Harnessing the Strengths of the Mentored Student Project to Compile a Handbook of Case Scenarios for Undergraduate Medical Students
Maya Roche1, Shashikiran Umakanth2, Ronald A Roche3, Farizal Bin Rizal4, Jaslyn Yeap Wen Xin5, Nuwani Pradeepika Serasinha Pathirana6, Dan Chiu Ping7, Kruthika Jaisankar8
1 Professor, Department of Biochemistry, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Professor and Head, Department of Medicine, TMA Pai Hospital, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
3 Professor, Department of Microbiology, Malabar Medical College, Kerala University of Health Sciences, Calicut, Kerala, India.
4 MBBS Student, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
5 MBBS Student, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
6 MBBS Student, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
7 MBBS Student, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
8 MBBS Student, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Maya Roche, Department of Biochemistry, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
E-mail: maya.roche@manipal.edu
Introduction
To be trained as problem-solvers, medical students need to be exposed to activities that integrate and apply knowledge. Student research projects in the medical curriculum are a means of achieving these objectives. At Melaka Manipal Medical College (MMMC), the Mentored Student Project (MSP) is a platform for research by students guided by a teacher-mentor. The MSP lends itself to innovative ideas to empower students for the future.
Aim
To use the MSP as a platform, to compile a handbook of case scenarios for medical students.
Materials and Methods
To construct the case scenarios, students (n=5) chose various medical topics (n=50), which were familiar to them from their curriculum of the first and second year. They were instructed to refer to authentic online and offline sources of medical literature. After ‘Turnitin’ analysis to check for plagiarism, the case scenarios were vetted by a clinician based on a questionnaire and compiled into a handbook. Students also presented a poster about the MSP experience. MCQ test designed by the faculty was used to as certain learning of the participants of the MSP (n=5) and performance was graded. A questionnaire on a Likert’s scale was used to analyse the students’ engagement with the MSP. Individual and focus group discussions to ascertain students’ opinion were also held.
Results
The study demonstrated that students were capable of designing case scenarios of good quality free of plagiarism. They scored between 60-70% in the MCQ test providing evidence of substantial knowledge retention. They felt that the experience had integrated their knowledge and would help them in problem-solving.
Conclusion
The evidence from this study brings to light the multifaceted role that MSPs play in the personal and professional development of medical students.
Critical thinking, Medical curriculum, Personal and professional development, Problem solving
Introduction
Ausubel DP, the famous American psychologist stated in his Subsumption Theory that learning is influenced by an individual’s existing cognitive structure which is a sum of organisation, stability and clarity of knowledge in a particular subject. This is the cardinal principle that determines learning and retention of new knowledge. It is in this context that relating new ideas to a student’s existing knowledge base becomes important. As personal development is a component of effective learning, students must take responsibility for this process and adopt an active and collaborative approach with their teachers or tutors [1,2]. Active learning promotes critical thinking and knowledge retention [3,4]. Student research projects are a mode of active learning [5] and are included in the curricula of most educational institutions all over the world.
Studies related to research by medical students indicate that they contribute to developing research-specific skills and competencies. These are needed in evidence-based clinical work and are beneficial for personal and professional development [6]. It also boosts the number of students who choose to engage in research after graduating from medical school, encouraging them to become physician-scientists [7]. As scientific research is no longer envisaged as an individual endeavour, but a collaborative, interdisciplinary activity, it is imperative that research activities for students should also reflect this trend. In the Indian scenario, there is no provision to engage undergraduate medical students in research. To address these issues in medical education and with the primary intention of inciting scientific curiosity among undergraduate students, a MSP was introduced into the curriculum at MMMC in 2008 [8].
The MSP is a research project carried out under the guidance of a teacher-mentor and as with any research activity, identifying a research problem, conducting a literature review, planning and conducting the experiments, documenting and analysing the results and drawing conclusions are basic components. The strengths of MSPs are that the students are guided by a teacher-mentor, have access to resources of the University in terms of text and digital media, laboratories, statistical support and possible collaborations for interdisciplinary research with numerous other institutions in the campus. At the end of the study, students are expected to tabulate the findings and present it in the form of a poster on the presentation day assigned by the institution. They are not allowed to proceed to the clinical phase of the programme unless they complete this activity.
The doctor’s profession constantly draws upon problem-solving skills. To inculcate problem-solving skills, case-scenarios or triggers are used as training instruments in medical curricula the world over [9,10]. These are invariably designed by a team of experts and reflect the curricular needs of the programme in question and are relevant to the social context [11,12]. In an earlier study at MMMC in 2016 [13], it was demonstrated that students of first-year MBBS course were able to design case-scenarios when provided with adequate study material and guidance by the teacher. These students were novices, the experiment was confined to a single topic and ended with evaluation of the cases designed and student feedback. The students who took part felt that it markedly enhanced comprehension, critical thinking, and clinical orientation to the topic and found it was a good strategy for active learning. Bolstered by the positive outcome, a larger study was planned with multiple topics, wherein the strengths of the MSP would be used not only to design case scenarios and a poster presentation, but also to compile a handbook for publication.
Primary Aim
To use the MSP as a platform, to compile a handbook of case scenarios for medical students, which can be used in Problem-Based Learning (PBL) or Case-Based Learning (CBL) sessions.
Secondary Aim
To train students to gather and use information from digital and text media.
To test students’ knowledge on the topics addressed in the case scenarios by administering an MCQ test and to include the MCQ section in the handbook.
To summarise the findings of the MSP experience and present it as a poster.
Materials and Methods
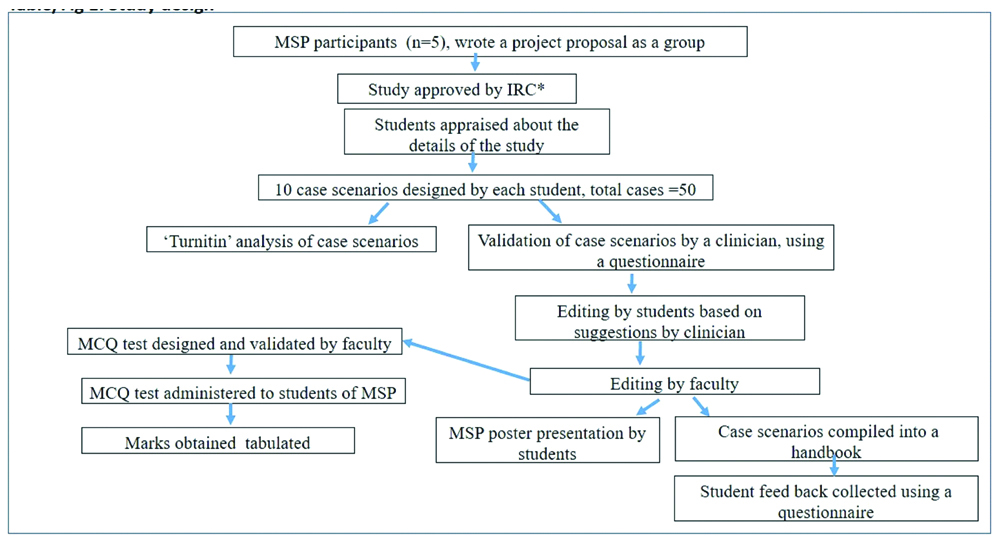
This experimental study was taken up as part of the MSP which is a compulsory research activity for students in the third-semester of the MBBS programme, to be carried out under the guidance of their teacher-mentors. The entire batch of MBBS students was divided into groups of five and each group was allotted a research project by their respective mentors. The students were familiar with their teacher-mentor for more than a year prior to the study, since they were assigned to the mentor, as soon as they joined the institution. Students were already exposed to PBL, in the previous two semesters and had a basic knowledge of anatomy, physiology and biochemistry. All the students had to compulsorily undertake a research project, (there were no exclusions) since it was a curricular requirement for their promotion to the clinical semester. In the MSP study reported here, a control group could not be accommodated because the study design required that all students take part in the research activity. The study design was explained to the students (n=5) in the MSP group and is shown in the chart [Table/Fig-1]. Students were asked to nominate one among them as their leader to serve as a conduit between the group and the teacher-mentor. As expected by the institution, they wrote a brief description of the project and submitted it to the Institutional Research Committee (IRC) which approved the study. Since the MSP required inputs from clinical and paraclinical sciences, the teacher-mentor requested the participation of another faculty, a senior clinician, i.e., Head of the Department of Medicine, for validating the case scenarios and a medical microbiologist for designing the MCQ test for the students.
Study design.
*Institutional Research Committee
The study spanned a period of six months from January to June 2018. Various medical topics (n=50), which were somewhat familiar to the students from their curriculum in the first and second year, were chosen by the students themselves. These topics were from haematology, neurology, infectious diseases, endocrinology, paediatrics, cardiology, immunology and others. Each student selected ten topics on which to design the case scenarios. They were asked to confine themselves to authentic online sources of medical literature such as Medscape, WebMD, Mayo Clinic and PubMed and also to standard textbooks of medicine such as Robbins and Cotran-Pathologic Basis of Disease. They were also given reference articles on case scenario design [11]. Four weeks’ time was allotted for designing the case scenarios, following which the students emailed the cases to the mentor. As a guideline for vetting by the clinician, a questionnaire on a five-point Likert’s scale with 15 items was designed and was validated by a member of the medical education department of the University. Subsequently, the case scenarios (n=50) were organised as five separate files, each file consisting of 10 case scenarios designed by a single student. They were emailed to the Head of the Department of Medicine of the hospital affiliated to the University for vetting along with the questionnaire mentioned above. The clinician was also asked to give his comments on the changes to be made in the content of the case scenarios and also express his opinion on the various attributes of the activity. The five sets of case scenarios were subsequently subjected to ‘Turnitin’ analysis in the University library, to assess the similarity index to measure plagiarism. A similarity index of <15% was considered to be acceptable.
To assess student learning in the activity, an MCQ test was formulated by the faculty using the course objectives of the first and second year MBBS. To validate the construct and content of the test, it was administered to two faculty colleagues, teaching the pre and paraclinical sciences. The questions which needed modification were identified and reformulated. The final validated MCQ test was of the single best answer type with four options given. It consisted of 150 questions, with 3 questions addressing the content in each case scenario. The MCQ test was administered to students who took part in the MSP, with a time limit of 75 minutes. Students used their laptops to answer the test and results were expressed as percentages. A questionnaire using a five-point Likert’s scale was used to analyse the students’ experience with the MSP. In addition to this, individual and focus group discussions to ascertain students’ opinion on the outcome of the study were also held. These discussions were held in an informal atmosphere and no questionnaires were used. In the discussions with individual students, they were asked whether group dynamics worked, the usefulness of this activity for medical students and whether the study contributed to their personal and professional development. For the focus group discussion, all the five students were interviewed as a group and asked about their experience while using digital media for case scenario design and whether they would take up research during future academic endeavours.
Results
The [Table/Fig-2] shows some of the cases designed by the students and subsequently vetted by the clinician along with the corresponding MCQs designed by the faculty.
Cases designed by students with corresponding MCQs designed by faculty.
| 1. Katie, The Lazy baby girl | Test yourself (MCQs) |
| A two-year-old baby girl, Katie was brought to the hospital by her parents. The doctor noticed that she had bow legs and her costochondral junctions had a beaded appearance. She had a pot belly and a protruding forehead. She had not yet attempted walking. Tenderness was elicited at wrists and ankles. The baby girl had minimal exposure to the sun and had been breastfed without being given any other supplements. | The least likely risk factor for rickets is: A. Prematurely born child B. Darkly pigmented child C. Child on supplemental milk formulae D. Child with limited sun exposure |
| Laboratory report showed that her vitamin D3 level was 15 ng/mL (normal range is 30-50 ng/mL) and parathyroid hormone was 75 pg/mL (normal range:10-65 pg/mL) with low plasma phosphorus and calcium. Her X-ray showed that the epiphyses were enlarged. | Vitamin D resistant rickets is also known as: A. Nutritional rickets B. Hypophosphatemic rickets C. Renal osteodystrophy D. Osteomalacia |
| Her parents were advised to give the baby girl 1000 IU of vitamin D supplement daily for six weeks along with more cheese, fortified milk, mackerel, and codfish. Besides, they were also advised to take her outdoor and expose her to sunlight for at least 30 minutes a day between 10 am and 3 pm. | Which of the following is least likely to be due to rickets? A. Gunstock deformity B. Bow legs C. Craniotabes D. Pot belly |
| 2. Shocked looking Amanda |
| A 35-year-old high school teacher, Amanda presented in the hospital with her eyes bulged and swelling in the front of the neck. She also complained of heat intolerance, unintentional weight loss, restlessness, palpitation, and insomnia over the past two weeks. She had reduced menstrual flow with decreased frequency of periods and frequent bowel movement recently. Her physician could also see a mild tremor in her hand, warm moist skin, and brittleness of her hair. | In Grave’s Disease, thyroid stimulating antibodies bind to which of the following? A. Thyroid follicular cytoplasmic antigens B. Parafollicular cells C. TSH receptors D. Thyroglobulin |
| Laboratory investigation showed that her free T4 was 37.8 pmol/L (normal range 11.0-21.0 pmol/L) and free T3 was 21.6 pmol/L (normal range is 3.1-6.0 pmol/L). Serum thyroid stimulating hormone was less than 0.1 mU/L (normal range is 0.5-5.0 mU/L). Further, anti-thyroperoxidase and anti-thyroglobulin antibodies were detectable in her blood. | Which of the following routes is used to administer radioactive iodine? A. Oral B. Subcutaneous C. Intramuscular D. Intravenous |
| The decision was made to treat her with methimazole. | Which among the following is the least likely symptom of Graves’ Disease? A. Weight loss despite increased appetite B. Restlessness, tremors, irritability C. Constipation D. Prominent bulging eyes |
The [Table/Fig-3] shows the questionnaire given to the clinician and grades given by the clinician during assessment of the case scenarios. In general, the clinician agreed that the cases were well constructed; realistic, related to the real-life situation and that the details of clinical investigations provided were adequate. Regarding the outcome of the activity in terms of benefits to students, the examiner thought that it increased knowledge, critical thinking and self-directed learning. The clinician advised a few changes in the case scenarios such as rewording titles, inclusion of X-ray reports wherever relevant, correction of some laboratory values and use of generic names of drugs instead of brand names. Checking for plagiarism in five sets of case scenarios using Turnitin software revealed a similarity index of 0-5%. Preliminary proofreading and editing were done by the students after which grammatical and syntax errors were corrected by meticulous proofreading by the faculty.
Assessment of the case scenarios by the clinician.
| S. No. | Variables | Strongly disagree (1) | Disagree (2) | Neutral (3) | Agree (4) | Strongly agree (5) |
|---|
| Attributes of case design per se |
| 1. | Cases were well constructed | | | | 100 | |
| 2. | Do you feel the title is relevant to the case? (If not, please suggest an alternative) | | | 40 | 20 | 40 |
| 3. | Is the case socially and clinically relevant? | | | | 80 | 20 |
| 4. | Is the case realistic and related to real-life situation? | | | | 80 | 20 |
| 5. | Is the clinical presentation given in the case adequate and significant for the clinical context provided? | | | | 40 | 60 |
| 6. | Are the investigations provided (including laboratory data if any) valid and essential for providing cues necessary for creating a hypothesis about the case/condition? (If NO, what other relevant investigations would you suggest?) | | | | 80 | 20 |
| 7. | Does the case contain sufficient cues that drive the students to useful discussion? | | | | 60 | 40 |
| 8. | Problems are in suitable format (length of text, use of visuals) | | | | 60 | 40 |
| 9. | Problems have suitable clarity | | | | 60 | 40 |
| 10. | Problems are of appropriate difficulty level for undergraduate medical students | | | | 80 | 20 |
| 11. | Does the problem promote teamwork? (as in a PBL session) | | | | | 100 |
| Attributes of outcome of the activity |
| 12. | Expands the knowledge base through active learning | | | | | 100 |
| 13. | Promote self directed learning | | | | 60 | 40 |
| 14. | Stimulate critical thinking | | | | 80 | 20 |
| 15. | Facilitate recall and application of knowledge | | | | 60 | 40 |
Numbers represent the cumulative numerical average of 50 case scenarios
The [Table/Fig-4] shows the results of the questionnaire given to students to assess their opinion on the experience of the study. Students strongly agreed that the activity stimulated recall of prior knowledge there by promoting acquisition of new knowledge, improved critical thinking and promoted self-directed learning. The activity according to them was reasonably enjoyable and was not time consuming. Discussions with individual students revealed that, though there were sometimes disagreements regarding the distribution of work related to compiling the case scenarios and designing the poster, they agreed on keeping deadlines and finishing the task at hand on time. Thus, group dynamics was largely effective and did not have any deleterious effects on creativity and productivity. They felt that the activity usefully engaged medical students by contributing to personal and professional development. In the focus group discussion, students were affirmative that they were motivated to study the relevant topics extensively. They also stated that they had used only specific websites for gathering information as instructed earlier by the mentor. However, they confessed that they did have some degree of difficulty in familiarising themselves with the methodology of case scenario construction and understanding certain terminologies in the websites. Other concerns included not finding proper references for normal range of some metabolites, cross-referencing to find information on topics not very familiar to them and not knowing in what sequence clinical symptoms appear in a disease. In spite of these difficulties, in response to the open ended questions in the questionnaire, one student remarked that the activity could be included for internal assessment, while another asserted that if that was the case, it should be conducted only in the fourth semester. Another student was of the opinion that since case scenario design borrows more directly from real life, it was more interesting than just reading from the textbook. Students also stated that research was interesting and they would definitely include it as a part of academics in the future. In the MCQ test, students scored 60-70% marks which is testimony to the knowledge retained in the topics. Students presented a poster summarising the entire MSP experience on the day assigned by the institution for the purpose. The case scenarios with MCQs were then compiled into a handbook and presented to the audience during poster presentation. The outcome was truly novel and was appreciated by all from within the institution and outside.
| Items of the questionnaire | Strongly disagree (1) | Disagree (2) | Neutral (3) | Agree (4) | Strongly agree (5) |
|---|
| 1. Increased knowledge | | | | | 100 |
| 2. Improved critical thinking | | | | 20 | 80 |
| 3. Activated prior knowledge | | | | | 100 |
| 4. Increased integration of concepts between different subjects | | | 40 | 20 | 40 |
| 5. Improved clinical orientation | | | 20 | 40 | 40 |
| 6. Improved motivation to learn | | | 40 | 20 | 40 |
| 7. Promoted self-directed learning | | | | 40 | 60 |
| 8. Would strengthen problem-solving skills | | | | 40 | 60 |
| 9. The activity was enjoyable | | | 40 | 40 | 20 |
| 10. The activity was difficult | | | 60 | 40 | |
| 11. The activity was time consuming | | 40 | 20 | 40 | |
| 12. Activity required consultation with other group members/peers | | 20 | 20 | 20 | 40 |
The numbers represent cumulative numerical average of opinions expressed by 5 students
Please answer the following†:
1. What are the text and electronic materials you referred to when constructing the case scenarios?
2. Are there any specific difficulties you faced during the activity?
3. Do you feel that case scenario design should be introduced as an activity for internal assessment for medical students in the 4th semester?
*Cronbach alpha=0.73
†Answers to open ended questions are discussed in the paper
Discussion
Student research projects in the medical curricula have been credited with various positive attributes in previous studies [6,14]. Bridging the gap between the availability of information and comprehending it [15], enhancing critical thinking and analytical skills and encouraging self-directed learning, just to name a few. The present study addressed all these aspects of learning successfully. Participation in research projects teaches medical students that clinical care and research should go hand in hand, with the goal of providing more benefit to patients and society [16].
The present study dealt with case scenarios which represent actual clinical situations with patients and as such, it helped students understand the relevance of what was being taught in lectures. Authors are already in an era where technology drives education and information gathering in numerous ways. In this context, it is imperative that students be taught the use of technology for research [17,18]. In this study, students managed the daunting task of collecting the right information from the internet [19] and organising it in a coherent manner. Making students independent learners is the dream of any teacher and this study achieved this goal amicably. Since students had to communicate with their peers in the group and with their mentor on a regular basis, it improved interpersonal communication skills, which are assessed in medical curricula [20]. Since this project had multiple objectives, culminating in the compiling of a handbook, the role of the mentor and the other faculty who took part in the study was substantial. The task of achieving this in a short period of six months using only the free time available for students from their rigorous schedule of the third semester was challenging. Finally, this MSP exemplifies the fact that when students and teachers work in unison, novel outcomes can become a distinct reality.
Limitation
In this activity, due to time constraints, the knowledge gained by students was assessed using only 3 MCQs per case scenario. It would have served the purpose better if the appraisal of knowledge was carried out in a more detailed and comprehensive manner using short answer questions in addition to MCQs.
Conclusion
The evidence from this study brings to light the multifaceted role that MSPs can play in the overall development of the personal and professional lives of medical students. MSPs have the power to make medical students self-learners and responsible individuals. Exposure to the basics of research methodology has the capacity to motivate them to pursue a career in research related to medicine. In this particular case, the MSP had the unique distinction of leading to the compilation of a handbook co-authored by students and faculty. It must be said here in the affirmative that, this MSP was a great success with laudable outcomes and the memory of the enriching experience will be cherished by both students and faculty for a lifetime.
Numbers represent the cumulative numerical average of 50 case scenarios
The numbers represent cumulative numerical average of opinions expressed by 5 students
Please answer the following†:1. What are the text and electronic materials you referred to when constructing the case scenarios?2. Are there any specific difficulties you faced during the activity?3. Do you feel that case scenario design should be introduced as an activity for internal assessment for medical students in the 4th semester?
*Cronbach alpha=0.73
†Answers to open ended questions are discussed in the paper
[1]. Ausubel DP, A subsumption theory of meaningful verbal learning and retentionThe Journal of General Psychology 1962 66(2):213-24.10.1080/00221309.1962.971183713863333 [Google Scholar] [CrossRef] [PubMed]
[2]. Ausubel DP, The psychology of meaningful verbal learning 1963 New YorkGrune & Stratton [Google Scholar]
[3]. Bagnasco A, Cadorin L, Tolotti A, Pagnucci N, Rocco G, Sasso L, Instruments measuring meaningful learning in undergraduate healthcare students: a systematic review protocolJ Nurs Educ 2015 71(3):655-64.10.1111/jan.1252025175546 [Google Scholar] [CrossRef] [PubMed]
[4]. Spencer JR, Anderson KM, Ellis KK, Radiant thinking and the use of the mind map in nurse practitioner educationJ Nurs Educ 2013 66(5):291-93.10.3928/01484834-20130328-0323550549 [Google Scholar] [CrossRef] [PubMed]
[5]. Harirforoosh S, Stewart DW, A descriptive investigation of the impact of student research projects arising from elective research coursesBMC Research Notes 2016 9(1):4810.1186/s13104-016-1865-126817849 [Google Scholar] [CrossRef] [PubMed]
[6]. Möller R, Shoshan M, Heikkilä K, What is the reward? Medical students’ learning and personal development during a research project courseMed Educ Online 2015 Sep 4 :2010.3402/meo.v20.2844126344390 [Google Scholar] [CrossRef] [PubMed]
[7]. Cluver J, Book S, Brady K, Back S, Thornley N, Engaging medical students in research: reaching out to the next generation of physician-scientistsAcad Psychiatry 2014 38(3):345-49.10.1007/s40596-014-0097-824913099 [Google Scholar] [CrossRef] [PubMed]
[8]. Vasudha D, Abraham Reem R, Sachidananda A, Ramnarayan K, Mentored student project for inculcating research skillsMedical Education 2010 44(5):49610.1111/j.1365-2923.2010.03648.x20374456 [Google Scholar] [CrossRef] [PubMed]
[9]. Asad M, Iqbal K, Sabir M, Effectiveness of problem based learning as a strategy to foster problem solving and critical reasoning skills among medical studentsJournal of Ayub Medical College Abbottabad: JAMC 2015 27(3):604-07. [Google Scholar]
[10]. Crawford TR, Using problem-based learning in web-based components of nursing educationNurse Educ Pract 2011 11(2):124-30.10.1016/j.nepr.2010.10.01021111680 [Google Scholar] [CrossRef] [PubMed]
[11]. Azer SA, Peterson R, Guerrero AP, Edgren G, Twelve tips for constructing problem-based learning casesMedical Teacher 2012 34(5):361-67.10.3109/0142159X.2011.61350022452277 [Google Scholar] [CrossRef] [PubMed]
[12]. Wood DF, Problem based learningBMJ 2003 326(7384):328-330.10.1136/bmj.326.7384.32812574050 [Google Scholar] [CrossRef] [PubMed]
[13]. Roche M, Adiga IK, Nayak AG, PBL trigger design by medical students: An effective active learning strategy outside the classroomJ Clin Diagn Res 2016 10(12):JC06-JC08.10.7860/JCDR/2016/21813.901528208882 [Google Scholar] [CrossRef] [PubMed]
[14]. Imafuku R, Saiki T, Kawakami C, Suzuki Y, How do students’ perceptions of research and approaches to learning change in undergraduate research?Int J Med Educ 2015 6:47-55. [Google Scholar]
[15]. Ávila MJ, Rodríguez-Restrepo A, The importance of research in undergraduate medical educationMedwave 2014 14(10):pii e603210.5867/medwave.2014.10.603225587714 [Google Scholar] [CrossRef] [PubMed]
[16]. Zier K, Wyatt C, Muller D, An innovative portfolio of research training programs for medical studentsImmunol Res 2012 54(1-3):286-91.10.1007/s12026-012-8310-x22418729 [Google Scholar] [CrossRef] [PubMed]
[17]. Law JK, Thome PA, Lindeman B, Jackson DC, Lidor AO, Student use and perceptions of mobile technology in clinical clerkships-Guidance for curriculum designAm J Surg 2018 215(1):196-99.10.1016/j.amjsurg.2017.01.03828173937 [Google Scholar] [CrossRef] [PubMed]
[18]. Williamson KM, Muckle J, Students’ Perception of Technology Use in Nursing EducationComput Inform Nurs 2018 36(2):70-76.10.1097/CIN.000000000000039629084028 [Google Scholar] [CrossRef] [PubMed]
[19]. Maroof KA, Parashar P, Bansal R, How are our medical students using the computer and internet? A study from a medical college of north IndiaNiger Med J 2012 53(2):89-93.10.4103/0300-1652.10354923271853 [Google Scholar] [CrossRef] [PubMed]
[20]. Gude T, Grimstad H, Holen A, Anvik T, Baerheim A, Fasmer OB, Can we rely on simulated patients’ satisfaction with their consultation for assessing medical students’ communication skills? A cross-sectional studyBMC Med Educ 2015 15:22510.1186/s12909-015-0508-x26687201 [Google Scholar] [CrossRef] [PubMed]