Rheumatoid Arthritis (RA) is one of the most frequent autoimmune diseases in the world which affects about 1% of people [1]. Disease severity can be assessed with severity scores of which include Disease Activity Score 28 (DAS28) [2,3], Simplified Disease Activity Index (SDAI) [3,4] and Clinical Disease Activity Index (CDAI) [3,4]. The most effective way to manage RA patients is early diagnosis and timely treatment with Disease Modifying Anti-Rheumatic Drugs (DMARDs), which prevent the exacerbation of disease, reduce the probability of joint destruction, and improve the outcome [5]. RA has variable course ranging from mild to aggressive forms. Availability of better prognostic markers would make it possible to select predictably severe cases for aggressive therapy, and also avoiding unnecessary exposure of patients with mild disease. Till now, serological support in the diagnosis of RA was mainly based on the presence of rheumatoid factor [6].
Anti-Cyclic Citrullinated Peptides (Anti-CCP) is shown to be more specific than rheumatoid factor in the diagnosis of RA [7]. This test becomes positive in early stage of disease and it has a high predictive value [7]. Anti-CCP antibodies are detected in seropositive as well as in seronegative RA patients [8]. They are detected by Enzyme-Linked Immunosorbent Assays (ELISA) and are found in most patients with RA but less often in other diseases and hence are specific [9,10].
Hence, the present study was conducted to investigate the correlation of disease severity of RA with antibody titers, anti-CCP and rheumatoid factor.
Materials and Methods
A cross-sectional study was conducted on 50 patients with RA attending outpatient department and in patient at Kasturba Medical College, Mangalore, Karnataka, India, over two years from August 2011 to September 2013. Sample size calculation was done using the formula [11].
Z alpha2pq/d2, Z alpha=1.96, p=47.7; with 95% confidence interval, 15% absolute precision, p=47.7 and the sample size comes to 42.
Patients fulfilling the ACR-EULAR 2010 (American College of Rheumatology European League Against Rheumatism) [12] criteria [Table/Fig-1] and above 16 years of age were included in this study. The study excluded patients with age<16 years, those who had associated overlap syndromes, pregnant and lactating patients and those who did not give valid consent. A detailed examination of each patient including their demographic characteristics, duration of disease, number of tender and swollen joints, Westergren’s ESR and C-Reactive Protein, patient’s and physician’s global assessment by VAS (0-10) and titers of rheumatoid factor and anti-CCP antibody. The rheumatoid factor (IgM) and anti-CCP were measured by using an ELISA, according to the producer protocol. The cut-off points was more than 15 IU/mL for rheumatoid factor and more than 5 RU/mL for Anti-CCP [6,7]. Severity of disease in patients was calculated by disease activity scores namely DAS28 [2,3], SDAI [3,4] CDAI [3,4]. The study was approved by institutional ethics committee and informed consent was taken from all the patients.
ACR-EULAR 2010 criteria-Classification criteria for RA* (score-based algorithm: add score of categories A-D; A score of >6 points is required for classification as definite RA according to ACR-EULAR 2010 criteria
| A) Joint involvement | Score |
| 1 large joint (shoulder, elbow, hip, knee, ankle) | 0 |
| 2-10 large joints | 1 |
| 1-3 small joints (MCP†, PIP‡, Thumb IP§, MTP||, wrists) | 2 |
| 4-10 small joints | 3 |
| >10 joints (at least 1 small joint) | 5 |
| B) Serology |
| Negative RF** and negative Anti-CCP†† | 0 |
| Low-positive RF** or low-positive anti-CCP†† antibodiesHigh-positive RF** or high-positive anti-CCP†† antibodies (>3 times Upper Limit of Normal) | 23 |
| C) Acute-phase reactants |
| Normal C Reactive Protein and normal ESR‡‡Abnormal C Reactive Protein or abnormal ESR‡‡ | 01 |
| D) Duration of symptoms |
| <6 weeks>6 weeks | 01 |
*RA=Rheumatoid Arthritis.†MCP-Metacarpophalengeal joint‡ PIP-Proximal interphalengeal joint §IP-Interphalangeal joint ||MTP-Metatarsophalangeal joint **RF-Rheumatoid factor ††Anti-CCP-Anti cyclic citrullinated peptide ‡‡ESR-Erythrocyte sedimentation rate. Note: These criteria are aimed at classification of newly presenting patients who have at least 1 joint with definite clinical synovitis that is not better explained by another disease.
DAS28 is calculated using an electronic device and also by using the DAS 28 online software (http://www.das-score.nl/www.das-score.nl/index.html) [2]. The following variables are required to calculate: Tender Joint Count (TJC) score 0-28, Swollen Joint Count (SJC) score 0-28, Patient’s global assessment VAS 0-10 (0 being no pain and 10 being unbearable pain), Physician global assessment VAS 0-10, ESR Westergren method (mm/hr). The 28 joints taken into account are shoulder (2), elbows (2), wrists (2), metacarpophalangeals (10), proximal interphalangeals (10) and knees (2).
SDAI [4] is simple sum of five variables namely TJC score (0-28), SJC score (0-28), Patient’s Global Assessment VAS 0-10 (PTGA), Physician global assessment VAS 0-10 (PHGA), C-reactive protein (mg/dL). CDAI [4] is a clinical index which is calculated similar to SDAI variables excluding CRP namely, TJC score (0-28), SJC score (0-28), Patient’s global assessment VAS 0-10, Physician global assessment VAS 0-10 [Table/Fig-2].
Characteristics of selected tools in rheumatoid arthritis.
| Tool | Formula | Low Disease Activity | Moderate Disease Activity | High Disease Activity |
|---|
| DAS28 | (0.56x√TJC)+(0.28x√SJC)+(0.70xlognESR)+(0.014xPGA) | <2.6 | <3.2 | <5.1 |
| SDAI | SJC+TJC+PGA+PhGA+CRP | <3.3 | <11 | <26 |
| CDAI | SJC+TJC+PGA+PhGA | <2.8 | <10 | <22 |
CDAI=Clinical Disease Activity Index; CRP=C-Reactive Protein, DAS28=Disease Activity Score 28 Joints; ESR=erythrocyte sedimentation rate; logn=log-normal; PGA=Patient Global Assessment; PhGA=Physician Global Assessment; SDAI=Simplified Disease Activity Index; SJC=Swollen joint count of 28 joints; TJC=Tender joint counts of 28 joints.
Statistical Analysis
The results were analysed by SPSS software (version 19). Pearson’s correlation coefficient was used. A p-value less than 0.05 were regarded as significant.
Results
Fifty patients with RA were evaluated (mean age- 44.82: range-18-70) [Table/Fig-3].
| Age (years) | Frequency (n) | Percentage (%) |
| <30 | 8 | 16 |
| 30-40 | 13 | 26 |
| 40-50 | 12 | 24 |
| 50-60 | 13 | 26 |
| >60 | 4 | 8 |
| Gender | Frequency (n) | Percentage (%) |
| Male | 12 | 24 |
| Female | 38 | 76 |
| Duration of illness | Frequency (n) | Percentage (%) |
| <3months | 6 | 12 |
| 3 month-2 years | 26 | 52 |
| >2 years | 18 | 36 |
| RF and Anti-CCP | Frequency (n) | Anti-CCP titres (RU/mL) |
| RF positive | 41 | 181.5±116.5 |
| Negative | 9 | 197.15±119.4 |
| Disease activity | High | Moderate |
| DAS 28 | 39 | 11 |
| SDAI | 38 | 12 |
| CDAI | 37 | 13 |
Patients were divided according to disease duration (<3 months, 3 months -2 yr, >2 yrs) [Table/Fig-3]; eight patients (16%) being in the early RA group with mean duration being 2.6 years. Thirteen patients (26%) were in the age group 30-40 and 50-60 while the lowest (8%) were in the >60 age group with mean age being 44.82±11.81 [Table/Fig-3].
Mean duration of early morning stiffness was 14.3±26.8 min. Mean ESR was 54±27 mm/hr. Mean CRP was 17.277±23.41 mg/dL. Mean DAS 28 was 5.955±0.962; mean SDAI was 46.9±27.1 and CDAI 28.9±10.8 Out of 50, 38 (76%) were females and 12 (24%) were males [Table/Fig-3]. Forty-nine patients were anti-CCP positive (98%) and one was negative (2%). The mean±SD titer of the anti-CCP was 184.3±114.2 RU range 5.8-500 [Table/Fig-3]. Forty one patients were rheumatoid factor positive (82%) and nine were RF negative (18%) with mean titer of 122.9±146.85 IU/mL. The patient negative for Anti-CCP was positive for RF [Table/Fig-3].
In none of the patients, disease activity was low as calculated by DAS-28, SDAI and CDAI. Severity with DAS-28 was high in 39 (78%) patients and moderate in 11 (22%) of patients. Scores of SDAI was high in 38 (76%) patients and moderate in 12 (24%) of patients. In comparison, CDAI was high in 37 (74%) patients and moderate in 13 (26%) patients [Table/Fig-3].
With use of Pearson’s correlation coefficient, we checked the correlation between rheumatoid factor and anti-CCP with SDAI, CDAI and DAS-28. There was no correlation between the titers of anti-CCP and DAS-28 (r=0.04, p=0.078) [Table/Fig-4] while significant correlation between anti-CCP levels and SDAI (r=0.059, p=0.037) [Table/Fig-5] and CDAI (r=0.08, p=0.029) [Table/Fig-6]; though DAS-28 scores were higher for patients who were positive for anti-CCP. The levels of Rheumatoid factor correlated with SDAI (r=0.032, p=0.023) [Table/Fig-7], CDAI (r=0.032, p=0.023) [Table/Fig-8] and DAS-28 scores (r=0.02, p=0.042) [Table/Fig-9]. Also, DAS-28 strongly correlated with SDAI (r=0.550, p<0.0001), and CDAI (r=0.808, p<0.0001).
Correlation between Anti-CCP and DAS-28 (r=0.04, p=0.078).
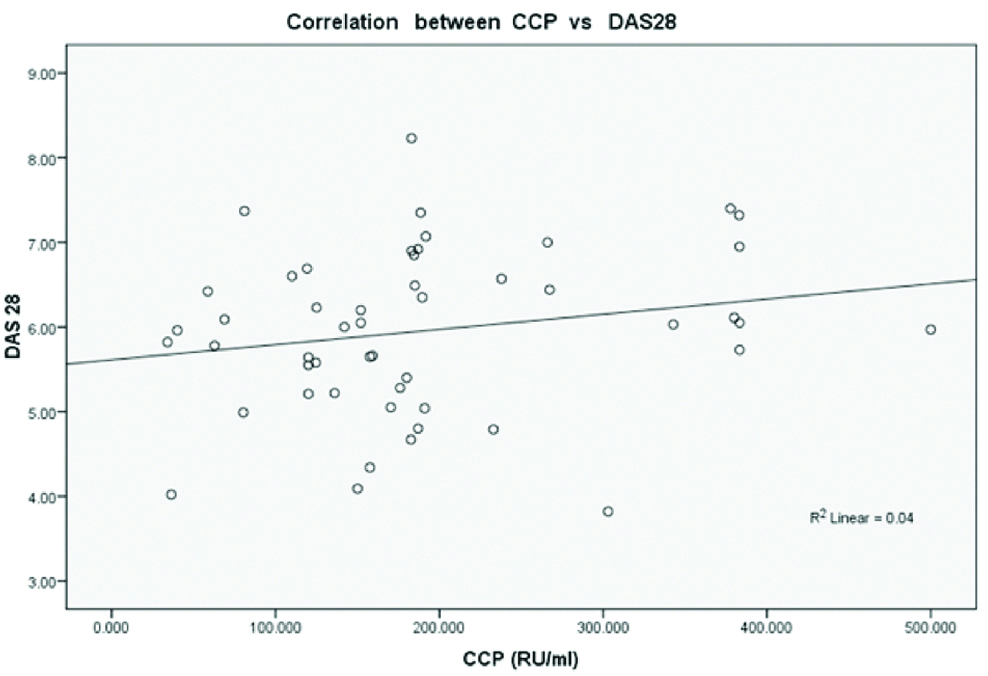 |
| n=50 | Anti-CCP | DAS-28 | r-value | p-value |
| Mean | 184.347 | 5.955 | 0.04 | 0.078 |
| Std deviation | 114.223 | 0.962 |
Correlation between Anti-CCP and SDAI (r=0.059, p=0.037).
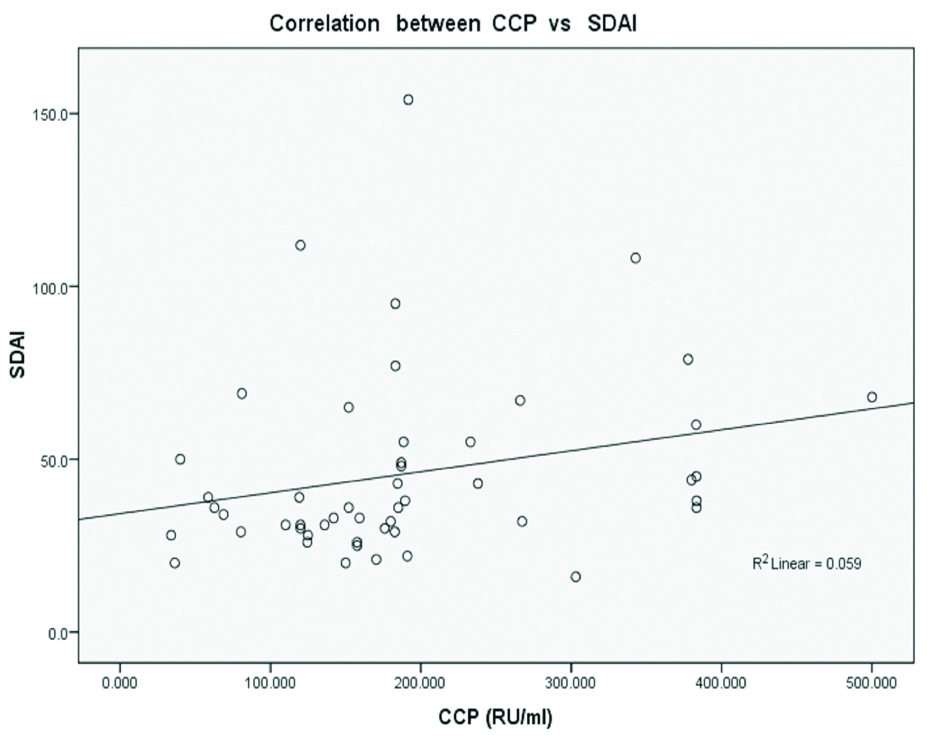 |
| n=50 | Anti-CCP | SDAI | r-value | p-value |
| Mean | 184.347 | 46.90 | 0.059 | 0.037 |
| Std deviation | 114.223 | 27.156 |
Correlation between Anti-CCP and CDAI (r=0.08, p=0.029).
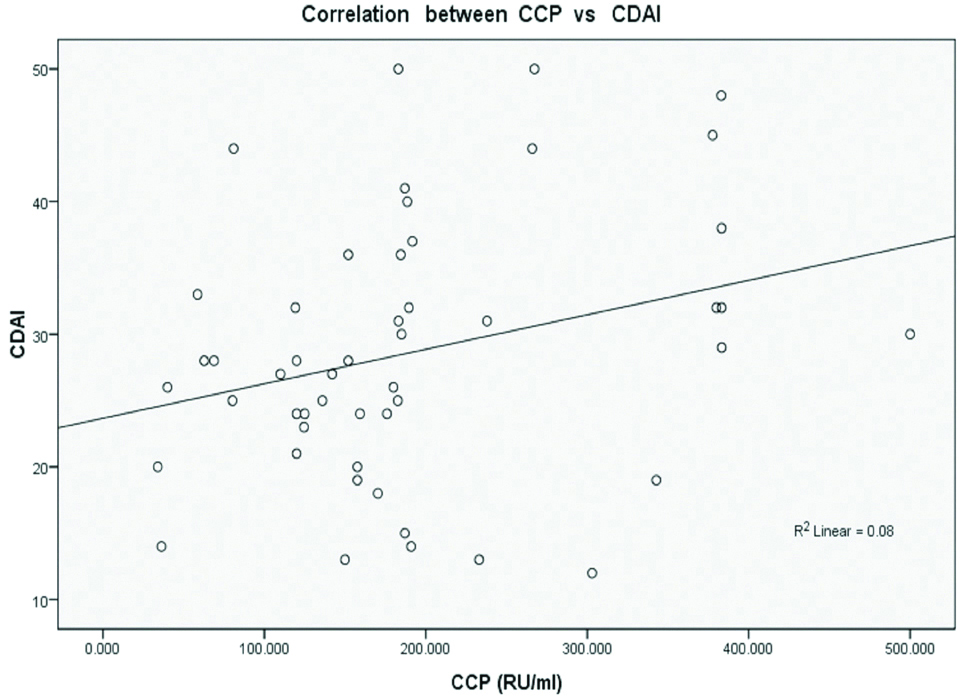 |
| n=50 | Anti-CCP | CDAI | r-value | p-value |
| Mean | 184.347 | 28.94 | 0.08 | 0.029 |
| Std deviation | 114.223 | 10.845 |
Correlation between RF and SDAI (r=0.032, p=0.023).
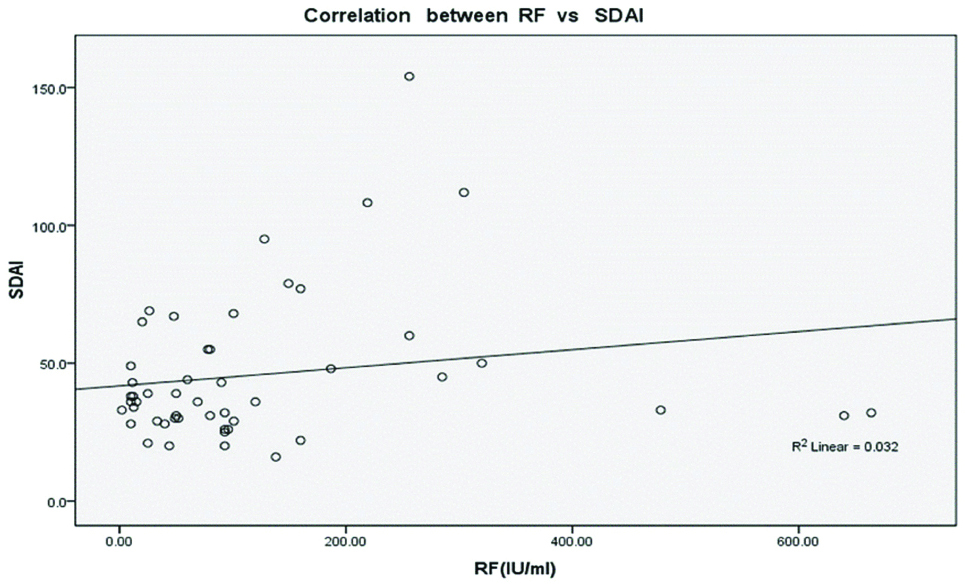 |
| n=50 | RF | SDAI | r-value | p-value |
| Mean | 122.9 | 46.9 | 0.032 | 0.023 |
| Std deviation | 146.85 | 27.156 |
Correlation between RF and CDAI (r=0.032, p=0.023).
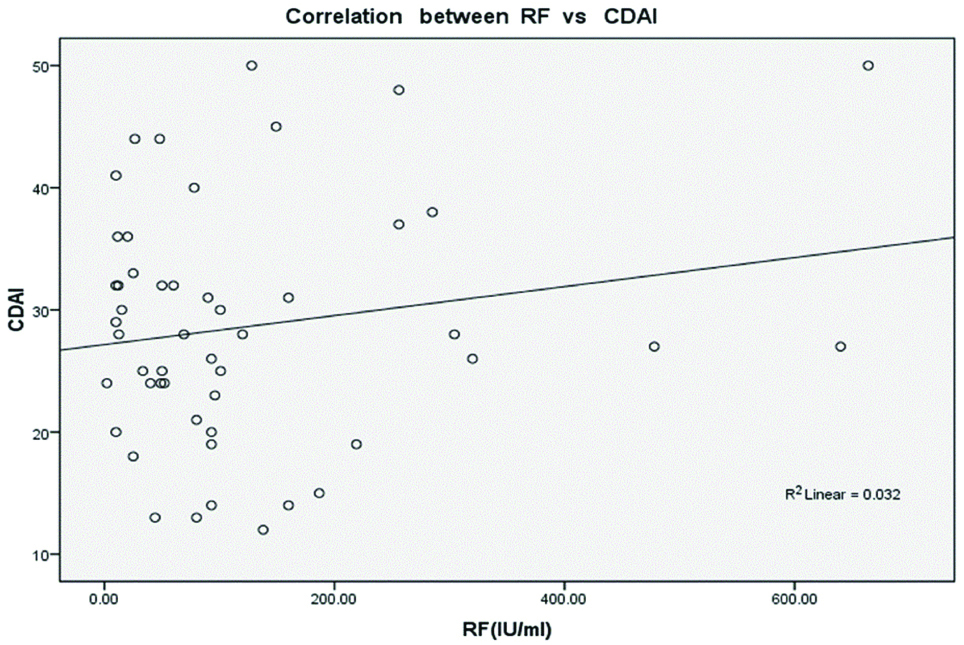 |
| n=50 | RF | CDAI | r-value | p-value |
| Mean | 122.9 | 28.94 | 0.032 | 0.023 |
| Std deviation | 146.85 | 10.845 |
Correlation between RF and DAS-28 (r=0.02, p=0.042).
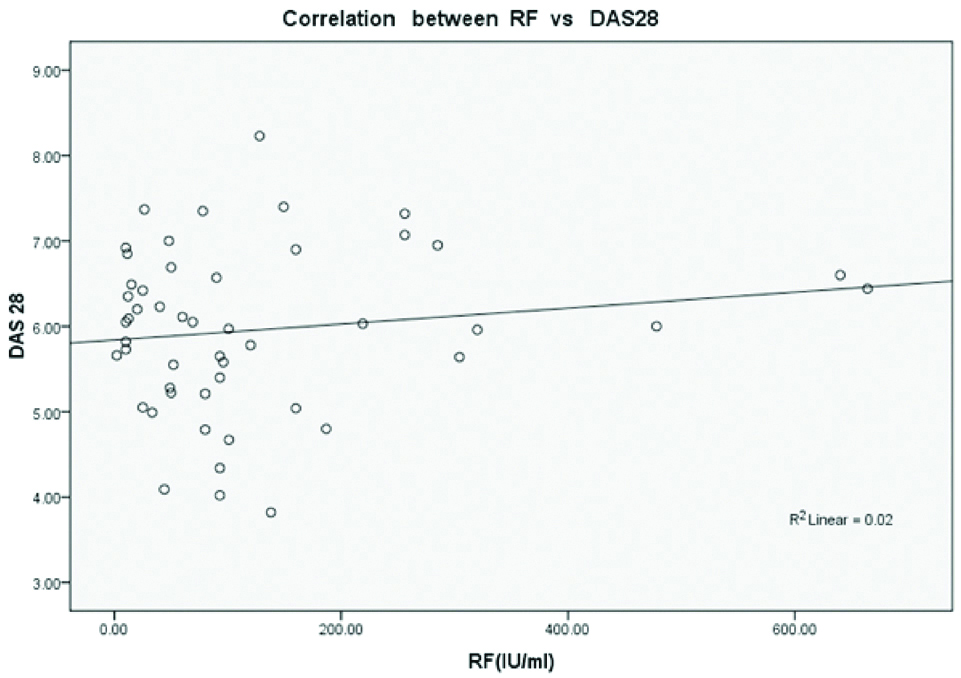 |
| n=50 | RF | DAS-28 | r-value | p-value |
| Mean | 122.9 | 5.955 | 0.02 | 0.042 |
| Std deviation | 146.85 | 0.962 |
Discussion
Rheumatoid factor and Anti-CCP have been used for diagnosis of RA and are present in patients with early RA. Anti-CCP positive patients are also known to have severe erosive disease. We aimed to correlate the severity of the disease in RA and the titres of antibodies of rheumatoid factor and Anti-CCP. The results in our study showed significant correlation between CDAI, SDAI and anti-CCP.
In this study, females were more commonly affected (76%) and with more severe disease. The study by Sieghart D et al., also had female predominance of 72% [13]. The maximum number of patients belonged to the age group, 30-40 and 50-60 years. Most of the patients had RA diagnosed recently (<2 yrs). 18% were rheumatoid factor negative which is similar to what was found by Papadopoulos NG et al., [14].
The present study addresses the issue related to disease and its serological severity. As expected, there was positive correlation among the severity scores, (p<0.0001) between DAS28 and SDAI (r=0.550), CDAI and SDAI (r=0.808). In a study by Glasnović M et al., on 211 patients with RA, they evaluated an anti-CCP titer as a predictive factor for erosive changes and disease activity. They evaluated disease activity by DAS-28 and radiological change by Steinbrocker score. Pearson’s coefficient was 0.479 and ranking correlation coefficient of spearman’s was 0.614 (p<0.0001). However, they did not find any significant correlation between anti-CCP and DAS-28 [15]. In a study by Papadopoulos NG et al., on 135 patients with early stage of RA, those patients who had positive anti-CCP had more tender and swollen joints and so higher DAS-28 (p<0.001). In this study, we found similar results [14]. In a study by Onder B et al., on 61 Patients with RA they evaluated the relation between Anti-CCP positivity and DAS-28 and Serum ferritin. Anti-CCP positivity was associated with higher scores of DAS-28, longer duration of morning stiffness, serum RF positivity and low levels of serum ferritin, while it was not associated with disease duration, VAS, HAQ, ESR, CRP and hemoglobin [16]. This study suggests that anti-CCP positivity was associated with higher scores of DAS-28, which is contrary to what Kuru O et al., in a study of 90 patients of RA found out [17]. They also concluded that level of anti-CCP is higher in RF positive patients. This finding is contrary to this study as the anti-CCP level is similar in those with RF positive and negative patients. Karimifar M et al., showed that the anti-CCP levels were associated DAS-28, and patients with higher VAS scores had higher titers of anti-CCP that is similar to what can be concluded in this study [11]. In another study by Karimifar M et al., they found that the levels of anti-CCP were associated with the severity of disease in those who were rheumatoid factor negative [18].
Sieghart D et al., suggested testing of many autoantibody specificities which will aid in diagnosis and reduces diagnostic duration gap associated with Anti-Citrullinated Protein Antibodies (ACPA) and RF determination [13]. Kastbom A et al., concluded that ACPA antibodies decline rapidly in recent onset RA which correlated with better disease activity and aggressive pharmacotherapy [19].
In general, we found a significant correlation between anti-CCP and disease activity (SDAI, CDAI) (p<0.05). However, this correlation was not enough powerful to use it as a surrogate of disease activity. Instead other factors such as VAS, ESR, and tender joints need to be considered. Disease activity monitoring is an essential part of RA evaluation. It is the basis of on going treatment with disease modifying drugs. There is a need of identification of patients who needs more aggressive treatment than the others. Disease activity measures help in segregating low activity RA from high ones. However, disease activity related titration of treatment is a reactive measure. Titers of anti-CCP have been a predictive factor for erosive RA. It has been found to rise in patients much earlier than clinical symptoms. Thus may aid in deciding aggressive treatment for those more so in early onset RA [20]. The significance of this study lies in filling the void present in the current literature, dealing with the relationship between disease severity and antibody titers. Its value lies in the fact that these antibodies could in fact be used as a marker of severity rather than just diagnosis.
Furthermore, we need to assess each patient at different time span to evaluate to fluctuation of antibody titers. We also need to give each patient individualised care and give more aggressive treatment to those with higher titers of anti-CCP and higher activity scores.
Limitation
There was significant correlation between CDAI and SDAI with anti-CCP. However, there was no correlation between DAS28 and anti-CCP titer, which can be explained due to the small sample size and taking ESR into account which is a nonspecific marker of inflammation compared to CRP which is included in SDAI. Also, the complex methodology required for the calculation of DAS28 makes this interpretation doubtful. Hence, a larger study sample is required to assess the association of DAS28 with anti-CCP titer. Patients on treatment with biologics were not taken into consideration as this was thought to confound the result as the patients with different disease duration were included.
Conclusion
There was significant correlation in the titers of anti-CCP and disease activity indices-SDAI and CDAI. Patients with higher levels of anti-CCP antibody had greater activity. Hence appropriate therapy in those patients with higher titres will be beneficial to the patients. Further studies especially in early onset RA monitoring the titers of antibodies during different treatment phases can be helpful. Prospective studies and RCT’s in this aspect of the disease management will provide a definitive answer in RA management.
*RA=Rheumatoid Arthritis.†MCP-Metacarpophalengeal joint‡ PIP-Proximal interphalengeal joint §IP-Interphalangeal joint ||MTP-Metatarsophalangeal joint **RF-Rheumatoid factor ††Anti-CCP-Anti cyclic citrullinated peptide ‡‡ESR-Erythrocyte sedimentation rate. Note: These criteria are aimed at classification of newly presenting patients who have at least 1 joint with definite clinical synovitis that is not better explained by another disease.
CDAI=Clinical Disease Activity Index; CRP=C-Reactive Protein, DAS28=Disease Activity Score 28 Joints; ESR=erythrocyte sedimentation rate; logn=log-normal; PGA=Patient Global Assessment; PhGA=Physician Global Assessment; SDAI=Simplified Disease Activity Index; SJC=Swollen joint count of 28 joints; TJC=Tender joint counts of 28 joints.