Materials and Methods
Study Design
A prospective descriptive study was conducted in the department of Radiodiagnosis in Meenakshi Medical College Hospital and Research Institute, Kanchipuram, India from June 2011 to December 2014 based on the MRI findings in patients with Tuberculosis of spinal and paraspinal region. The following MRI sequences-FSET2 Sagittal, SET1 Sagittal, FSET2 Axial, SET1 Axial sequences were done in all cases with additional FIR (Fat Suppressed) and SET1 Coronal sequence wherever required.
Inclusion Criteria
Patients diagnosed with tuberculosis of spinal and paraspinal region by Fine needle aspiration cytology/Histopathology/serology/CSF examination not involving the bony components on MRI were included in the study.
Exclusion Criteria
Patients with involvement of bony components or typical MRI appearance of Tuberculous spondylitis-involvement of intervertebral disc and adjacent vertebra were not included.
A total of 529 cases of tubercular spinal lesions were diagnosed. Out of which only 43 patients showed atypical features on MR imaging involving only soft tissue without affecting the bony component of spine. Consent was obtained from all the patients to include in the study. The study was cunducted after considering and following all the factors of Declaration of Helsinki.
Results
In the study group of 43 patients, 28 cases were male and 15 cases were female at the ratio of approximately 2:1. Age wise patients were very widely distributed, youngest one was six years and oldest one was 73 years of age.
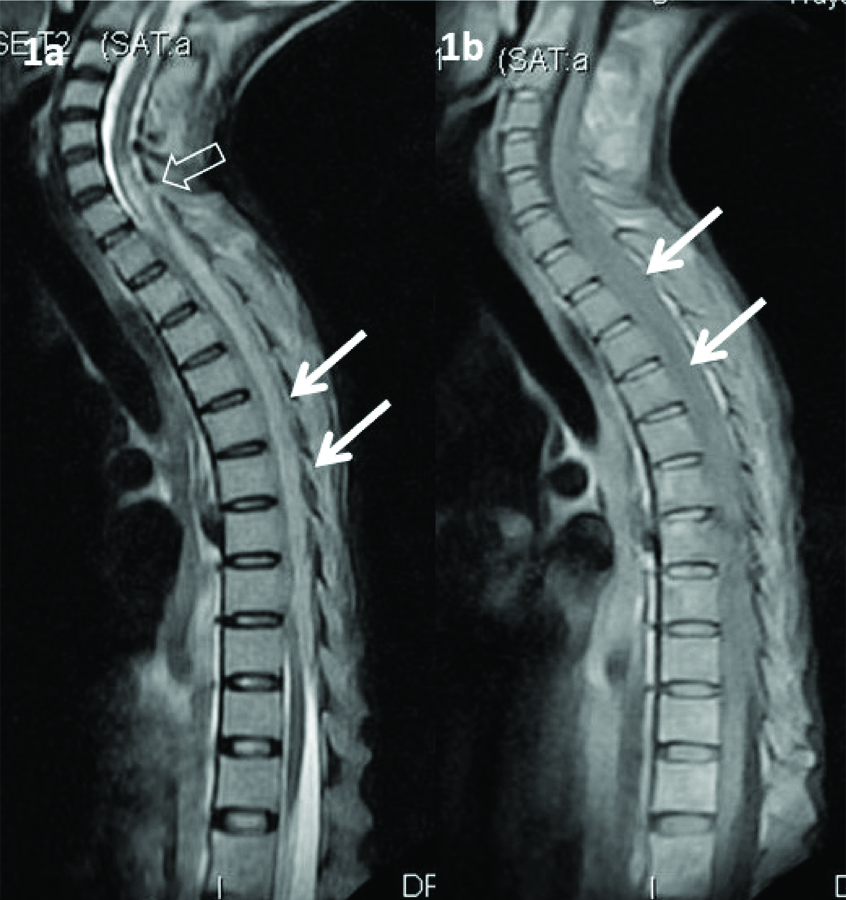
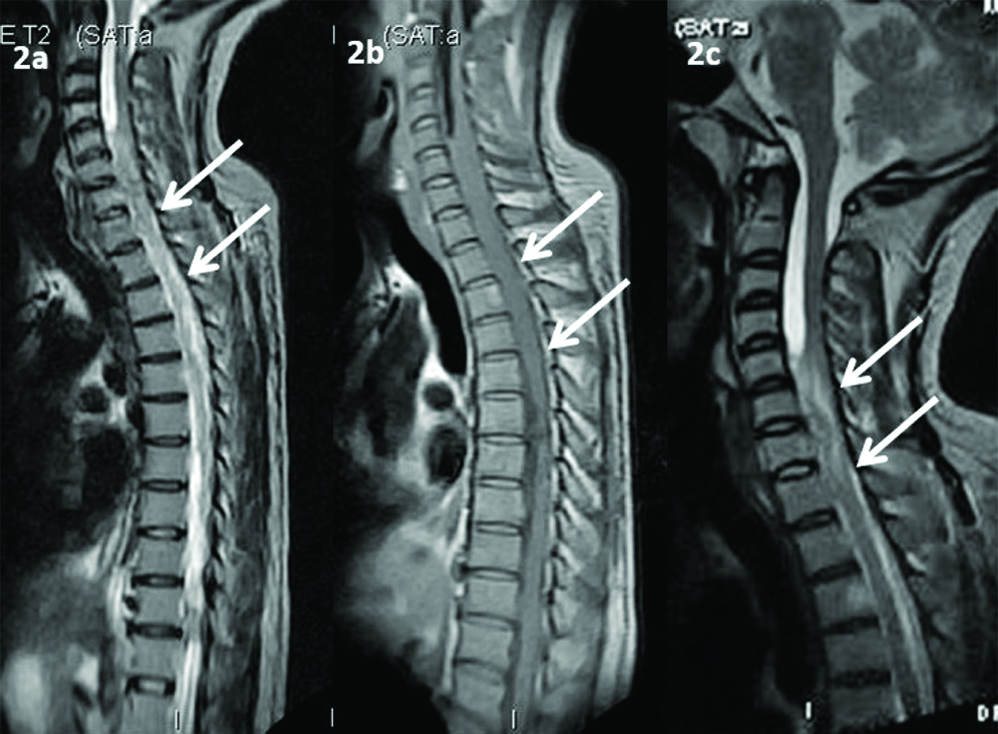
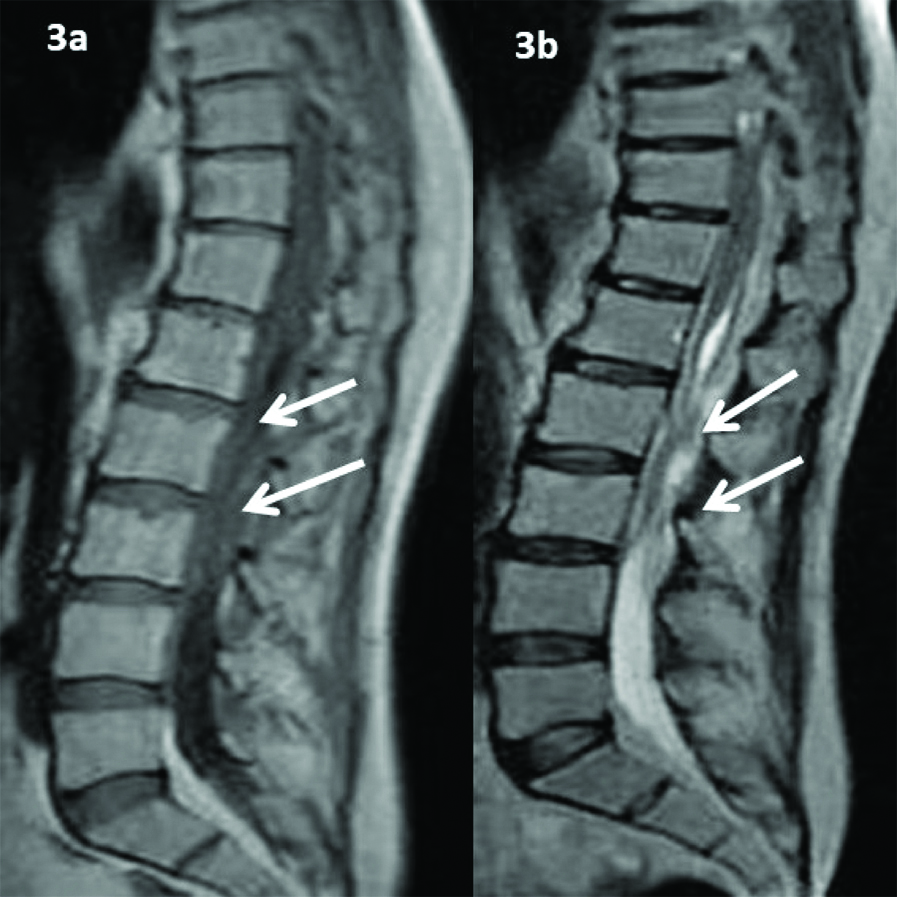
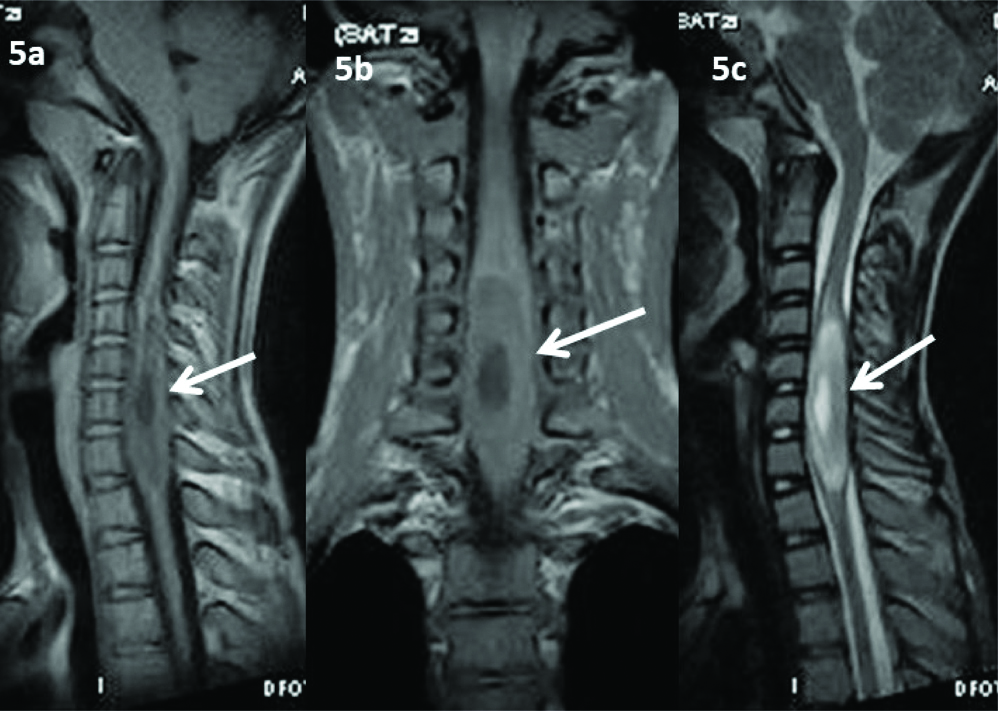
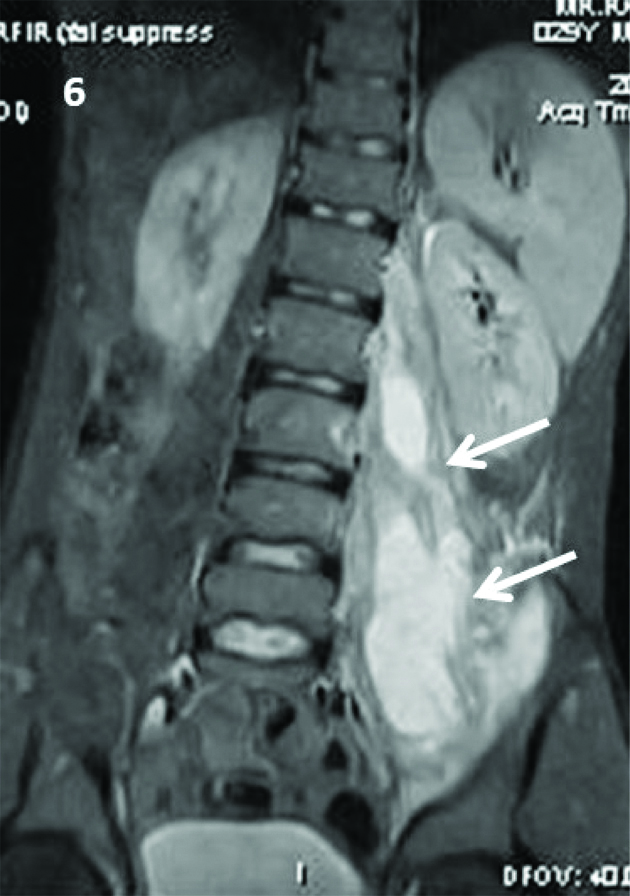
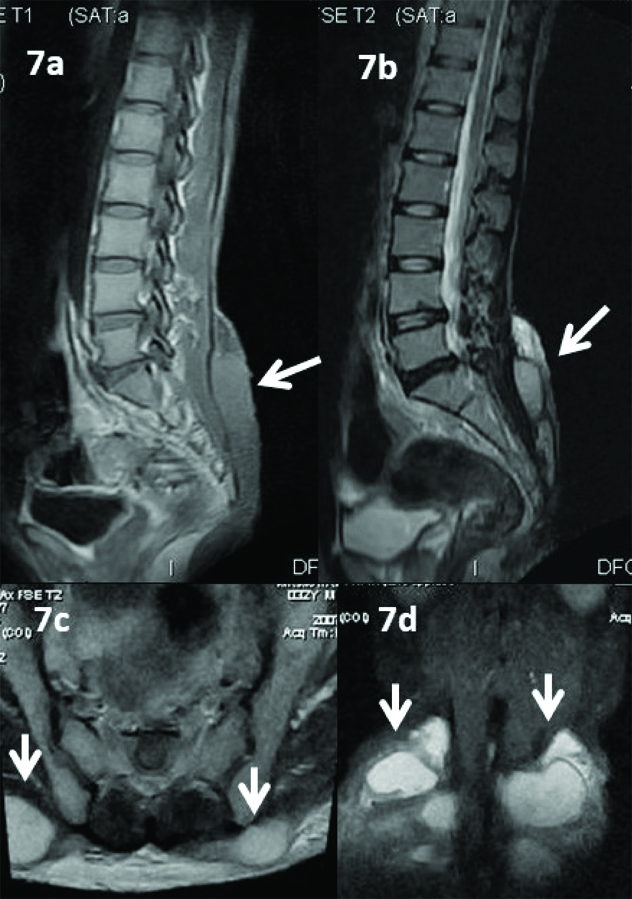
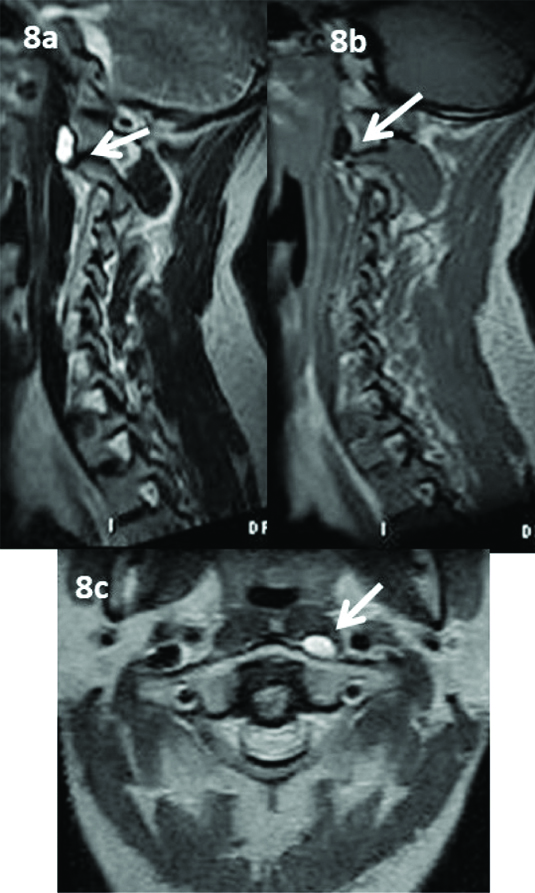
Dorsal region involvement was seen in 21 cases (48.8%) which was the most common in the present study followed by 13 cases and six cases involving Lumbar (30%) and cervical (13.9%) region respectively. Also, three cases were showing multilevel involvement (6.9%). Various extraosseous changes involving spinal and paraspinal components in case of tubercular lesions ranging from intraspinal soft tissue component either in extradural [Table/Fig-1a,b] or Intradural [Table/Fig-2a-c] compartment, Arachnoiditis evidenced by Cerebrospinal Fluid (CSF) signal alteration/clumping of nerve roots [Table/Fig-3a,b], Intramedullary tuberculoma [Table/Fig-4a-c], spinal cord abscess [Table/Fig-5a,b] and the most common Paraspinal soft tissue lesions-Abscesses and Granulation tissue [Table/Fig-6,7a-d,8a-c].
1a. T2W; and 1b. T1W Sagittal images showing long segment extradural soft tissue component (Solid Arrow) in the upper, middle dorsal region of spinal canal compressing the spinal cord leading to cord oedema (Open arrow) at C6 to C7 level.
2a, 2c. T2W; and 2b. T1W Sagittal images showing long segment intradural soft tissue component (Solid Arrow) in the lower cervical and upper dorsal region of spinal canal causing widening of CSF space and compressing the spinal cord.
3a. T1W; and 3b. T2W Sagittal images showing altered CSF signal intensity with clumping of nerve roots and loss of normal cord-CSF interface in the lumbar region with minimal intradural soft tissue component Arachnoiditis.
4a. T1W; 4b. and 4c.T2W Sagittal images showing a well defined T1 isointense and T2 hypointense intramedullary lesion at D1 vertebral body level with severe cord oedema Intramedullary Tuberculoma.

5a. T1W sagittal; 5b. T1W Coronal; and 5c. T2W Sagittal images showing focal cord expansion and central necrotic area in the lower part of cervical spinal cord S/o Spinal Cord Abscess.
T2W Fat suppressed coronal image showing multiloculated hyperintense collection in the left psoas muscle.
7a. T1W; 7b. T2W sagittal images; 7c. T2W axial; and 7d. T2W fat suppressed coronal images showing multiloculated T1 hypointense and T2 hyperintense collection in the both gluteal region.
8a. T2W; 8b. T1W sagittal images; and 8c. T2W axial image of cervical spine showing a small T1 hypointense and T2 hyperintense collection just anterior to atlas on left side.
Paraspinal soft tissue component or abscess is the commonest finding and intramedullary tuberculoma and abscess are the least common findings in the present study [Table/Fig-9]. One patient had both intradural soft tissue component and arachnoiditis.
Pattern of involvement and number of cases.
| S. No. | Pattern of involvement | No. of cases |
|---|
| 1. | Paraspinal soft tissue component | 27 (62.8%) |
| 2. | Intraspinal soft tissue component | 10 (23.2%) |
| 3. | Arachnoiditis | 4 (9.3%) |
| 4. | Intramedullary Tuberculoma | 2 (4.6%) |
| 5. | Spinal Cord Abscess | 1 (2.3%) |
Discussion
In developing countries, skeletal involvement is seen in ~10% of the patients with extrapulmonary tuberculosis in which spine is the most commonly affected [6]. Tuberculous Spondylitis is termed as Pott’s Disease as it was first described by Sir Percival Pott in 1782 [7], caused by Mycobacterium tuberculosis. It usually affects dorsal spine, however, any part of spine may be involved. The usual patterns of vertebral involvement are paradiscal, anterior and central [8]. The affected vertebra and the adjacent disc appear hypointense on T1W and hyperintense on T2W MRI sequences with or without soft tissue component/abscess in the paravertebral and spinal canal regions [3]. Sometimes only soft tissue component can be seen without affecting the bony components of spine. Tuberculosis of spinal region can manifest in various forms in the following order of frequency-Tuberculous Spondylitis (60%), arachnoiditis (20%), meningitis (12%), and intramedullary lesion (8%) [9]. In the present study, soft tissue component is the predominant finding that too in the paraspinal region comprising about 62.8% and only 23.2% of cases showed intraspinal soft tissue component, followed by arachnoiditis (9.3%).
Pathogenesis of Intradural Tuberculous Infection are of three types in the following order of frequency-as a direct extension of disease from the adjacent diseased vertebra, through the CSF from intracranial tubercular meningitis and rarely tuberculous lesion primarily originating in spinal meninges [10-12]. In the present study, all the 43 cases (100%) showed tuberculous lesions arising primarily from the soft tissue in the spinal and paraspinal region but not involving the bony components. Among the 43 cases, 10 cases had intraspinal soft tissue component, four cases had arachnoiditis and three cases had intramedullary lesions such as intramedullary tuberculoma (two cases) and spinal cord abscess (one case), which means these lesions are arising directly from meninges through hematogenous spread which is very rare according to Sree Harsha CK et al., [11]. In 1969 Wadia NH et al., suggested that these forms of Spinal Intradural Tuberculosis such as intradural extramedullary tuberculosis, spinal arachnoiditis, and chronic adhesive arachnoiditis should be designated as “Tuberculous Radiculomyelopathy” [13].
According to Konar SK et al., and Burton CV, Tuberculous radiculomyelopathy has three stages namely Radiculitis - Pia arachnoid inflammation with hyperemia and swelling of nerve roots, Arachnoiditis - adhesion of nerve roots secondary to fibroblast proliferation and collagen deposition and Adhesive Arachnoiditis - Encapsulation of atrophied nerve roots due to dense collagen deposition [12,14].
Usually three types of imaging patterns on MRI for arachnoiditis of Cauda Equina are seen, Central Type - Clumping of Nerve roots in the centre of thecal sac, Peripheral type - Nerve roots will adhere peripherally to dural margins and Mixed Type - Clumping of Nerve roots to one side of thecal sac mimicking soft tissue mass [12,15]. In the present study, all the four cases of arachnoiditis showed mixed type of appearance on MRI [Table/Fig-3a,b].
Patients with tubercular meningitis developing symptoms of spinal cord involvement should raise a suspicion of Tuberculous Radiculomyelitis or Intramedullary Tuberculoma [16]. In the present study none of the patients had Tubercular meningitis.
Intramedullary Tuberculomas are very rare contributing merely 2% of CNS tuberculosis [17]. In the present study, authors got only two cases of intramedullary granulomas out of 43 cases. Tuberculomas are 42 times more common in brain compared to spinal cord and most of which are seen in Dorsal portion [18]. In the present study both the cases of intramedullary tuberculoma were seen in the dorsal portion of spinal cord.
Tuberculomas of the spinal canal can be either intradural or extradural; however, they are uncommon as a cause of spinal cord compression [19-21]. Extradural lesions are usually secondary to Spondylitis. Intradural tuberculomas are either intramedullary or extramedullary in location but are collectively called Spinal cord Tuberculomas [22] among which Intradural extramedullary tuberculous granulomas are the rarest form of spinal tuberculomas [23]. In the present study authors got two cases of Tuberculomas and both were intramedullary in location, Extramedullary tuberculomas were not seen. According to Devi BI et al., the incidence of spinal intramedullary tuberculomas is 1 in 175 cases of spinal Tuberculosis and 1 in 1600 cases of CNS Tuberculosis in India [19].
In 1969, Dastur DK et al., described the pathology of Tuberculosis affecting the spinal cord as follows [24]:
Venous obstruction secondary to meningitis causing oedema of border zones of spinal cord, vasculitis or thrombosis of meningeal vessels causing ischaemic myelomalacia, vascular occlusion causing Infarction or Pericentral necrosis due to Intramedullary Tuberculomas.
MR Appearance of Spinal Intramedullary Tuberculoma [
25,
26]
In this study, the intramedullary tuberculoma appears as a focal lesion which is isointense on T1W image and hypointense on T2W image with severe surrounding T2 hyperintense oedema. Typically on MRI, the intramedullary tuberculomas are hypo or isointense to cord in T1-weighted sequence with only an indirect sign of focal expansion of spinal cord and heterogeneous intensity on T2-weighted image with central hyperintensity and peripheral hypointensity, which is described as target sign. Peripheral enhancement is characteristic feature of tuberculoma on post contrast images [25,26]. The central hyperintensity on T2-weighted image is suggestive of caseating necrosis. The perilesional oedema is usually seen as high signal intensity on T2-weighted image. It may be associated with meningeal enhancement, epidural collections and skip lesions. Pulmonary and other extra pulmonary sites are to be evaluated for primary source of infection. Gadolinium enhanced MRI study helps to demonstrate the classical ring sign of an abscess and can also differentiate myelomalacia from a syrinx [27]. MRI is very helpful in follow-up patients to assess the response to ATT chemotherapy [26].
Isolated intramedullary tuberculomas without primary source from pulmonary or other sites may mimic closely to other intramedullary lesions such as Ependymoma, Glioma or Intramedullary abscess caused by fungal organisms (e.g., blastomycosis, histoplasmosis, candidiasis) [26,28]. In immunocompromised patients, Toxoplasmosis and lymphoma are common differential diagnosis [26]. One case of intramedullary spinal cord abscess seen in the present study which appears as focal expansion of spinal cord with T1/T2 isointense lesion and central T2 hyperintense necrotic area in the cervical cord. The diagnosis of tuberculosis was confirmed by CSF examination. Imaging appearance of intramedullary abscess mimics the intramedullary tuberculoma, however, the cord expansion and area of central necrosis are more in Intramedullary abscess [19].
Involvement of the spinal cord in the absence of skeletal lesions, though uncommon, has been previously reported [10,13,27].
Soft tissue component is the predominant finding in the present study; soft tissue component/abscess was seen in 37 out of 43 cases, among which 27 cases (62.8 %) in paraspinal region and 10 cases (23.2%) in intraspinal compartment. In 2004, a study by Sinan T et al., stated ~65.5% of cases showed paraspinal soft tissue component which almost comparable to the present study [29]. On MRI, soft tissue components are iso-hypointense on T1W images and hyperintense on T2W images, Frank tubercular abscess will be more hyperintense on T2W images with thin hypointense walls with or without septations which will show enhancement in post contrast images [3,4,29].
Limitation
The limitation is the number of cases included in the present study which was very low to assess the epidemiology and also difficult to categorise the typical imaging appearance for various soft involvement in tuberculosis of spinal and paraspinal region.
Conclusion
Tuberculosis should be suspected in patients with inflammatory changes in the soft tissues of spinal and paraspinal region, even when the bony components are not involved. MRI has an excellent capability in detecting the bone and soft tissue involvement in tuberculosis even in the distant asymptomatic site at a very early stage especially the involvement of spinal cord and to assess the integrity of nerve roots.