Panhypopituitarism without Thrombosis due to Primary Antiphospholipid Syndrome
Pulin Kumar Gupta1, Subodh Kumar Mahto2, Arjun Malasandra Balakrishna3, Parikha Rampal4, Narendra Kumar Sharma5
1 Professor, Department of Medicine, PGIMER, Dr. RML Hospital, New Delhi, India.
2 Senior Resident, Department of Medicine, PGIMER, Dr. RML Hospital, New Delhi, India.
3 Senior Resident, Department of Medicine, Sucheta Kriplani Hospital and LHMC, New Delhi, India.
4 Postgraduate, Department of Radiology, PGIMER, Dr. RML Hospital, New Delhi, India.
5 Senior Resident, Department of Medicine, PGIMER, DR. RML Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subodh Kumar Mahto, Senior Resident, Department of Medicine, OPD Block, PGIMER, Dr. RML Hospital, New Delhi-110001, India.
E-mail: drsubodhkr05@gmail.com
Hypopituitarism is a clinical syndrome in which pituitary hormones deficiency is seen in many conditions. Antiphospholipid Syndrome (APS) is an autoimmune disease characterised by antiphospholipid antibodies, commonly manifests as venous or arterial thrombosis with recurrent foetal loss. We here by report a case of 40-year-old female who presented with bilateral swelling of lower limbs with exertional breathlessness along with feeling of cold extremities, easy fatigability, lethargy and decreased appetite for six months which turned out to be hypopituitarism with APS. Hormone replacement was started and she experienced a good clinical improvement.
Autoimmune, Hormone replacement, Hypopituitarism
Case Report
A 40-year-old female presented with complaints of progressively increasing bilateral swelling of lower limbs since six months associated with exertional breathlessness. Pitting type swelling, not associated with pain and itching, first appeared on both feet, which progressed upwards to knees. She had also complained of difficulty in breathing which was increased on exertion and relieved on rest, not associated with orthopnea and proximal nocturnal dyspnea. Patient complained of rashes, arthralgia, oral ulcer and photosensitivity which were present on and off since six months, subsided after taking medication, however she was not investigated. Multiple, small, reddish, non-blanchable, non-indurated, flat pin point size rashes were present all over the face and both hands. There were also complaints of decreased appetite, lethargy, easy fatigability and feeling of cold extremities for same duration. She also had history of menstrual irregularities. History of one abortion at 14th week of gestation six years back. On general physical examination; she had mild pallor and bilateral pedal oedema. Rests of the general physical and systemic examination were within normal limits.
Laboratory investigations revealed 8 gm/dL haemoglobin with total leukocyte count 5300/mm3 with normal differential and platelet counts. Peripheral smear revealed RBC showing moderate anisopoikilocytosis with presence of microcytes, target cells with normochromic to mildly hypochromic picture. The erythrocyte sedimentation rate was 55 mm/1st hour. Urine examination was normal with no dysmorphic RBC. Renal function tests and liver function tests were all within normal limits. LDH level was 233 U/L. Coomb’s test (Direct and indirect) was negative. A 24 hour urine protein was 250 mg/day. HBsAg, Anti HCV and HIV were all negative. D-Dimer was normal. C-reactine protein was raised (>20 mg/dL) while complement levels were normal. Ultrasonography of the abdomen and 2-echo were normal.
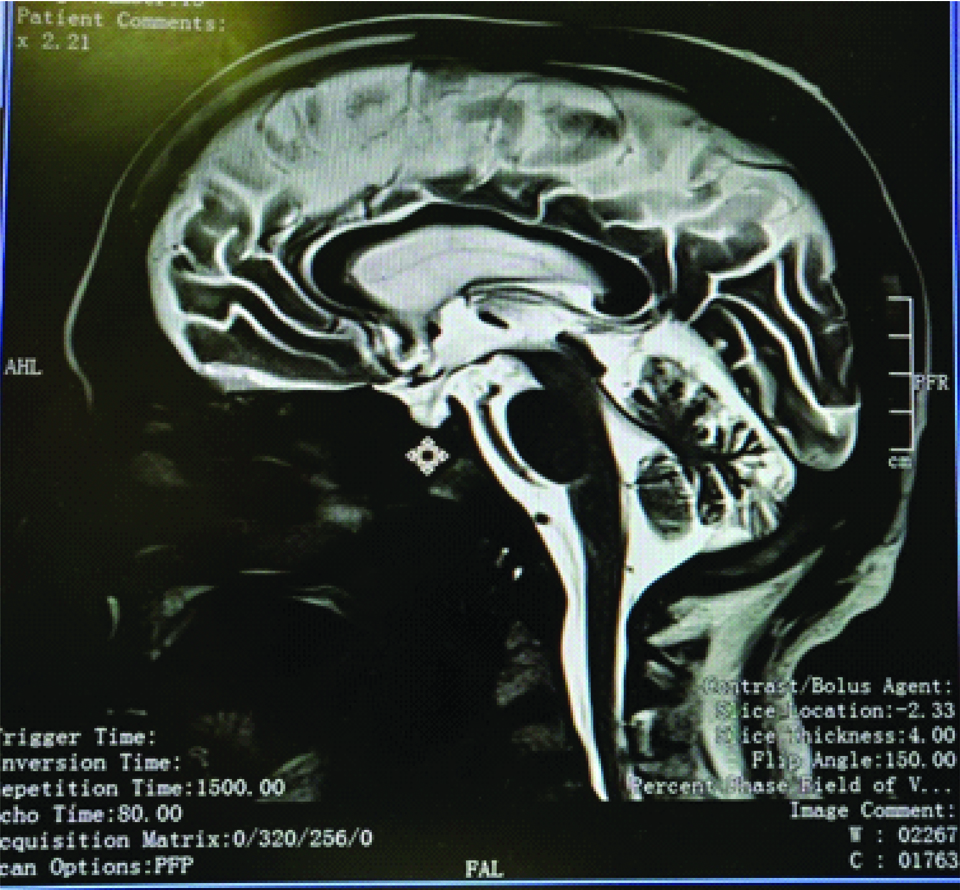
Anti-Neutrophil Antibody level (ANA) and anti-ds DNA were negative. Antiphospholipid antibodies (both IgM and IgG) were raised while Anticardiolipin antibody (both IgM and IgG) were negative [Table/Fig-1]. Hormonal profile was suggestive of low levels of estradiol, progesterone, cortisol and prolactin [Table/Fig-2]. MRI brain showed CSF signal intensity in the visualised sella on the T2 image suggestive of empty sella [Table/Fig-3]. She was treated with oral fludrocortisone initially followed by sex hormones and l-thyroxine. All her symptoms except pedal oedema were resolved before discharge. Her appetite and lethargy improved. During 1st monthly follow-up visit, her haemoglobin had increased to 9.7 gm/dL and pedal oedema had resolved too. Repeat B2 glycoprotein level was done after 12 weeks during subsequent follow-up, which was also elevated.
Autoimmune profile of the patient.
| Autoimmune profiles | Observed value | Normal value |
|---|
| Anti-Neutrophil Antibody (ANA) | 18.50 U/L | <20 U/L |
| Anti-ds DNA | 7.49 IU/mL | <10 IU/mL |
| Antiphospholipid antibodies IgM | 32.96 MPL U/mL | 0.50-10 MPL U/mL |
| Antiphospholipid antibodies IgG | 18.16 GPL U/mL | 0.50-10 GPL U/mL |
| Anticardiolipin antibody IgG | 2.84 GPL U/mL | 0.50-10 GPL U |
| Anticardiolipin antibody IgM | 4.04 MPL U/mL | 0.50-10 MPL U. |
Hormonal profile of the patient.
| Hormonal profiles | Observed value | Normal value |
|---|
| fT3 | 0.50 pg/mL | 2.30-4.20 pg/mL |
| fT4 | 0.10 ng/mL | 0.70-1.51 ng/mL |
| S.TSH | 0.567 μIU/mL | 0.550-4.780 μIU/mL |
| LH | 4.47 mIU/mL) | 0.8-15.5 mIU/mL |
| FSH | 16.6 mIU/mL | 1.3-23.4 mIU/mL |
| Prolactin | 2.0 ng/mL | 3-18.6 ng/mL |
| Estradiol | 34.06 pmol/L | 97.5-592 pmol/L |
| Progesterone | 0.291 nmol/L | 0.44-6.47 nmol/L |
| Serum cortisol | 42.1 nmol/L | 123-626 nmol/L |
MRI brain showed CSF signal intensity in the visualised sella on the T2 image suggestive of empty sella.
Discussion
Antiphospholipid Syndrome (APS) is a systemic autoimmune disorder characterised by venous or arterial thrombosis and/or pregnancy related morbidities and complications in the presence of antiphospholipid antibodies. Antiphospholipid antibodies are autoantibodies directed against phospholipid-binding proteins [1]. APS, in addition to the classic episodes of deep venous thrombosis and stroke, involves almost all the organ systems including heart, placenta, endocrine system and renal system [2,3]. The involvement of multiple endocrine glands including adrenals, thyroid, parathyroid, ovaries, and testis have been well described in literature [2]; however the data regarding involvement of pituitary gland in APS from Indian subcontinent is scarce.
The major clinical features of APS are thrombose, thrombocytopenia and recurrent foetal demise. Recent reports have indicated that antiphospholipid antibodies are also related to other clinical manifestations, including cardiac valve lesions and haemolytic anemia with or without underlying autoimmune diseases such as Systemic Lupus Erythematous (SLE). The origin of these pathogenic autoantibodies still remains a mystery but is likely to be due to the complex interaction of multiple environmental factors in individuals with genetic markers that increase susceptibility to the disease [4].
Our patient was a 40-year-old lady who presented with non-specific complaints which were not investigated for almost more than six months and were considered as a part of somatization disorder. Though there was a history of abortion, it was not investigated further as patient did not have any symptoms of hypopituitarism during or after pregnancy until now. Most of the cases published in the existing literature [3] have described the association of antiphospholipid antibodies with hypopituitarism only during pregnancy, but our patient was diagnosed with antiphospholipid antibodies syndrome six years after abortion when she presented with symptoms of multiple hormonal deficiency. Auto-immunity is an independent risk factor for pituitary necrosis [5].
Primary and secondary hypopituitarisms, adrenal insufficiencies (Addison’s disease), ovarian failure, hypoparathyroidism, hypothyroidism and hyperthyroidism (Graves’ disease) have been reported as endocrine disorders related to cases of APS [2,6,7]. Lymphocytic hypophysitis has also been reported as a cause for hypopituitarism in antiphospholipid antibodies syndrome [8]. These reported cases also indicated that many such patients showed recurrent multiple thrombotic events affecting veins and arteries, including myocardial infarction and cerebral stroke [6], however our patient did not show any such thrombotic symptoms. A high index of clinical suspicions is required as patients can present with rapidly evolving non-specific symptoms of corticotrophin or thyroid deficiency many years after child birth. Symptoms of a mass lesion such as headache and visual loss are also very common [6]. Sellar MRI commonly depicts a homogeneous gadolinium enhancement of the pituitary gland [9]. The empty sella of the pituitary gland and related hypopituitarism of our patient may be related to the formation of thrombi caused by antiphospholipid antibodies. Our case indicates that the presence of antiphospholipid antibodies, even in the absence of catastrophic thrombosis, may be an independent risk factor for endocrine diseases, including panhypopituitarism, and the prevalence of APS may be much higher in patients with panhypopituitarism, than it is appreciated.
Conclusion
Though adrenal insufficiency is the commonest endocrine disorder associated with APS physicians should also be aware of the possibility of underlying panhypopituitarism in such patients. Early diagnosis and adequate replacement of the deficient hormones significantly reduces the overall morbidity and also helps in preventing long term complications.
[1]. Lim W, Antiphospholipid syndromeHematology Am Soc Hematol Educ Program 2013 2013:675-80.10.1182/asheducation-2013.1.67524319251 [Google Scholar] [CrossRef] [PubMed]
[2]. Uthman I, Salti I, Khamashta M, Endocrinologic manifestations of the antiphopolipid syndromeLupus 2006 15:485-89.10.1191/0961203306lu2318rr16941999 [Google Scholar] [CrossRef] [PubMed]
[3]. Asherson RA, Petri M, Endocrine manifestations in the antiphospholipid syndrome. In: Asherson RA, Cervera R, Piette JC, Shoenfeld YThe antiphospholipid syndrome II 2002 AmsterdamElsevier Science BV:245-257.10.1016/B978-044450987-1/50026-7 [Google Scholar] [CrossRef]
[4]. Sherer Y, Blank M, Shoenfeld Y, Antiphospholipid syndrome (APS): Where does it come from?Best Pract Res Clin Rheumatol 2007 21:1071-78.10.1016/j.berh.2007.09.00518068862 [Google Scholar] [CrossRef] [PubMed]
[5]. Paiva I, Gomes L, Ribeiro C, Carvalheiro M, Ruas MM, Autoimmune hypophysitis or lymphocytic hypophysitisActa Med Port 2003 16:459-63. [Google Scholar]
[6]. Ikeda K, Takahama M, Matsushita M, Ando S, Sekigawa I, Iida N, A case of hypopituitarism associated with antiphospholipid syndromeRheumatology (Oxford) 2000 39:447-48.10.1093/rheumatology/39.4.44710817784 [Google Scholar] [CrossRef] [PubMed]
[7]. Mehdi AA, Salti I, Uthman I, Antiphospholipid syndrome: Endocrinologic manifestations and organ involvementSemin Thromb Hemost 2011 37:49-57.10.1055/s-0030-1270071 [Google Scholar] [CrossRef]
[8]. Da Silva BS, Bonin C, Bueno CB, Glezer A, Bronstein MD, Carvalho JF, Primary antiphospholipid syndrome and panhypopituitarism: A unique presentationActa Reumatol Port 2012 37:272-75. [Google Scholar]
[9]. Caturegli P, Newschaffer C, Olivi A, Pomper MG, Burger PC, Rose NR, Autoimmune hypophysitisEndoc Rev 2005 265:599-614.10.1210/er.2004-001115634713 [Google Scholar] [CrossRef] [PubMed]