Cluster Headache in a Case of Ophthalmic Cysticercosis
Animesh Das1, Robin Bansal2
1 Resident, Department of Neurology, Sanjay Gandhi Posgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
2 Resident, Department of Neurology, Sanjay Gandhi Posgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Animesh Das, Resident, Department of Neurology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow-226014, Uttar Pradesh, India.
E-mail: animeshdas05@gmail.com
Cluster headache is considered to be a primary headache. A lot of literature has been published for apparent cluster headache like conditions arising out of organic pathologies like tumours, dissection and infection in the craniofacial area although the causal relationship still needs to be proved convincingly. In certain cases, treatment of the primary pathology like sinusitis or otitis media leads to alleviation of the symptoms of headache. Neuroimaging has been recommended in cases of cluster headache with atypical symptoms and signs or those not responding to treatment. Neuroimaging in the present case of cluster headache was suggestive of ophthalmic cysticercosis. To the best of present authors’ knowledge, cluster headache in ophthalmic cysticercosis has never been described.
Cephalgia, Cranial pain, Imaging, Taenia, Trigeminal cephalgias
Case Report
A 28-year-old male presented to the Outpatient Department (OPD) of Neurology, with recurrent excruciating left sided hemicranial pain for the last six years. Headache was not side shifting. The attacks were associated with congestion and lacrimation of the ipsilateral eye with nasal obstruction and severe restlessness. Each attack persisted for 30-40 minutes with a frequency of 5-6 per day, six days a week. The patient would occasionally get up from his sleep at night time due to severe headache and move around incessantly. The patient used to get these attacks initially at a frequency of 4-6 clusters per year but in the last six months, he complained of about four clusters. These clusters were not seasonal. These attacks used to subside by oxygen inhalation at 10 litres/minute which he had been advised by a neurologist. He had no significant medical or surgical history. On ophthalmologic examination, fundus was normal with no evidence of papilloedema. Visual acuity was 6/6 in both eyes. Intraocular pressure was 18 and 16 mmHg in right and left eye respectively. He had normal field of vision on confrontation test. Extraocular movements were full in all cardinal directions. There were no neurological signs on examination. His systolic blood pressure was in the range of 120-130 mmHg. Tenderness over the sinuses could not be elicited. He was given a provisional diagnosis of cluster headache (ICHD-3) as he fulfilled the revised International classification of headache disorders criteria-3 for cluster headache [1]. Other differential diagnosis kept were ophthalmologic conditions like scleritis, uveitis, sino-orbital disease and intermittent angle closure glaucoma, other primary headaches like paroxysmal hemicrania or hemicrania continua and migraine, vascular causes like arterio-venous malformations, dissections, cerebral venous sinus thrombosis and systemic causes like hypertensive emergencies.
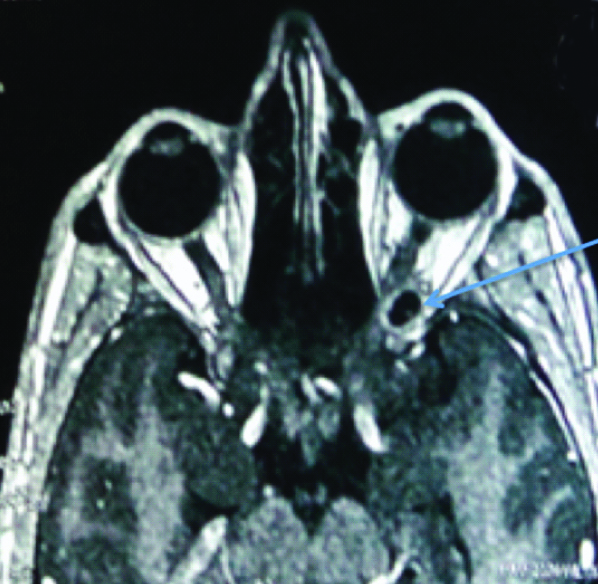
His headache symptoms did not fit into either paroxysmal hemicrania or hemicrania continua because of specific duration associated with these Trigeminal Autonomic Cephalgias (TAC). There was no history of any addiction. ENT evaluation for acute sinusitis was performed which was normal. There was no evidence of any tympanic membrane perforation or any glomus tumour. In view of increasing frequency of cluster attacks in the recent months, a possibility of secondary aetiology of headache was considered and Magnetic Resonance Imaging (MRI) of the brain was planned. MRI orbits with gadolinium contrast was done which revealed a single ring-enhancing lesion at left orbital apex causing shift of left optic nerve to the medial side [Table/Fig-1,2]. The lesion was having T2 hyperintense and T1 hypointense centre. Rest of the surrounding orbital structures were normal with no evidence of any sinusitis. Magnetic Resonance Angiography (MRA) and Venography (MRV) were not suggestive of any aneurysm, dissection or cerebral venous sinus thrombosis. Magnetic resonance spectroscopy of the lesion showed increased lactate (1.33 ppm) and succinate peak (2.4 ppm). This is supportive of a parasitic lesion like cysticercus. All the other MRI findings also favoured a diagnosis of vesicular stage of cysticercosis.
MRI brain with orbital cuts showing T2 hyper intense lesion in left orbital apex causing shift of left optic nerve to the medial side.

T1 contrast enhanced image showing peripheral ring enhancing lesion in left orbit with hypointense centre.
Lesions around the orbit like orbital pseudotumour and sinuses like sinusitis are known to precipitate cluster headache like episodes by stimulating the trigeminovascular pathway [2,3]. The present finding of ophthalmic cysticercosis and typical cluster headache like symptoms may have a cause and effect relationship. Symptomatic cluster headache, secondary to some disorder has been renamed as secondary headache attributed to that disorder in the new classification of ICHD-3 [1]. Ophthalmic cysticercosis and cluster headaches are being treated frequently by steroids in varying doses [4,5]. The acute attacks of the patient during the hospital visit were managed with oxygen inhalation and steroids (methylprednisolone 500 mg for three days) which was a treatment option for both cluster headache and ophthalmic cysticercosis. The headache bouts also settled and he was discharged in stable condition on tapering steroid dose of eight weeks (initial wysolone dose of 40 mg at discharge) with the advice for regular follow-up. At one year follow-up, he had only one attack of cluster headache which was managed symptomatically with oxygen therapy and indomethacin dose of 50 mg thrice a day for one week.
Discussion
Cluster headache is a primary headache syndrome, characterised by recurrent episodes of unilateral pain involving first division of trigeminal nerve along with autonomic symptoms. Although classified as primary headaches, some of the cluster headaches are associated with craniofacial organic aetiologies like hypothalamic and pituitary tumours, meningiomas, carotid artery dissections, vascular malformations which activate the trigeminovascular reflex resulting in trigeminal autonomic cephalgias [6]. These are called secondary cluster headaches [7].
Secondary cluster headaches or symptomatic cluster headaches, although rare, should be suspected in cases of refractory ones, abnormal neurological signs (Horner’s or Adie’s syndrome, trigeminal distribution numbness, ophthalmoplegia, optic atrophy papilloedema, bitemporal hemianopia, swelling of the eye), atypical symptomatology (atypical attack duration and frequency, continuous headache or background headache, headache triggered by sitting and standing, altered consciousness, acute weakness of upper extremity, impotence, acromegaly), age of onset more than 50-year-old and investigations should be planned accordingly [8]. In young individuals, a change in character/frequency of the headache bouts as in the present case, should suggest a secondary cause.
A review of 31 secondary TAC cases published by Favier I et al., suggested that since typical TAC cases fulfilling International Headache Society criteria can also be related to large cerebral mass lesions like pituitary tumours or granulomatous pituitary involvement, neuroimaging (contrast-enhanced MRI with MRA) should always be considered in patients with TAC [8]. Edvardsson B, and Carter DM, have also highlighted the utility of contrast enhanced MRI with MRA in the management of cluster headache [9,10]. In the previously described case series of unusual presentations of Neurocysticercosis (NCC), a wide variety of CNS manifestations like mesencephalic syndrome, tonsilar herniation, haemorrhagic stroke, transient ischaemic attacks and cervical myelopathy has been described [11]. Migraine like or tension type headaches have been described with neurocysticercosis in an epidemiological survey from Ecuader [12]. To the best of authors knowledge, this is the first case in which ophthalmic cysticercosis is causing cluster headache like symptoms.
The pathogenesis of secondary cluster headaches has not been convincingly proven although they have been described in various case series [8,10]. Primary cluster headaches have been related to the activation of trigeminovascular reflex along with hypothalamic activation resulting in various autonomic symptoms of nasal congestion and conjunctival redness and tearing, eyelid oedema, forehead and facial swelling and miosis/ptosis. Pain in secondary causes has been attributed variously to autonomic disturbance caused by structural lesions like hypothalamic and pituitary lesions or irritation of pain sensitive structures and activation of trigeminal nerve endings [12,13]. Since trigeminovascular reflex is involved in the pathogenesis of primary cluster headache, an orbital lesion such as cysticercosis may have irritated the afferent sensory nerves in the ophthalmic division of trigeminal nerve causing reflex activation, manifesting as secondary cluster headache. Since the headache frequency decreased after symptomatic treatment by steroids (intravenous methylprednisolone for three days followed by tapering doses of wysolone 40 mg within a span of eight weeks), authors presume that the lesion may have degenerated in the next one year resulting in near complete resolution of the cluster headache. Unfortunately, authors could not repeat MRI brain with orbital cuts to prove the resolution of the cysticercosis due to financial constraint of the patient but following the clinical profile, authors believe that this cysticercus granuloma was responsible for the attacks of cluster headache. He was free from any cluster attacks even at follow-up visits of 18 months and 22 months. The character of cluster headache in the present case was not different from those of typical attacks of primary cluster headache.
Conclusion
Ophthalmic cysticercosis may present with cluster of headache like symptoms. In cases of cluster headache associated with atypical signs and symptoms or recent change in character, contrast-enhanced MRI with MRA should be done to find out secondary causes ranging from benign cysticercus granuloma to malignant pituitary tumours, neurovascular malformations and dissections.
[1]. Headache Classification Committee of the International Headache SocietyThe International Classification of Headache Disorders 2018 383rd edition(1)Cephalalgia:1-211.10.1177/0333102417738202 [Google Scholar] [CrossRef]
[2]. Takeshima T, Nishikawa S, Takahashi K, Cluster headache like symptoms due to sinusitis: evidence for neuronal pathogenesis of cluster headache syndromeHeadache 1988 28:207-08.10.1111/j.1526-4610.1988.hed2803207.x3384646 [Google Scholar] [CrossRef] [PubMed]
[3]. Harley JS, Ahmed F, Cluster-like headache heralding inflammatory orbital pseudotumourCephalalgia 2008 28:401-02.10.1111/j.1468-2982.2007.01521.x18241221 [Google Scholar] [CrossRef] [PubMed]
[4]. Sekhar GC, Lemke BN, Orbital cysticercosisOphthalmology 1997 104(10):1599-604.10.1016/S0161-6420(97)30090-6 [Google Scholar] [CrossRef]
[5]. Shapiro RE, Corticosteroid treatment in cluster headache: evidence, rationale, and practiceCurr Pain Headache Rep 2005 9(2):126-31.10.1007/s11916-005-0050-315745623 [Google Scholar] [CrossRef] [PubMed]
[6]. Alexander DN, Peter JG, Cluster headache Clinical ReviewBMJ 2012 344:e240710.1136/bmj.e240722496300 [Google Scholar] [CrossRef] [PubMed]
[7]. Cremer PD, Halmagyi GM, Goadsby PJ, Secondary cluster headache responsive to sumatriptanJ Neurol Neurosurg Psychiatry 1995 59(6):633-34.10.1136/jnnp.59.6.6337500105 [Google Scholar] [CrossRef] [PubMed]
[8]. Favier I, van Vliet JA, Roon KI, Witteveen RJ, Verschuuren JJ, Ferrari MD, Trigeminal autonomic cephalgias due to structural lesions: a review of 31 casesArch Neurol 2007 64(1):25-31.10.1001/archneur.64.1.2517210806 [Google Scholar] [CrossRef] [PubMed]
[9]. Edvardsson B, Symptomatic cluster headache: A review of 63 casesSpringerplus 2014 3:6410.1186/2193-1801-3-6424570848 [Google Scholar] [CrossRef] [PubMed]
[10]. Carter DM, Cluster headache mimicsCurr Pain Headache Rep 2004 8(2):133-39.10.1007/s11916-004-0027-714980148 [Google Scholar] [CrossRef] [PubMed]
[11]. Wilbrink LA, Ferrari MD, Kruit MC, Haan J, Neuroimaging in trigeminal autonomic cephalgias: when, how, and of what?Curr Opin Neurol 2009 22:247-53.10.1097/WCO.0b013e32832b4bb319434790 [Google Scholar] [CrossRef] [PubMed]
[12]. Cruz ME1, Cruz I, Preux PM, Schantz P, Dumas M, Headache and cysticercosis in Ecuador, South AmericaHeadache 1995 35(2):93-97.10.1111/j.1526-4610.1995.hed3502093.x [Google Scholar] [CrossRef]
[13]. Leone M, Bussone G, Pathophysiology of trigeminal autonomic cephalalgiasLancet Neurol 2009 8:755-64.10.1016/S1474-4422(09)70133-4 [Google Scholar] [CrossRef]