staining with desmin (x100).

Patient 2: Photomicrographs: a) Interlacing spindle shaped cell fascicles with oval nuclei, abundant eosinophilic cytoplasm and low mitiotic activity (H&E, x100); b) Immunohistochemistry showing tumour staining with smooth muscle antigen (x100).

Discussion
Leiomyomas are benign mesenchymal tumours, commonly seen in the female genital tract (95%) and rarely in urinary tract [1-3]. Urethral Leiomyomas (UL) and PL are very rare and are categorised as deep tissue leiomyomas [3]. UL and PL contribute to 5-7% of paraurethral masses [4-6]. PL may be asymptomatic or symptomatic in the form of mass, urinary symptoms or dyspareunia [2,3]. PL may present with features mimicking uterovaginal prolapse, urethral obstruction, recurrent urinary infections, vaginal bleed or abdominal pain [Table/Fig-6] [4-6].
Reported cases of paraurethral leiomyoma in English literature [6,9-17].
| Sl. No. | Author | Year | Age | Presentation | Treatment | Follow-up | Complications |
|---|
| 1 | Adams-Piper E et al., [6] | 2016 | 20 | Incidental mass | Excision | - | - |
| 2 | Harada S et al., [9] | 2018 | 50 | Mass per urethra | Excision | - | - |
| 3 | Aydogmus K et al., [10] | 2017 | 49 | Mass per vaginum and dyspareunia | Excision | - | - |
| 4 | Pastor Navarro et H al., [2] | 2013 | 40 | Mass per vaginum and dyspareunia | Excision+closure of cervix | six years | - |
| 5 | Migliari R et al., – 6 patients [11] | 2015 | 32-49 | - | Excision | - | - |
| 6 | Maeda K et al., [12] | 2015 | 44 | Urinary retention | Excision | three months | - |
| 7 | Mukthar S et al., [13] | 2011 | 23 | Mass per vaginum and dyspareunia | Excision | two months | - |
| 8 | Bruschini H et al., [14] | 2006 | - | Obstructive lower urinary tract symptoms | Excision | - | - |
| 9 | Chong KM et al., [15] | 2006 | - | Vaginal bleed | Excision | | |
| 10 | Tantbirojn P et al., [16] | 2006 | 44 | Mass | Excision | - | - |
| 11 | Blaivas JG et al., – 79 patients [17] | 2004 | - | 72 had lower urinary tract symptoms and 7 referred for periurethral mass | Excision | - | - |
| 12 | Present report | 2018 | 35 and 40 | Obstructive lower urinary tract symptoms | Excision | two years | - |
Differential diagnoses for PL include a variety of congenital, inflammatory, cystic lesions or tumours from urethra and vagina. They include urethral caruncle or diverticulum, prolapsed ectopic ureterocele, cystocele, urethrocele, Gartner duct cyst, Bartholin gland cyst, epidermal inclusion cyst, endometriosis, fibrous polyp, congenital paraurethral cysts, Skene’s duct abscess, urethral papilloma, leiomyosarcoma, rhabdomyosarcoma or malakoplakia [2,3,7]. In order to distinguish UL from PL, characteristic physical examination findings have been proposed. UL are fixed and can protrude through the urethra while PL is mobile. This distinction is necessary to avoid urethral injury during excision of the mass [2]. In both patients, authors found that the tumours were mobile and hence they were diagnosed to have PL.
US and MRI provide valuable information regarding the diagnosis and extent of PL [7]. Transvaginal US can determine relationship of PL with respect to the urethra. On MRI, PL appears well circumscribed, whorled masses, hypointense or isointense to muscle on T1WI and still relatively low signal intensity on T2WI suggesting mesenchymal origin [2,8]. Heterogeneously enhancing lesions on T2-weighted MRI with irregular enhancement on post-contrast-enhanced images may point towards leiomyosarcoma and rhabdomyosarcoma [8].
Though PL is benign, excision is the treatment of choice to confirm the diagnosis [Table/Fig-6] [6,9-17]. A vaginal approach is utilised for the resection of small to moderate sized PL [2]. For larger PL, an abdominoperineal approach may be necessary [3]. PL may be biopsied using TVS and excised after histopathological confirmation.
PL show well-defined tumours enveloped in a fibrous capsule free from adjacent structures. Capsule is made of fasciculi of spindle shaped cells with eosinophilic cytoplasm and central nuclei, with little mitotic activity [2]. Leiomyosarcoma shows marked pleomorphism, increased cellularity, and mitotic activity [5]. On IHC, PL express smooth muscle actin, muscle-specific actin, desmin, caldesmon, Cluster of Differentiation 10 (CD10), myosin, and vimentin. CD68, CD117, S-100, chromogranin and synaptophysin are not expressed by leiomyomas [2,8]. Recurrence or malignant transformation has been rarely reported in extrauterine sites which can occur even after nine years [5,7].
Typically, UL present with obstructive lower urinary tract symptoms. PL is a rare cause of obstructive lower urinary tract symptoms in women aged between 30 and 50 years. Both of the present patients had poor urinary stream due to PL. Once the PL was excised, both of them voided well with good urinary stream. Urethra is closely related to PL and hence care should be taken to avoid injury to urethra during excision. A foley periurethral catheter is useful to identify the urethra.
Conclusion
Paraurethral Leiomyomas (PL) are rare benign mesenchymal neoplasms and can present with obstructive lower urinary tract symptoms. Excision is the treatment of choice. Urethral injury should be avoided and integrity should be assessed at the end of surgical procedure. Long-term follow-up is required in view of rare chance of recurrence and malignant change of PL.
[1]. Chakrabarti I, De A, Pati S, Vaginal leiomyomaJ Midlife Health 2011 2(1):42-43.10.4103/0976-7800.8327421897740 [Google Scholar] [CrossRef] [PubMed]
[2]. Pastor Navarro H, Martínez Ruiz J, Martínez Sanchíz C, Perán Teruel M, Segura Martín M, Pastor Guzman JM, Paraurethral leiomyomaArch Esp Urol 201 66(8):820-23. [Google Scholar]
[3]. Wu Y, Wang W, Sheng X, Kong L, Qi J, A misdiagnosed vaginal leiomyoma: case reportUrol Case Rep 2015 3(3):82-83.10.1016/j.eucr.2015.02.00426793510 [Google Scholar] [CrossRef] [PubMed]
[4]. Goyal LD, Kaur H, Kaur K, Kaur S, An unusual case of vaginal myoma presenting with postmenopausal bleedingJ Family Reprod Health 2013 7(2):103-04. [Google Scholar]
[5]. de Lima Junior MM, Sampaio CB, Ticianeli JG, de Lima MM, Granja F, Leiomyoma--a rare benign tumour of the female urethra: a case reportJ Med Case Rep 2014 8:36610.1186/1752-1947-8-36625391855 [Google Scholar] [CrossRef] [PubMed]
[6]. Adams-Piper E, Jacobs S, Ghoniem GM, Paraurethral leiomyoma in a 20-year-old woman: a case reportUrol Case Rep 2015 4:14-16.10.1016/j.eucr.2015.10.00826793567 [Google Scholar] [CrossRef] [PubMed]
[7]. Shen YH, Yang K, Recurrent huge leiomyoma of the urethra in a female patient: A case reportOncol Lett 2014 7(6):1933-35.10.3892/ol.2014.199124932262 [Google Scholar] [CrossRef] [PubMed]
[8]. Sim CH, Lee JH, Kwak JS, Song SH, Necrotizing ruptured vaginal leiomyoma mimicking a malignant neoplasmObstet Gynecol Sci 2014 57(6):560-63.10.5468/ogs.2014.57.6.56025469351 [Google Scholar] [CrossRef] [PubMed]
[9]. Harada K, Ishikawa Y, Fujiwara H, Ishihara G, Female paraurethral leiomyoma successfully excised through a vaginal approach: A case reportJ Obstet Gynaecol Res 2018 44(6):1174-76.10.1111/jog.1364129607582 [Google Scholar] [CrossRef] [PubMed]
[10]. Aydogmus S, Aydogmus H, Ekmekci E, Keleckci S, Eris S, Paraurethral LeiomyomaJ Reprod Med 2017 62(1-2):85-88. [Google Scholar]
[11]. Migliari R, Buffardi A, Mosso L, Female paraurethral leiomyoma: treatment and long-term follow-upInt Urogynecol J 2015 26(12):1821-25.10.1007/s00192-015-2776-826224380 [Google Scholar] [CrossRef] [PubMed]
[12]. Maeda K, Wada A, Kageyama S, Takimoto K, Narita M, Kawauchi A, A female paraurethral leiomyoma causing urinary retention: a case reportHinyokika Kiyo 2015 61(11):455-58. [Google Scholar]
[13]. Mukhtar S, Saeed M, Saeed R, Ikram M, Paraurethral leiomyomaJ Coll Physicians Surg Pak 2011 21(11):702-03. [Google Scholar]
[14]. Bruschini H, Truzzi JC, Simonetti R, Mesquita R, Delcelo R, Szenfeld J, Paraurethral leiomyoma in a female causing urinary obstructionInt Urogynecol J Pelvic Floor Dysfunct 2006 17(3):286-89.10.1007/s00192-005-1329-y16075157 [Google Scholar] [CrossRef] [PubMed]
[15]. Chong KM, Chuang J, Tsai YL, Hwang JL, A rapidly growing paraurethral myoma with profuse bleeding from a mucosal vessel: report of a caseGynecol Obstet Invest 2006 61(2):87-89.10.1159/00008901016244489 [Google Scholar] [CrossRef] [PubMed]
[16]. Tantbirojn P, Sansopha L, Thanakit V, Sirisubya N, Paraurethral leiomyoma: a case reportJ Med Assoc Thai 2006 89(4):545-49. [Google Scholar]
[17]. Blaivas JG, Flisser AJ, Bleustein CB, Panagopoulos G, Periurethral masses: etiology and diagnosis in a large series of womenObstet Gynecol 2004 103(5 Pt 1):842-47.10.1097/01.AOG.0000124848.63750.e615121554 [Google Scholar] [CrossRef] [CrossRef]