Hyponatremia, a very common electrolyte disorder in clinical medicine, most frequently occurs in elderly in-patients [1-3]. It is defined as s. Na+ level of <135 mEq/L and observed to be occurring in 15-30% of hospitalised patients. However, in elderly patients, the prevalence rate has been reported to be even higher up to 50% [3-5].
Ageing results in impairment of water-excretory capacity due to decreased GFR, reduction in total body water content, higher sensitivity to osmotic stimuli, and associated with multiple comorbidities and exposure to multiple drugs [6-10]. Besides, low salt diet followed by many elderly patients and hypoproteinemia due to background illness or malnutrition may also contribute to hyponatremia in this age group [11]. Therefore, ageing itself is considered a significant risk factor for hyponatremia.
Hyponatremia can be of three types-hypertonic hyponatremia, isotonic hyponatremia or hypotonic hyponatremia. Hypotonic hyponatremia is the most common type encountered in clinical practice and further categorised in three-ways based on patient’s volume status- hypervolemic, euvolemic and hypovolemic. Hyponatremia, resulting from hyperlipidemia, paraproteinemia is pseudohyponatremia [12].
Clinical manifestations of hyponatremia count on multiple factors like the duration of the development of symptoms, severity of the decline in sodium level and the patient’s overall health [13]. Mild hyponatremia usually remains asymptomatic and GI manifestations occur with s. Na+ ~ 125 mEq/L. As the s. Na+level fall further CNS symptoms such as confusion, lethargy, focal neurologic deficits, disorientation and agitation usually manifest. Severe neurologic features such as seizure and coma are usually seen when the sodium level falls acutely (<48 hours) below 115 mEq/L [12].
Mild chronic hyponatremia can cause gait impairment, attention deficit, increased risk of falls and osteoporosis [14,15]. Patients with chronic hyponatremia usually develop neurologic symptoms when sodium level falls below 110 mEq/L due to acute exacerbation [16].
Despite being a treatable condition, hyponatremia is associated with prolonged hospital stay and increased mortality rate [10,17].
The present study aimed to determine the prevalence, common aetiologies, comorbids and clinical outcomes of hospitalised hyponatremic elderly patients.
Materials and Methods
A prospective, observational study was carried out over a 12 month period from August 2017 to July 2018 in a teaching hospital. Ethical Committee approval and informed consents were taken prior to the study. All patients of 60 years and above, admitted to the Post-graduate Department of Medicine were included in the study and 950 elderly patients admitted during the period were studied. Detailed history and thorough clinical examination were done. Clinical data including demographics, presenting symptoms, comorbid, drug history, clinical examination findings, volemic status, laboratory investigations, treatment and final outcome were recorded. Patients with pseudohyponatremia and hypernatremia were excluded.
Investigations included complete haemogram, renal function test with serum uric acid, liver function test, blood glucose, routine urine examination, electrolytes, lipid profile, thyroid function test, morning serum cortisol. Imaging studies (chest radiograph, ultrasonography of abdomen and pelvis, CT Scan of brain), ECG, echocardiogram were done in patients when indicated clinically to detect further comorbid conditions and aetiologic factors. Serum sodium and urine sodium were measured by ion sensitive electrode method. Serum osmolality and urine osmolality were measured by freesing point depression osmometer. Hyponatremia was defined in patients having serum Na+ level of <135 mEq/L. The hyponatremic patients were further classified into hypo-, hyper-and eu-volemic groups based on the clinical findings of their volemic status. Multifactor aetiology was defined when more than one factor, known to cause hyponatremia were present simultaneously in a patient. Severe sepsis was defined as confirmed or suspected infection with hypofunction of distant organ [18] and Syndrome of Inappropriate Anti Diuretic Hormone (SIADH) was diagnosed by ‘Bartter and Schwartz criteria’ [19].
Statistical Analysis
All the data were analysed by using statistical package SPSS, version 20.0. Data were first analysed for normal distribution by Kolmogorov- Simrinov, Q-Q Plot, Histogram and then Independent t-test, Wilcoxon rank sum (Mann-Whitney U) test, Pearson’s chi-squared test and Fisher-exact test were used as applicable, to compare the variables. The p-value of <0.05 was of statistical significance.
Results
Out of total 950 elderly patients studied, 32 patients (six patients of hypertriglyceridemia, one multiple myeloma, 11 patients with hypernatremia and 14 patients with hyperglycaemia) were excluded. Of the remainder 918 patients, 478 (52.1%) patients had normal serum sodium level (135-145 mEq/L). The mean age of the patients was 69.87±7.94 and 70.0±8.18 in hyponatremic and normonatremic patients, respectively (p=0.815). Females constituted 44.8% in hyponatremic and 45.2% in normonatremic patients group. The baseline parameters of patients in the study groups are described in [Table/Fig-1] and no significant difference was found between the groups, regarding age, sex and BMI.
Baseline parameters and comparison of proportions across the study groups.
| Parameters | Hyponatremic elderly patients | Normonatremic elderly patients | p-value |
|---|
| No. of Patients | N=440 | N=478 | |
| Sex: Female (% of total) | 197 (44.8%) | 216 (45.2%) | 0.899# |
| Age (years) Mean±SD | 69.87 (±7.946) | 70.00 (±8.182) | 0.815@ |
| BMI Mean (±SD) | 22.517 (±4.309) | 22.198 (±4.624) | 0.50@ |
| (Min-Max) | (12.82-38.93) | (11.69-37.31) |
| Comorbid |
| No. of Comorbid Mean (±SD) | 1.46 (±0.92) | 1.04 (±0.90) | <0.001## |
| Absence of Comorbid N (%) | 60 (13.6%) | 148 (31.0%) | <0.001#{OR: 0.352; 95% CI 0.252-0.492} |
| Presence of multiple (≥2) Comorbid | 202 (45.9%) | 137 (28.7%) | <0.001${OR : 2.113; 95% CI 1.608-2.775} |
| Na+level on admission |
| Mean (±SD) | 122.08 (±8.68) | 138.05 (±2.713) | <0.001& |
| (Min-Max) | (94-134) | (135-145) |
| Length of Hospital Stay |
| Median days | 6 | 5 | <0.001& |
| Mean (±SD) | 7.53 (±6.109) | 5.66 (±3.645) |
| Death N (%) | 20 (4.5%) | 19 (4.0%) | 0.669$$ |
Min: Minimum; Max: Maximum; SD: Standard deviation; CI: Confidence interval; OR: Odd ratio
#Pearson Chi-Square test; @Independent ‘t’ test; ##Mann whitney u-test; $Pearson (Mantel-Haenszel test); &Wilcoxon ranksum test; $$Pearson test
Hyponatremia was found in 46.3% of all hospitalised elderly medicine patients, including patients who developed hyponatremia during hospital stay (N=39). The mean sodium level was 122.08±8.68 mEq/L in hyponatremic patients and 138.05±2.71 in normonatremic group (p<0.001). Hypovolemic hyponatremia was most common (42.0%, N=185); followed by hypervolemic (32.5%, N=143) and euvolemic (25.5%, N=112) and 53 patients (12.0%) had satisfied the diagnostic criteria for SIADH. Most of the hyponatremia in the present study, was of multifactorial aetiology (61.8%, N=272). Use of diuretics (28.8%, N=127), acute renal failure (27.9%, N=123), GI loss (15.5%, N=68) were other leading causes. Among the diuretic users, 93 patients (21.1%) were using thiazides and 33 patients (7.5%), loop diuretics. A total of 139 patients had infections out of which 67 (15.2%) patients had severe sepsis. Other aetiologies are described in [Table/Fig-2]. Salt- restricted diet was followed by 47 (10.7%) patients and nutritional hypoalbuminemia (after excluding the underlying diseases causing protein loss) was found in 54 (12.3%) patients with hyponatremia.
Aetiological factors causing hyponatremia in the elderly patients (N=440).
| Aetiologies | No. of patients% (N) |
|---|
| Multifactor | 61.8 (272) |
| Diuretics | 28.8 (127) |
| Acute Renal Failure | 27.9 (123) |
| GI Loss | 15.5 (68) |
| Severe sepsis | 15.2 (67) |
| SIADH | 12 (53) |
| CHF | 7.7 (34) |
| CLD | 5.9 (26) |
| CVA | 7.4) (33) |
| LRTI | 8 (35) |
| SAH | 0.7 (3) |
| Hypothyroid | 2.7 (12) |
| Adrenal insufficiency | 0.9 (4) |
| Low salt intake | 10.7 (47) |
| Hypoalbuminemia (Nutritional) | 12.3 (54) |
GI: Gastrointestinal; SIADH: Syndrome of inappropriate anti diuretic hormone; SAH: Subarachnoid haemorrhage; LRTI: Lower respiratory tract infection; CHF: Congestive heart failure; CLD: Chronic liver disease; CVA: Cerebro-vascula accident
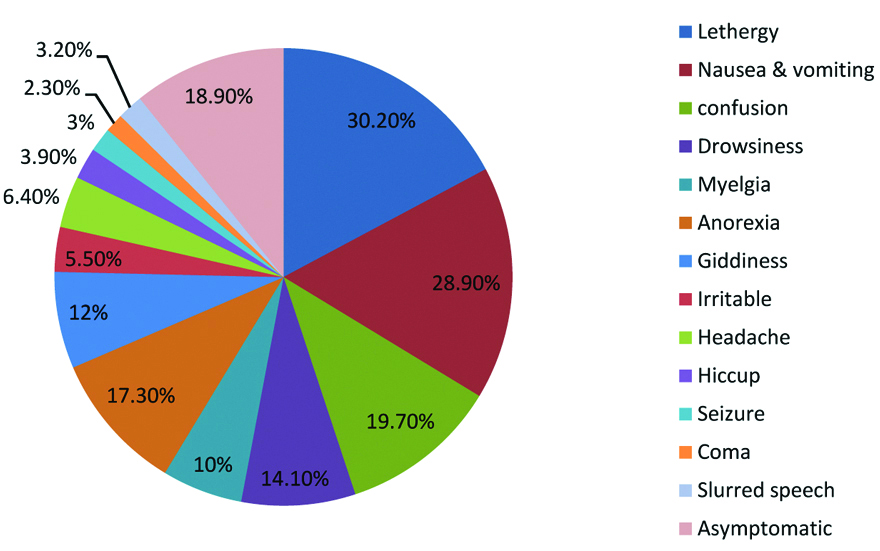
The most common mode of presentation was lethargy (30.2%). Other manifestations included nausea and vomiting (28.9%), confusion (19.7%), drowsiness and impaired consciousness (14.1%). Seizure and coma occurred in 3.0% (N=13) and 2.3% (N=10) of patients, respectively. 13 (3%) patients had fall and fractures in recent past (<6 month). 83 (18.9%) patients had no presenting symptoms attributed to hyponatremia [Table/Fig-3].
Clinical manifestations of hyponatremia patients (N=440).
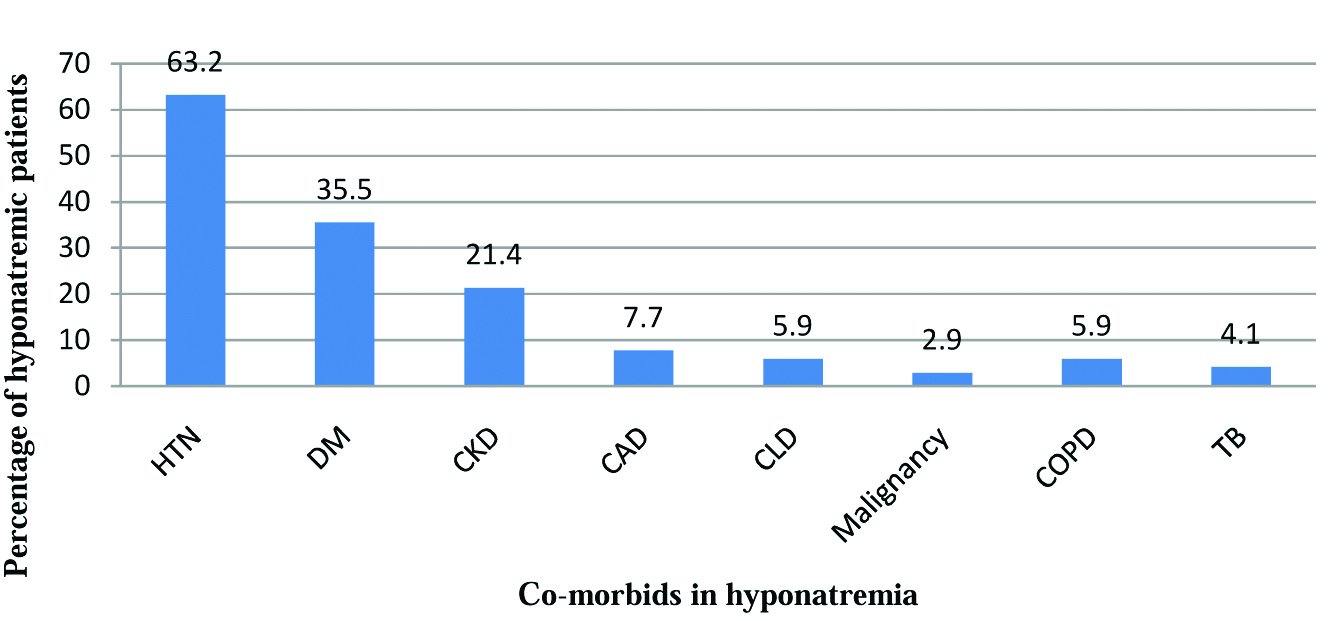
Hypertension was the most common comorbid condition detected (63.2%), followed by Diabetes mellitus (35.5%) and Chronic kidney disease (21.4%) in hyponatremic group. Other comorbid are depicted in [Table/Fig-4]. Absence of comorbid conditions was significantly present in 148 patients (31.0%) in normal serum sodium group of patients (p<0.001). Again, presence of multiple (≥2) comorbid conditions was significantly associated with hyponatremia in elderly patients (p<0.001, OR 2.113; 95% CI 1.608-2.775) [Table/Fig-1].
Co-morbids associated with hyponatremia study group.
DM: Diabetes mellitus; HTN: Hypertension; CAD: Coronary artery disease; CKD: Chronic kidney disease; CLD: Chronic liver disease; COPD: Chronic obstructive pulmonary disease; TB: Tuberculosis
Excluding the hospital stay in patients discharged against medical advice (N=21 in hyponatremia, N=15 in normonatremia), hyponatremic group had longer hospital stay, mean of 7.5±6.1 days as compared to mean of 5.6±3.6 days in normonatremic group; (median 6 days vs. 5 days) (p<0.001). Regarding outcome of the patients, 20 patients (4.5%) in hyponatremic group and 19 patients (4.0%) in control group died during hospitalisations; bearing no significant difference in mortality rate across the elderly groups (p=0.669). The mortality rate, among mild (s. Na+ level of 126-134 mEq/L), moderate (116-125 mEq/L) and severe hyponatremia (≤115 mEq/L) were 2.7% (N=5), 8.0% (N=12) and 2.8% (N=3), respectively (Fisher’s-exact test, p=0.06). Female (3.5%) versus male (5.3%) had died in hyponatremic group; whereas in control group, female 4.1% vs. male 3.8%.
Discussion
The prevalence of hyponatremia in this study was 46.3% of all elderly medicine in-patients. Miller M et al., study revealed 53% of elderly in-patients aged 60 years and above, had hyponatremia over 12 months [20]. Other studies also observed the prevalence of hyponatremia in almost 50% of geriatric admissions [4,5]. In one Asian study, Siregar P, described the prevalence ratio of 2.79 for elderly compared to young group in hospitalised patients [21].
The slight male preponderance in this study is consistent with other recent studies of hyponatremia in elderly [22,23]. Similar to the study by Gill G et al., our study also had no sex difference between the two groups [24].
Hypovolemic hyponatremia was predominantly observed (42%). Cumming K et al., as well found 69.7% of hyponatremia due to dehydration and apprehended it could be ‘frequently overlooked and underdiagnosed’ [25]. In elderly, dehydration can be due to various factors including decreased body water content, less fluid intake, injudicious use of diuretics, predisposition to infections or a combination. Currently, there is no biological marker to detect volemic status and solely depends on clinical examination which is a drawback for accuracy in diagnosis, especially in older people [26].
Many previous studies, reported multifactorial aetiology as the most common cause of hyponatremia in elderly (51.3%, 75.3%, 72.7%) [7,25,27]. The present study, equate their findings by observing 61.8% of patients having multifactor in hyponatremic group. The other leading cause of hyponatremia in the present study was diuretics; of which the most frequent association being thiazides (21.5%). Liamis G et al., depicted thiazide as one of the commonest cause of hyponatremia in elderly [11]. Hypertension being the most frequent comorbid associated with elderly and widespread prescription of thiazide make the thiazide induced hyponatremia described as a ‘silent epidemic’ [28]. Euvolemic hyponatremia was found in 25.5% of patients and SIADH was diagnosed in 12% of cases in the present study reflecting it, as not a leading cause of hyponatremia in the elderly patients. Soiza RL et al., in their study, also pointed out the possibility of SIADH being over diagnosed in previous studies, especially in dehydrated elderly people [26].
Comorbid conditions are commonly present with the geriatric population and associated with hyponatremia in elderly patients. Mohan et al, in their study found 73% of hyponatremic patients had comorbid [29]. Similarly, in the present study 86.4% of patients in hyponatremic group had comorbid as compared to 69% in normonatremic group which is statistically significant (p<0.001). Moreover, the present study also observed the presence of multiple comorbid condition as a significant risk factor for development of hyponatremia in elderly (OR 2.113, 95% CI 1.608-2.775, p<0.001).
In Chua M et al., study, the median length of hospital stay was 13 days and concluded that hyponatremia was strongly associated with longer hospital stay [10]. Authors found the median length of stay at six days (range: 1-52 days) in hyponatremia group in comparision to five days (range: 1-25) in normonatremic group with statistical significance (p<0.001).
However, authors could not find statistically significant difference in mortality across both the group though presence of underlying comorbid was a significant factor for hyponatremia; which may be an important limitation of the present study. Though, authors found a markedly high 8% of mortality in moderate hyponatremia than mild and severe hyponatremic patients (2.7%, 2.8%); was also statistically not significant (Fisher’s-exact test, p=0.06). However, Chawla A et al., studied overall mortality rate among 45,693 hospitalized patients with hyponatremia (<135 mEq/L) compared with 164,146 patients with s. Na >135 mEq/L and concluded that severity of underlying illnesses rather than severity of hyponatremia is the responsible cause for death; propitiating the present findings [30]. Furthermore, Asadollahi K et al., found no consistent association of death with hyponatremia, after reviewing many literatures and analysing mortality pattern of 12 different studies [31].
Limitation
The present study did not measure serum sodium level of patients on daily basis. Hence, the true incidence of hyponatremia in patients during hospitalisation may be higher than the present report. Prognosis of hyponatremia in elderly patients, in terms of mortality rate, may be affected by confounding factors and age itself may be a confounder. To confer prognosis precisely, therefore, requires further statistical analysis like large scale regression analysis, which is another limitation of the present study. However, a large sample size and an appropriately matched control group for comparison, strengthen the present study.
Conclusion
Nearly half of the elderly patient has hyponatremia on admission and hypovolemic hyponatremia is a frequent type. Multifactorial aetiology is the most common cause and other leading causes are diuretic use, renal failure, and infection. Low salt intake and nutritional hypoalbuminemia, in combinations with other factors, also contribute to hyponatremia in elderly. Comorbids are often present in elderly patients and a significant risk factor for hyponatremia; especially the presence of multiple comorbids. Hyponatremia, in elderly patients certainly causes longer hospital stay but association with higher mortality rate is inconsistent, and needs further extensive study.
Min: Minimum; Max: Maximum; SD: Standard deviation; CI: Confidence interval; OR: Odd ratio
#Pearson Chi-Square test; @Independent ‘t’ test; ##Mann whitney u-test; $Pearson (Mantel-Haenszel test); &Wilcoxon ranksum test; $$Pearson test
GI: Gastrointestinal; SIADH: Syndrome of inappropriate anti diuretic hormone; SAH: Subarachnoid haemorrhage; LRTI: Lower respiratory tract infection; CHF: Congestive heart failure; CLD: Chronic liver disease; CVA: Cerebro-vascula accident