Cone Beam Computed Tomography Analysis of Canalis Sinuosus in Association with an Osteolytic Lesion of Maxilla: A Case Report and Review of Literature
Ritu Tiwari1, Alfred Joseph Ravikumar2, Abhishek Dubey3
1 Consultant, Department of Oral and Maxillofacial Radiology, JSD Techno Dental Imaging Centre, Bengaluru, Karnataka, India.
2 Consultant, Department of Oral and Maxillofacial Surgery, 32 Dental Clinics, Chennai, Tamil Nadu, India.
3 Senior Lecturer, Department of Oral and Maxillofacial Radiology, Maharana Pratap Dental College, Kanpur, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ritu Tiwari, JSD Technodental Imaging Center, 16th Main, 4th ‘T’ Block, Jayanagar-560041, Bengaluru, Karnataka, India.
E-mail: tiwari.ritu28@gmail.com
Canalis Sinuosus (CS) is a frequent anatomical variation arising from the infraorbital canal. It is a neurovascular channel carrying the anterior superior alveolar nerve and vessels. Anterior maxilla is often the site for invasive procedures like implants, supernumerary teeth extraction, impacted canine extractions and periapical surgeries. Knowledge of anatomical variations in this area is of utmost importance to avoid iatrogenic surgical trauma and post-surgical distress to the patient. Although numerous unnamed accessory canals have been reported in the anterior maxilla, there is a lack of literature explaining the exact position, course and significance of CS. The purpose of this article is to increase awareness amongst the clinicians through a CBCT based case report in which CS was identified as an incidental finding in close proximity to an osteolytic lesion of the maxilla. Additionally, a Pubmed-Medline based analysis was also performed with select keywords which revealed 18 relevant results and eight reported cases from 1999 to 2018. This further emphasises the fact that CS is a significant structure that often gets misdiagnosed and conventional radiography fails to display these configurations accurately.
Anterior maxilla, Anterior superior alveolar nerve, Dental implant, Infraorbital canal
Case Report
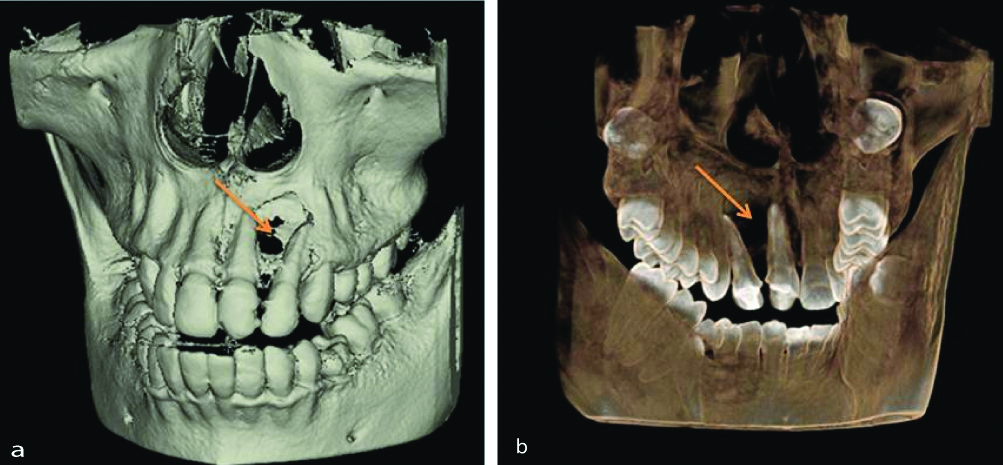
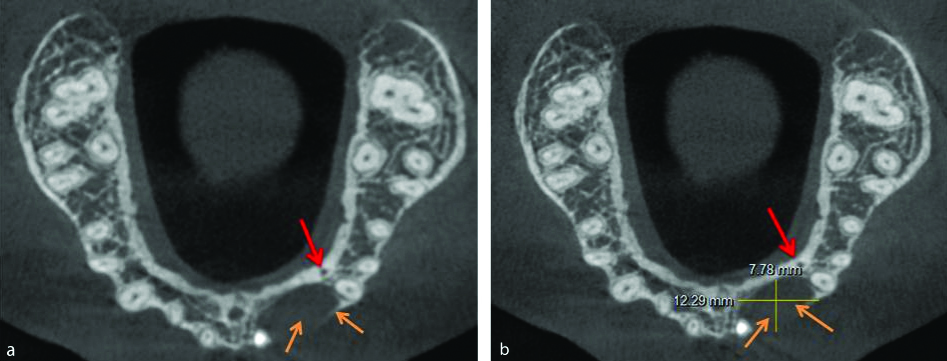
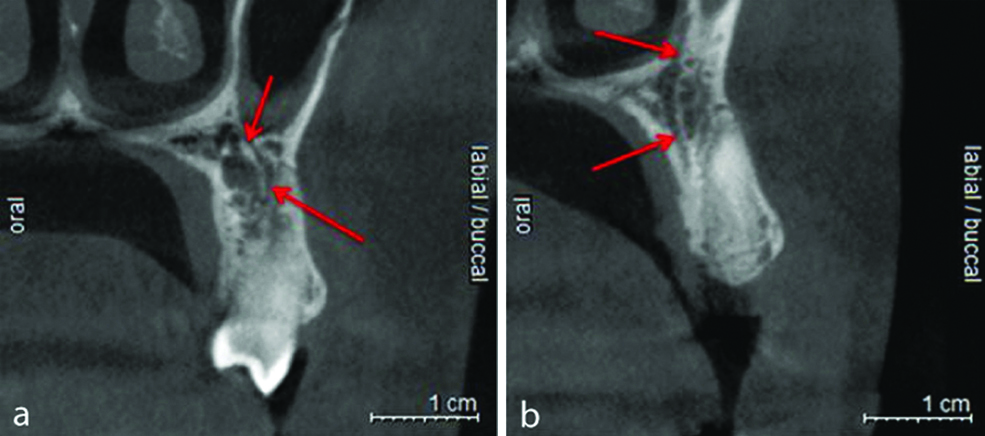
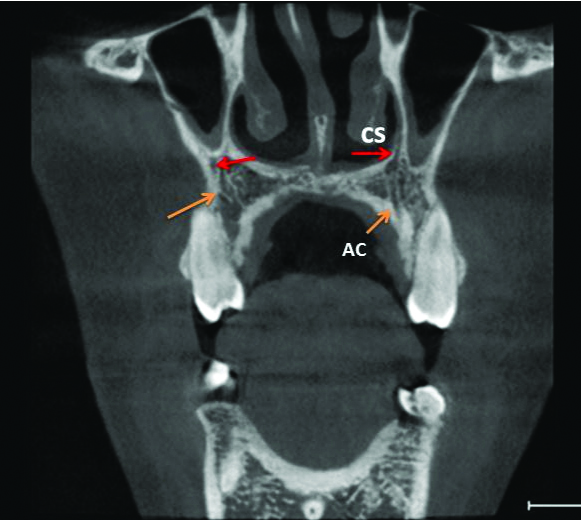
A 21-year-old female was referred to a private radiology clinic for CBCT examination of the anterior maxilla for suspected periapical pathology. The patient reported pain in the left upper jaw since three months. No significant extraoral findings were seen. There was a history of endodontic treatment done with respect to the left central and lateral incisor (teeth number 21 and 22) six months back. On examination, tenderness on percussion and vestibular tenderness were present in the region. A CBCT examination was performed in an Orthophos XG 3D machine (85 kVp, 7 mA) with FOV of 8*8 cm and images were reconstructed into axial, coronal, sagittal planes with Galelios software. A well-defined, roughly oval, unilocular, hypodense lesion was noted in the anterior maxilla extending mediolaterally from the mesial aspect of 23 till distal aspect of 21, superoinferiorly from below the floor of nasal fossa to the middle thirds of the alveolar ridge (in the 21-23 region) and involving the labial and palatal cortical plates. The lesion had regular and non-corticated borders and completely hypodense internal structure. Frank perforation of the labial and palatal cortical plate was noted in the 21-22 regions [Table/Fig-1]. The lesion was in close proximity to the floor of the nasal fossa and appeared to approximate the nasopalatine canal in the region of 21. CBCT also revealed the presence of CS in close proximity to the lytic lesion and located postero-lateral to it. The image of this canal may be observed in transaxial, cross-sectional, coronal and sagittal reconstructions as a wide, hypodense path, adjacent to left canine apex, present under the anterior part of the nasal floor and extending upwards to the anterior nasal wall [Table/Fig-2,3]. CS was also noted on the right side as a linear hypodense track, in the right canine-first premolar region (teeth number 13-14) [Table/Fig-3,4].
3D reconstruction of the maxilla from the anterior a) and posterior b) aspect showing the osteolytic defect (orange arrow) in relation to teeth 21 and 22 with perforated cortical plates.
Axial sections of the maxilla showing the canalis sinuosus (red arrow) on the palatal cortex in close proximity to the posterior-lateral aspect of the lytic lesion (orange arrow) and posterior to the root apex of left canine.
Cross sections depicting the accessory canel of canalis sinuosus (red arrow) reaching the palate posterior to the a) Right maxillary frist pre-molar b) left maxillary canine.
Coronal section at the level of frist premolar depicting the path of canalis sinuosus (red arrow) and its accessory canal (AC) (orange arrow) in association with the floor of nasal fossa.
Radiological differential diagnoses considered for the osteolytic lesion included infected radicular cyst, adenomatoid odontogenic tumour (extrafollicular variant), unicystic ameloblastoma and keratocystic odontogenic tumour. Since, a surgical intervention was planned, it was imperative that the location of CS be kept in mind to avoid neurovascular injury and concomitant paresthesia in the patient and the treating clinician was informed accordingly.
Discussion
Anterior Superior Alveolar Nerve (ASAN) is a branch of infraorbital nerve (given off about 15 mm or more behind the infraorbital foramen) which supplies the incisors, canines and its soft tissues [1,2]. It communicates with the middle superior alveolar nerve and forms the superior dental plexus. The course of the ASAN was first described by Wood-Jones in 1939 [3]. The ASAN is more than one-third the size of the parent trunk and traverses the anterior wall of the maxilla in a distinct bone canal called the CS also termed sinuosus canaliculus or anterior superior alveolar canal owing to its double curved course [1,3,4]. CS originates from the infraorbital canal posterior to the infraorbital foramen and courses in an antero-lateral direction. After reaching the anterior wall of the maxilla, it turns medial to run below the infraorbital foramen crossing the antrum wall from lateral to medial. Once the canal reaches the nasal aperture, it loops inferiorly and descends along the piriform opening [1].
Precise knowledge of the ASAN and CS carries significant clinical implications. With increased popularity of cross-sectional modalities like Cone Beam Computed Tomography (CBCT), visualisation of its pathway and morphology has become a lot easier. Here a case is discussed in which CS was an incidental finding noticed on CBCT examination indicated for suspected periapical pathoses in the anterior maxilla. The clinician was duly notified about the same which in turn aided prudent treatment planning for the patient.
There are a few cases of CS described in literature and even fewer studies describing CBCT based assessment of the canal. Pubmed-Medline based survey for term “canalis sinuosus” “anatomical variations in ASAN” and “CBCT analysis of CS” from 1999-2018 revealed 18 relevant results out of which eight were case reports, making this the ninth case report in this category [Table/Fig-5] [2,5-11].
Pubmed–Medline based survey results for reported cases of Canalis Sinuosus published between 1999-2018 [2,5-11].
| S. No. | Author | Year | Type of examination | Age/Sex of the patient | Findings |
|---|
| 1 | Leven AJ et al | 2018 | IOPA and CBCT | 32/M | Anatomic variation of a neurovascular channel in close proximity to the maxillary right permanent lateral incisor |
| 2 | Shah PN et al | 2017 | IOPA and CBCT | 60/M | Accessory branch of canalis sinuosus mimicking external root resorption in maxillary right central incisor |
| 3 | Arruda JA et al | 2017 | CBCT | 51/F | CS seen as a path adjacent to the upper end of the dental implant and canine apex in the right lateral incisor-canine region. |
| 4 | Rusu MC et al | 2017 | CBCT | 74/M | Multiple accessory canals (ACs) derived from canalis sinuosus, which opened opposite each frontal tooth |
| 5 | McCrea SJJ | 2017 | IOPA, Occlusal and CBCT | 55/F | A well-demarcated canal present between the apex of tooth 23 and the nasopalatine canal |
| 6 | Torres MG et al | 2015 | CBCT | 47/F | Pre operative implant assessment revealed a wide accessory branch from the CS running an intraosseous course in the inferior and posterior direction up to a foramen located in the hard palate, slightly medial in relation to tooth 23 |
| 7 | Neves FS et al | 2012 | CBCT | 54/F | Bilateral accessory canal (anatomical variation of CS) extending adjacent to the maxillary lateral incisor. |
| 8 | Shelley AM et al | 1999 | IOPA | 35/M | Canalis sinuosus manifested as a periapical radiolucency with corticated borders on an upper left canine |
Recent studies have attempted to study the morphology of CS using CBCT. Gurler G et al., reported that the average canal diameter was 1.37 mm and it was significantly larger in males than in females. They also noted accessory canals in 5.4% of the study group with most common location being palatal to the lateral incisors (62.5%) [12]. Orhan K et al., studied 6668 accessory canals found in 1460 CBCT images and it was concluded that maximum accessory canals (44.72%) were seen in the maxillary inter central region which supplemented the results of earlier such studies [13]. Ghandourah AO et al., performed a CBCT based study to assess the frequency, location and width of Accessory Canals (AC) of CS and found out that ACs occurred predominantly in central incisor region in adults from 19-99 years of age and in the left lateral incisor and canine region in the young adults (7-18-year-old) [14].
CS has been classified into seven types based on its emergence possibilities according to their location relative to the teeth/incisive foramen region by de Oliveira-Santos C et al., [15]. These are as follows: central incisor region, between the central and lateral incisor region, lateral incisor region, canine region, first premolar region, lateral to incisive foramen and posterior to incisive foramen. [15,16] In this case, CS was seen in the canine region on the left side and the first premolar region on the right side.
There is no agreement between the distances of the CS from anatomical structures like alveolar bone crest and buccal/labial cortical bone and a discrepancy is observed between the males and females as well as between the left and right sides. Alveolar bone is subjected to morphological changes over time and this could possibly explain this variation [2].
Conventional intraoral radiography techniques (periapical, occlusal radiographs) and orthopantomography depict it as a radiolucent tract in the periapical area of canines and lateral incisors. Superimposition of CS or its accessory channels onto the anterior maxillary teeth may mimic periapical lesions, external root resorptions or other osteolytic lesions [11]. However, with the advent of CBCT, CS can be detected as a hypodense path in the anterior maxilla. As a rule, it should be evaluated in the CBCT examinations indicated as a part of pre-operative implant site evaluation, surgical extractions and in relation to the periapical lesions. Hence, we would like to stress upon the use of a proper radiographic technique like CBCT which can clearly delineate this anatomic structure.
Conclusion
This case reinforces the fact that the knowledge of critical anatomical structures like ASAN and its bony associate (canalis sinuosus) is extremely valuable in inferring radiologic outcomes in the anterior maxilla. Additionally, anatomical variations can often be ambiguous and thus mandate a careful evaluation to realise the treatment needs. This article is an attempt to alert and guide the professionals towards this often present but commonly ignored anatomical variation in order to elude the post-surgical neurovascular complications.
[1]. Von Arx T, Lozanoff S, Anterior superior alveolar nerve (ASAN)Swiss Dent J 2015 125(11):1202-09. [Google Scholar]
[2]. Arruda JA, Silva P, Silva L, Álvares P, Silva L, Zavanelli R, Dental implant in the canalis sinuosus: a case report and review of the literatureCase Rep Dent 2017 2017:481012310.1155/2017/481012328928992 [Google Scholar] [CrossRef] [PubMed]
[3]. Jones FW, The anterior superior alveolar nerve and vesselsJ Anat 1939 73(4):583-91. [Google Scholar]
[4]. Song WC, Kim JN, Yoo JY, Lee JY, Won SY, Hu KS, Microanatomy of the infraorbital canal and its connecting canals in the maxilla using 3-D reconstruction of microcomputed tomographic imagesJ Craniofac Surg 2012 23(4):1184-87.10.1097/SCS.0b013e3182587a4f22801121 [Google Scholar] [CrossRef] [PubMed]
[5]. Leven AJ, Sood B, Pathosis or additional maxillary neurovascular channel? A case reportJ Endod 2018 44(6):1048-51.10.1016/j.joen.2018.02.02529680725 [Google Scholar] [CrossRef] [PubMed]
[6]. Shah PN, Arora AV, Kapoor SV, Accessory branch of canalis sinuosus mimicking external root resorption: A diagnostic dilemmaJ Conserv Dent 2017 20(6):479-81.10.4103/JCD.JCD_375_1629430105 [Google Scholar] [CrossRef] [PubMed]
[7]. Rusu MC, Sandulescu M, Bichir C, Muntianu LAS, Combined anatomical variations: The mylohyoid bridge, retromolar canal and accessory palatine canals branched from the canalis sinuosusAnn Anat 2017 214:75-79.10.1016/j.aanat.2017.07.00628823708 [Google Scholar] [CrossRef] [PubMed]
[8]. McCrea SJJ, Aberrations causing neurovascular damage in the anterior maxilla during dental implant placementCase Rep Dent 2017 2017:596964310.1155/2017/596964328785491 [Google Scholar] [CrossRef] [PubMed]
[9]. Torres MG, de Faro Valverde L, Vidal MT, Crusoé-Rebello IM, Branch of the canalis sinuosus: a rare anatomical variation-a case reportSurg Radiol Anat 2015 37(7):879-81.10.1007/s00276-015-1432-925616849 [Google Scholar] [CrossRef] [PubMed]
[10]. Neves FS, Crusoé-Souza M, Franco LC, Caria PH, Bonfim-Almeida P, Crusoé-Rebello I, Canalis sinuosus: a rare anatomical variationSurg Radiol Anat 2012 34(6):563-66.10.1007/s00276-011-0907-622134775 [Google Scholar] [CrossRef] [PubMed]
[11]. Shelley AM, Rushton VE, Horner K, Canalis sinuosus mimicking a periapical inflammatory lesionBr Dent J 1999 186(8):378-79.10.1038/sj.bdj.480011610365458 [Google Scholar] [CrossRef] [PubMed]
[12]. Gurler G, Delilbasi C, Ogut EE, Aydin K, Sakul U, Evaluation of the morphology of the canalis sinuosus using cone-beam computed tomography in patients with maxillary impacted caninesImaging Sci Dent 2017 47(2):69-74.10.5624/isd.2017.47.2.6928680842 [Google Scholar] [CrossRef] [PubMed]
[13]. Orhan K, Gorurgoz C, Akyol M, Ozarslanturk S, Avsever H, Folia Morphol (Warsz). An anatomical variant: evaluation of accessory canals of the canalis sinuosus using CBCTFolia Morphol (Warsz) 2018 77(3):551-57.10.5603/FM.a2018.000329345719 [Google Scholar] [CrossRef] [PubMed]
[14]. Ghandourah AO, Rashad A, Heiland M, Hamzi BM, Friedrich RE, Cone-beam tomographic analysis of canalis sinuosus accessory intraosseous canals in the maxillaGer Med Sci 2017 15:Doc 20 [Google Scholar]
[15]. De Oliveira-Santos C, Rubira-Bullen IR, Monteiro SA, León JE, Jacobs R, Neurovascular anatomical variations in the anterior palate observed on CBCT imagesClin Oral Implants Res 2013 24(9):1044-48.10.1111/j.1600-0501.2012.02497.x22587228 [Google Scholar] [CrossRef] [PubMed]
[16]. Manhães Júnior LR, Villaça-Carvalho MF, Moraes ME, Lopes SL, Silva MB, Junqueira JL, Location and classification of Canalis sinuosus for cone beam computed tomography: avoiding misdiagnosisBraz Oral Res 2016 30(1):e4910.1590/1807-3107BOR-2016.vol30.004927119586 [Google Scholar] [CrossRef] [PubMed]