FB aspiration is a common paediatric emergency especially in children under three years of age. If not diagnosed adequately and managed timely, serious complications can result from it. Rigid Bronchoscopy (RB) is the gold standard for diagnosis and treatment; however it is an invasive procedure and has its own share of complications. It is thus desired that a non-invasive modality should first be used for diagnosis before bronchoscopy, to avoid unnecessary intervention and anesthesia [1-3].
Whereas, a chest radiograph is generally the first imaging modality to be used in diagnosis, it is helpful only in radio-opaque foreign bodies. Since most aspirated foreign bodies are radiolucent, there may be negative chest radiographs in about 1/3rd children who aspirate FBs. Here diagnosis depends on indirect signs such as emphysema, atelectasis, and pneumonic infiltration which are not always present [4].
With the advent of newer radiological modalities such as Multi Detector CT (MDCT), paediatric thoracic and specifically airway imaging has significantly improved. Reduction in scanning time, ability to image large anatomical areas together and contrast enhancement have made MDCT a desired modality for airway imaging. Also, associated pulmonary signs secondary to airway obstruction such as atelectasis and emphysema are better assessed by the wholesome thoracic imaging done by MDCT. In case of an alternate diagnosis, it can help prevent an unnecessary bronchoscopy and guide further therapeutic measures [5].
This study aims at assessing the efficacy of MDCT in detecting removable airway obstruction in paediatric patients with acute onset respiratory distress due to clinical suspicion of FB aspiration; thus guiding for or against an invasive maneuver such as bronchoscopy. Also, it is aimed to study the accuracy of MDCT in detecting the cause of airway obstruction.
Materials and Methods
Study Design
After due clearance from Institutional Ethics Committee via Letter no IEC/HMPCMCE-/2018/Ex.25/150/18 (Dated:6.8.18); a retrospective observational study was done at Department of Radio-Diagnosis of Pramukh Swami Medical College, Anand, Gujarat, India, which is a tertiary teaching hospital in rural western India. The data analysed was from the MDCT studies done between June 2016 to May 2018.
Inclusion Criteria
The data of all patients less than 18 years of age, who presented with sudden onset respiratory distress due to clinical suspicion of FB aspiration; undergoing MDCT Thorax followed by further management (Rigid Bronchoscopic evaluation or other non-invasive management) at the institute.
Exclusion Criteria
Paediatric patients with respiratory symptoms and no suspicion of FB aspiration.
Patients not undergoing post MDCT management: Bronchoscopy or otherwise at the Institute i.e., Patients lost to follow-up.
Source of Data
Axial Source Images and Reconstructed Minimum Intensity Projection images, Multi Planar Reformation images, Volume Rendering and Virtual bronchoscopy images were obtained from the Hospital Picture Archiving and Communication System (Mediff Version 3.5.7) for the study period. Corresponding clinical and Bronchoscopic details were obtained from the Hospital Records.
Investigator
A single Radiologist, blinded to the bronchoscopic findings, retrospectively analysed the MDCT data of the patients included in the study and thereafter compared them with the available bronchoscopic results from the hospital database. The results were documented in the Performa format depicted in [Table/Fig-1].
Performa for documentation of variables used in the study.
| S. No | Variable | Observation |
|---|
| 1. | Age (In Months): | |
| 2. | Gender (M/F): | |
| 3. | Duration of onset of respiratory distress: | |
| 4. | MDCT findings: | |
| a) Presence or absence of airway obstruction: | |
| b) Cause of airway obstruction: FB/Mucus Plug/Other | |
| c) Site of airway obstruction: | |
| d) Other pulmonary findings : | |
| e) Type of foreign body: Radio-opaque/Radio-lucent | |
| 5. | Alternate diagnosis: | |
| 6. | Bronchoscopy indicated or not by MDCT (Y/N): | |
| 7. | Bronchoscopic findings: | |
| 8. | Alternate treatment: | |
Imaging Protocol
All patients included in the study underwent a Plain CT Thorax/Contrast enhanced CT scan of Thorax on a 128 Slice Optima CT 660 (Wipro GE Healthcare Pvt., Ltd.,). The prerequisites before a CT scan included a normal renal function test (S. creatinine and creatinine clearance), and a written informed consent from the patient’s guardians, for an intravenous contrast study. Non-contrast 5 mm thick contiguous helical MDCT sections of thorax were performed from the lung apices to mid portion of kidneys. Wherever, indicated, 1.5 mL/kg of non-ionic iodinated contrast medium was injected intravenously and scans were taken in similar protocol thereafter. Few 5 mm coronal reconstructions, 5 mm thick sagittal reconstructions were also done through the region of interest. The three-dimensional reconstructed and Multi Planar Reformatted (MPR) images were obtained. Volume Rendering and Virtual bronchoscopic reconstruction was done wherever required.
The axial images were first analysed in mediastinum, lung and bone windows. This was followed by isotropic reconstruction and analysis of sagittal and coronal images. Other reconstructive algorithms were analysed thereafter.
Statistical Analysis
Efficacy of MDCT in determining presence and cause of airway obstruction thereby advising for or against a further bronchoscopy was analysed on the lines of Sensitivity, Specificity and Accuracy. All calculations were done in Microsoft Excel and MedCalc Software version 18.9.
Results
We included a total of 19 patients in our study, all of which underwent MDCT Thorax. A majority of 13 (68.4%) of these 19 patients underwent a RB after MDCT.
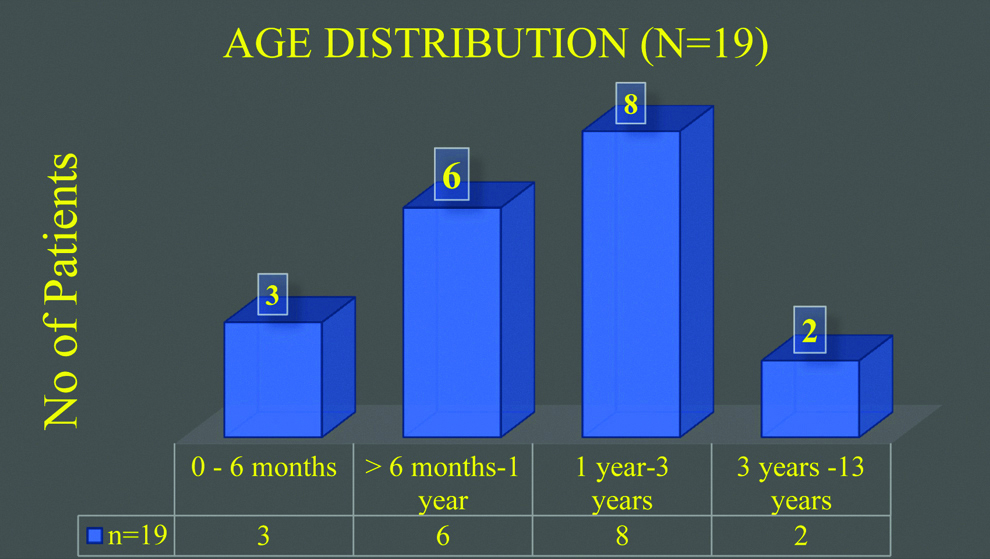
Our study group included patients from 6 months to 13 years of age with mean age of presentation being 4.3 years. The most common age group was Toddlers (1-3 years) (n=8; 42.1%) [Table/Fig-2]. Fourteen (74%) out of 19 children were males thereby forming 3/4th of the total study population.
Age profile of study population.
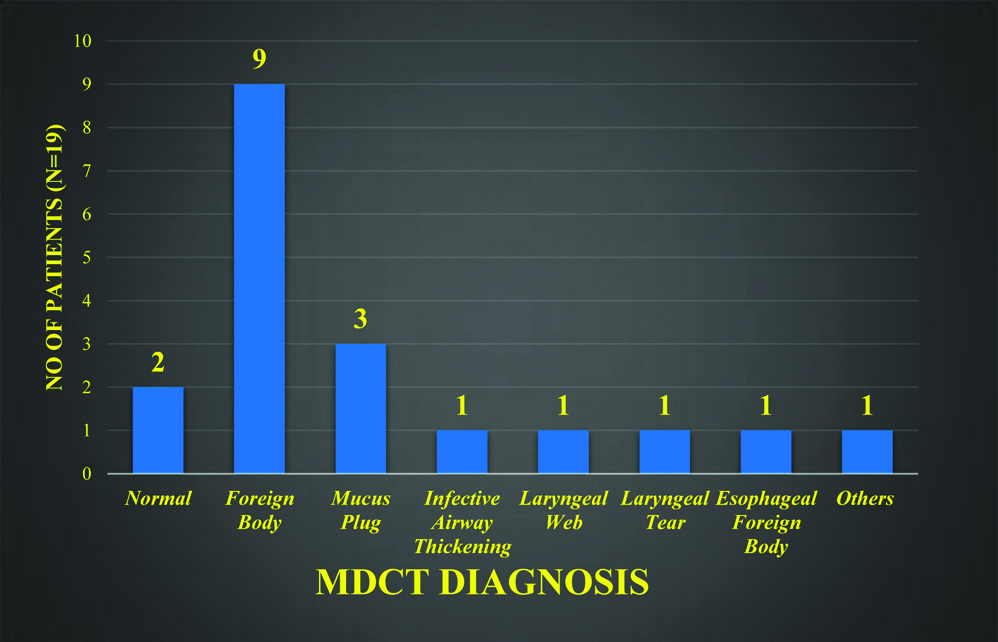
The first and foremost interpretation from MDCT scans was the presence or absence of a removable airway obstruction. The primary MDCT diagnosis of airway FB was made in nine cases and airway mucus plugs were seen in three cases. Overall primary MDCT diagnosis in study group is depicted in [Table/Fig-3]. This observation implied that according to MDCT, 12 (63%) out of 19 cases of suspicious FB aspiration had a removable airway obstruction and hence further management by RB was advised in these cases. Whereas, more than 1/3rd of the study group i.e., the rest seven (37%) cases had an alternate diagnosis and were not advised by the radiologist to undergo bronchoscopic intervention.
Primary MDCT diagnosis in all study subjects.
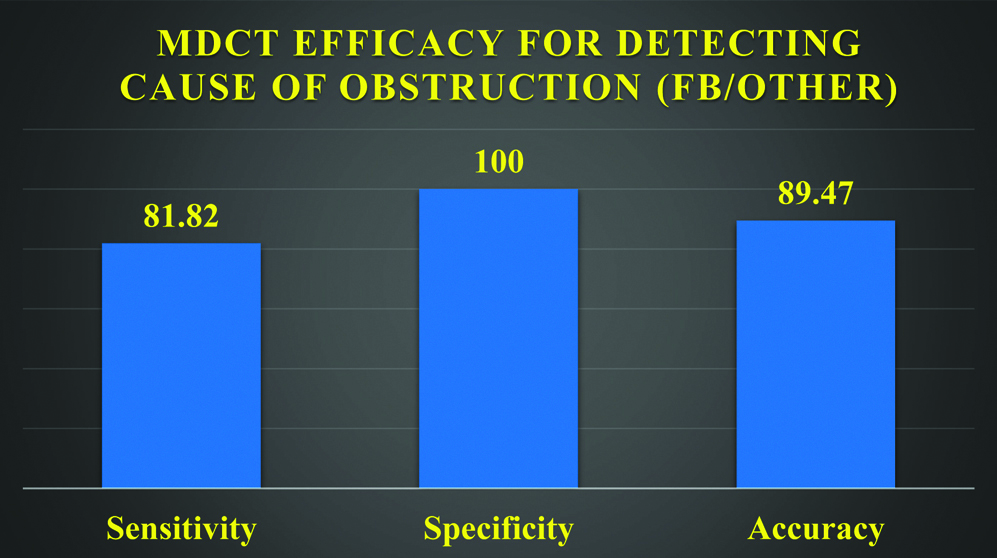
In all these 12 cases, bronchoscopy was done as advised by radiological input. In 10 out of these 12 cases, an airway FB was found and successfully extracted. In the rest two cases, mucus plugs were found occluding the airway. Hence, MDCT had misdiagnosed one case of FB as a mucus plug. In addition to this pertaining to very strong clinical suspicion, RB was done in one more case despite of a normal MDCT. In this case a thorn (organic/plant matter) was found in the airway which was missed on MDCT. Therefore, MDCT showed two false negatives for diagnosing airway FB in comparison to bronchoscopy. The accuracy of MDCT in diagnosing “cause” of airway obstruction is plotted in [Table/Fig-4].
Statistical analysis of MDCT performance for detecting cause of airway obstruction.
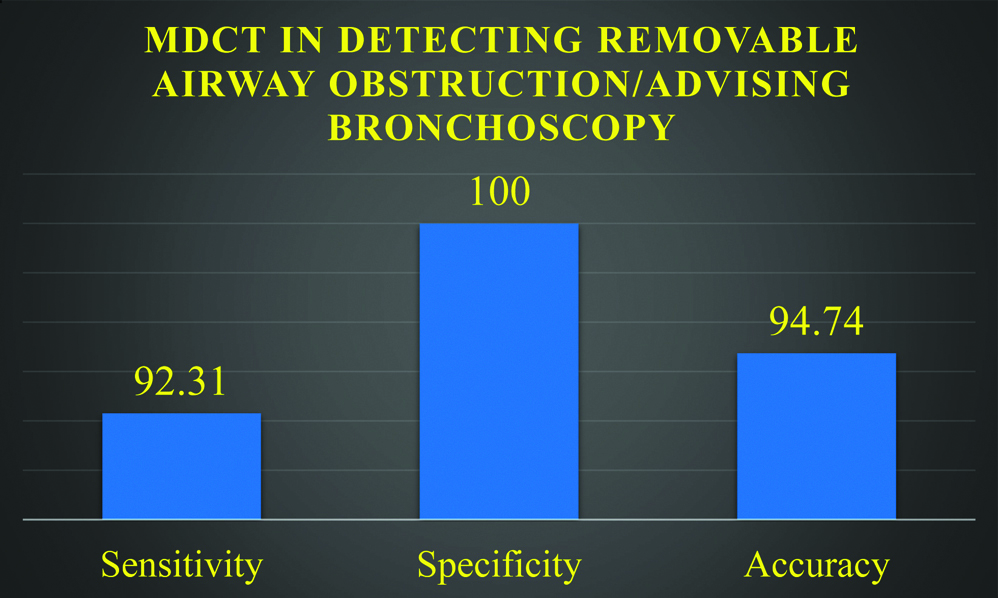
The major purpose of our study however, was answered in this further analysis that MDCT had suggested diagnosis other than intraluminal airway obstruction in seven cases thereby advising against bronchoscopy. This was found to be correct in six cases; thus preventing an unnecessary Intervention correctly in 1/3rd of the study group with an accuracy of 85.71% [Table/Fig-5].
Statistical analysis for MDCT performance in detecting removable airway obstruction.
The most prevalent type of FB were non-metallic (n=8) with ground nut seeds (n=4) forming the major bulk of inhaled FBs.
Other MDCT analysis included the site of airway obstruction, in which right main bronchus was found to be the most common site (n=5) followed by left main bronchus (n=3). Other sites included trachea and distal bronchi, in two cases each. Amongst the secondary pulmonary findings, Collapse-Consolidation (n=9) was seen most commonly followed by Hyper-aeration (n=2). Pneumothorax was seen in one case. No secondary findings were seen in rest of the cases.
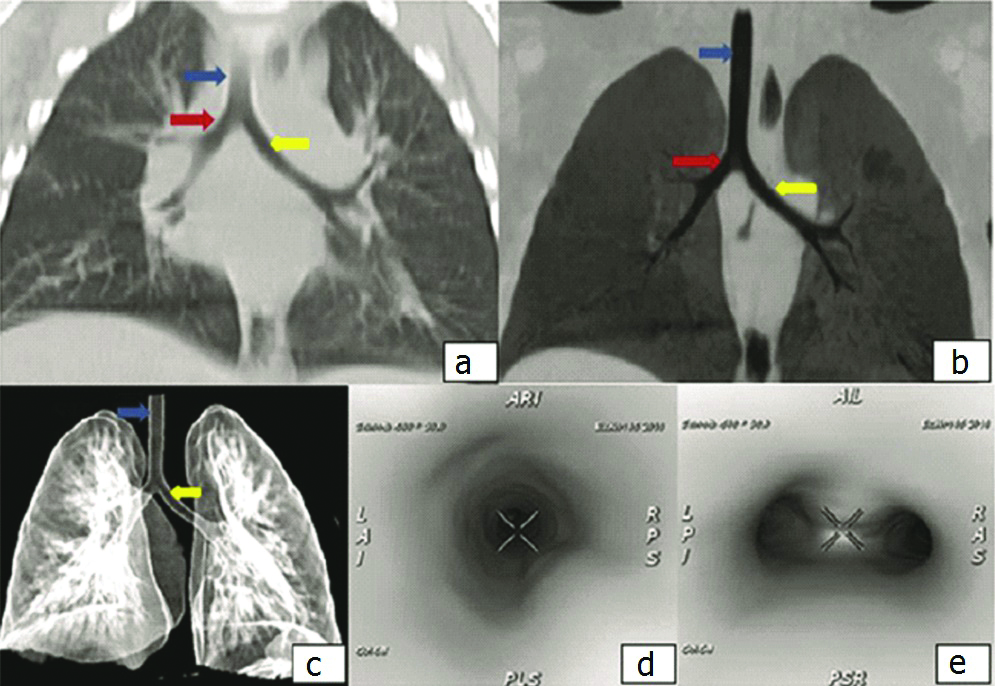
Various MDCT representations of a normal Paediatric airway anatomy are depicted in [Table/Fig-6].
Normal paediatric airway on MDCT: a) Coronal reconstruction of lung window; b) MinIP coronal image; c) Volume rendering image (Blue Arrow: Trachea, Red Arrow: Right Main Bronchus, Yellow Arrow: Left Main Bronchus); d) Virtual Bronchoscopy (VB) image showing trachea; e) VB at level of carina showing right and left main bronchi.
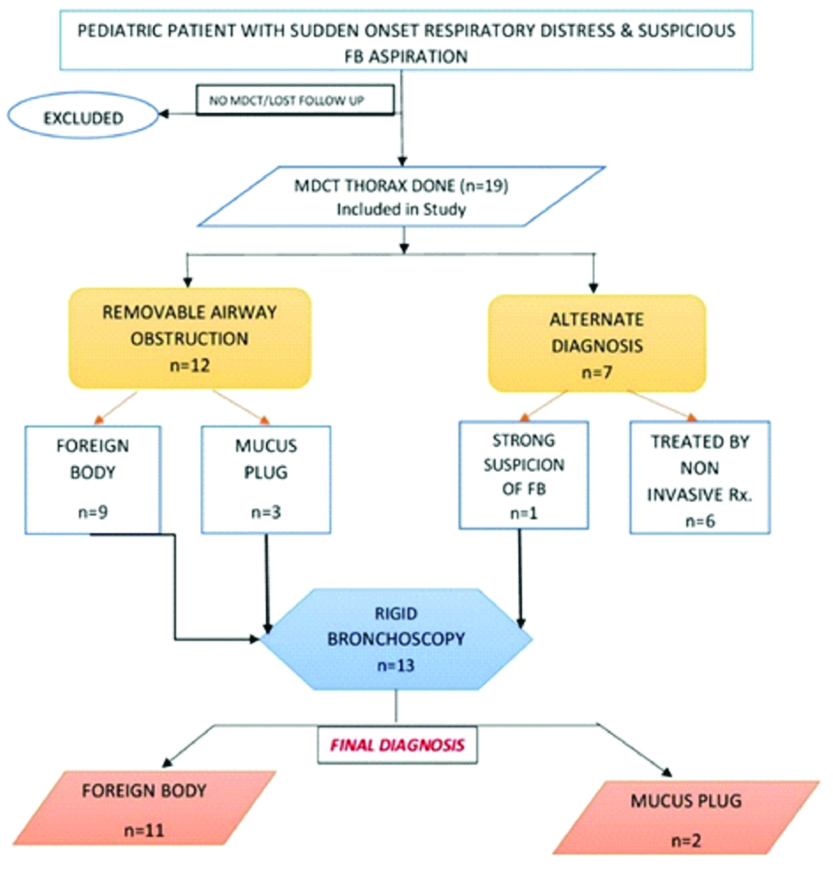
The Study Design and Observations are summed up in the flowchart in [Table/Fig-7]. Few representational cases are shown in [Table/Fig-8,9 and 10].
Flowchart depicting the study design and major observations from the study.
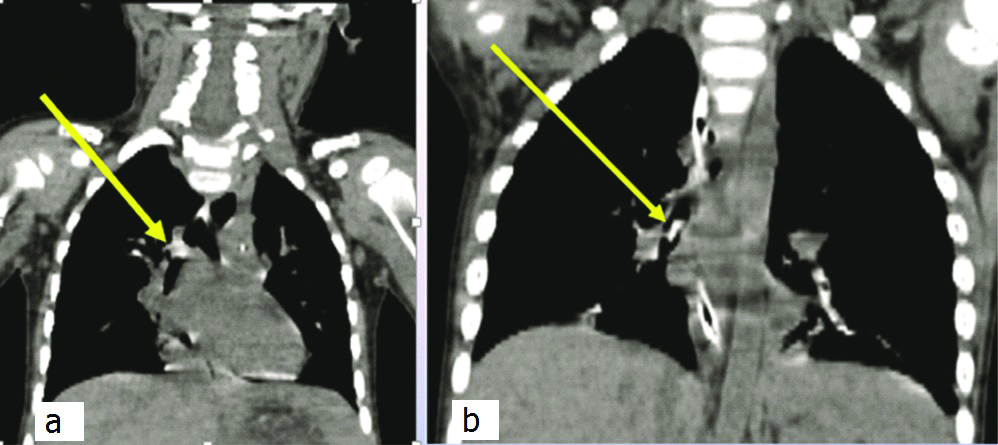
In two separate patients represented in Coronal MDCT images (a) and (b), hyperdense metallic Foreign Bodies (Yellow Arrows) are seen lodged in the Right Main Bronchus.
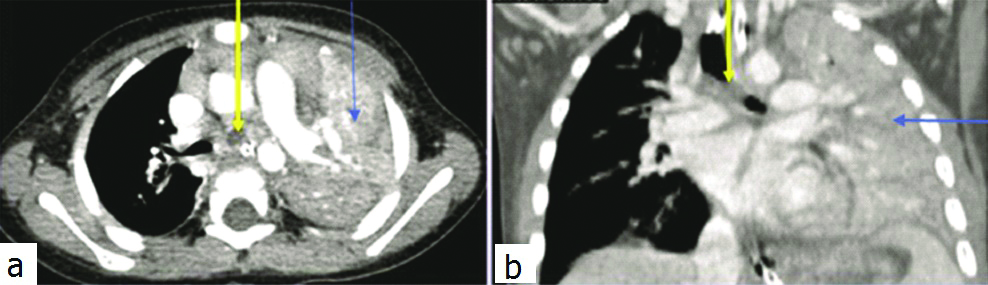
A hypodense non-metallic Foreign Body (Yellow Arrow) is seen obstructing the Left Main Bronchus in Axial (a) and Coronal (b) MDCT images. Associated massive consolidation is observed in the left lung (Blue Arrow).
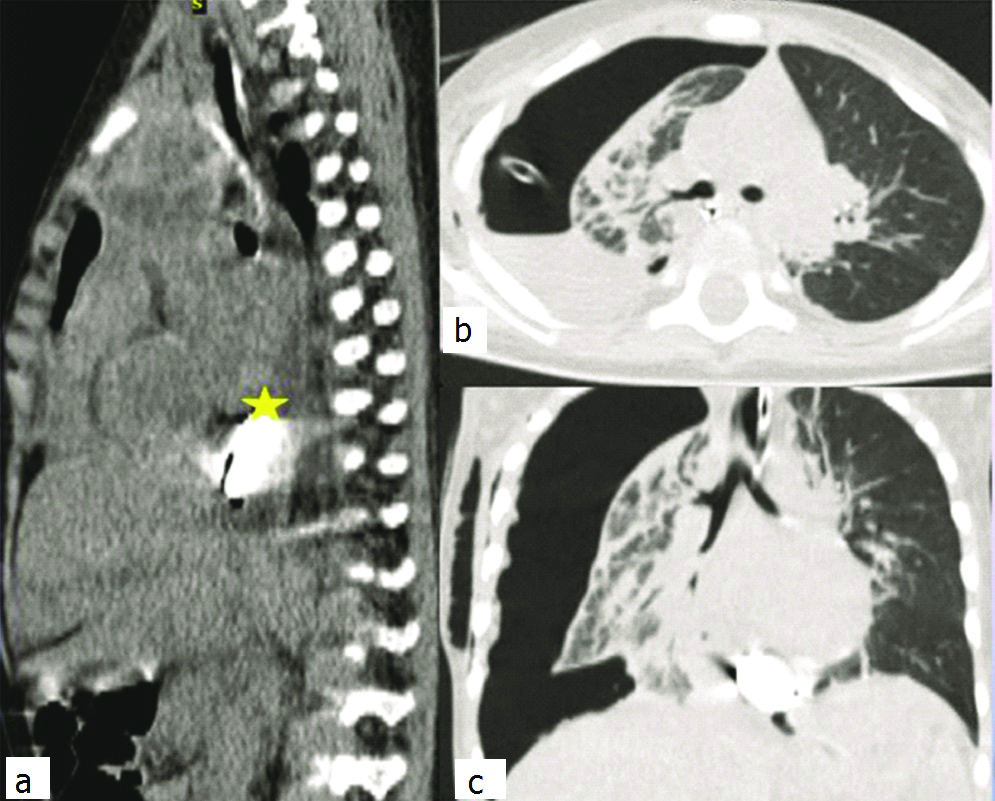
In Sagittal Plain MDCT image (a), a metallic object (yellow asterix) is seen lodged in the posterior mediastinum (oesophagus). In axial lung window images (b), pneumothorax with fluid collection is seen in right hemithorax. In Coronal lung window images (c), along with pneumothorax and Foreign Body as described earlier, it is seen that the central airways are clear.
Discussion
In a paediatric emergency, when a clinician has a suspicion of airway FB aspiration, it is prudent to take quick decisions resulting in a correct and comprehensive diagnosis, thereby leading to early management to prevent possible complications. This study is aimed to guide the clinician to choose the fastest, most accurate and least invasive way to confirm this diagnosis.
RB is the gold standard for both diagnosis and removal of airway obstructing agent; however, it has been described in literature to have a complication rate of 4-17% which includes life threatening complications such as respiratory distress, pneumothorax, cardiac arrest, pneumonia, tracheal laceration and pneumo-mediastinum even in experienced hands. Thus, a need for a non-interventional diagnostic modality to confirm the presence of FB and rule out alternate diagnoses mimicking FB arises [3,6].
Where plain radiography is not very satisfactory with a low sensitivity of 60-67% and specificity of 32-68% for detecting airway FB in children [6-8]; the next plausible alternative to Bronchoscopy is CT. After the advent of MDCT, a quick, wholesome approach is provided to image the central airways. A single-breath-hold acquisition by CT is suffice for imaging the whole tracheobronchial tree. Normal anatomical structures and associated pathological conditions can both be precisely imaged in various planes and reconstructions. MDCT is capable of diagnosing both radio-opaque and radio-lucent FB unlike plain radiography [1,5,9].
FB aspiration is most commonly observed in literature in young children of less than three years of age with a male predominance. This is attributed to the newly found chewing abilities of these children which make them put foreign objects in their mouth and the lack of molars to properly chew on items [10]. We also found male toddlers as the most common population of our study group with a mean age of 4.3 years similar to the findings of Kosucu P et al., and Boufersaoui A et al., [6,11].
Non-metallic FB were the most common group of objects to be aspirated by children in our study with a 66% prevalence as also observed by Boufersaoui A et al., [11]. Ground nut seeds were the most common objects to be aspirated similar to the findings of Abd-El Gawad EA et al., and Saki N et al., [1,12]. Organic FB are known for delayed diagnosis owing to their radiolucent appearance. While the diagnostic time is prolonged, they tend to swell in the airway and cause bronchial obstruction and stenosis, hence re-emphasising the need for a quick diagnostic modality [13].
We found Right main bronchus to be the most common site for lodging of FB in 71.4 % of cases similar to the observations of Haliloglu M et al., and Saki N et al., [12,14]. This observation may be attributed to the larger size and more vertical orientation of the right main bronchus in comparison to the left [10].
Direct visualisation of the FB in a central airway is the most accurate diagnostic cue. In nine out of 11 cases of positive FB, proven on Bronchoscopy, MDCT could localise the FB by direct visualisation in the airway. In the two false negatives, a FB was misread as a mucus plug and in another case a thorn was missed on MDCT. Both these false interpretations were also observed by Bhat KV et al., while analysing MDCT on similar parameters for FB aspiration [6,9].
The emphasis on a radiological examination prior to bronchoscopy is not only for the establishment of clinical cues, it is also extremely pivotal to rule out alternate diagnosis and prevent unnecessary exposure to the complications of bronchoscopy and anesthesia. The major defining factor for this study is the variety and the number of alternate diagnoses that we observed on MDCT which prevented unnecessary intervention and guided further therapeutic approach. A glaring example of this would be a case where the parents saw their toddler take a metallic battery in his mouth followed by onset of respiratory distress after a few hours. Though clinically, the diagnosis was certain, MDCT concluded that the said FB was in the Child’s esophagus, which was ruptured causing a pneumothorax and pleural collection hence resulting in the respiratory symptoms. The airway was clean and an endoscopy was thus planned in place of a bronchoscopy for this patient [Table/Fig-10].
Comparative table for Statistical Analysis of MDCT performance in detecting Airway FB in children [1,9,15,16].
| Statistical Parameters | ElGawad EA et al., [1] (n=21) | Bhat KV et al., [9] (n=40) | Manach Y et al., [15] (n=303) | Hong SJ et al., [16] (n=51) | Present Study (n=19) |
|---|
| Sensitivity | 94.4% | 92.3% | 98% | 100% | 92.3% |
| Specificity | 75% | 85.7% | 97% | 66.7% | 100% |
| Accuracy | 90.4% | 90% | - | 94.1% | 94.7% |
In this study, where the aim was to help the clinician arrive at a diagnosis with least hassle, MDCT was correct in advising for bronchoscopy 12 out of 12 times (100%) and against further intervention six out of seven times (85%); therefore preventing six patients i.e. 31% of the study population from unnecessary intervention. Hence, the excellent primary diagnostic potential of MDCT in airway imaging with a high sensitivity of 92.3% and an overall accuracy of 94.7% for detecting removable airway obstruction was re-established; which was comparable to many recent studies in literature [Table/Fig-11] [1,9,15,16].
Radiation exposure remains the concern for making MDCT an essential diagnostic modality in paediatric airway obstruction. Recent studies have been focused to resolve this issue by attempting to reduce the radiation dose by various methods. The most common method implemented to decrease radiation dosage has been decrease in tube current, which is linearly related to dosage at a fixed kilo voltage and scanning time. Choi YW et al., defined the optimum tube current as the minimum milliamperage (mA) necessary to image a diagnostic quality image [17]. A CT done at 30 mA in paediatric chest causes significant reduction in radiation dose which is about 0.2 mSv at this tube current [18]. Kosucu P et al., used this principle to observe that a low tube current of 25 to 50 mA was found sufficient to detect airway FB in children with a radiation dose reduction of about two-third as compared to conventional CT [6]. It is thus hoped that low dose MDCT will pave a way for regularisation of CT in the protocol for diagnosis of paediatric airway FB.
Limitation
A small sample size and retrospective nature of our study are its major limitations. The authors agree that this study can form the basis of a larger prospective study over a longer duration, which shall bring more significant statistical results in the said situation. In a prospective study, a low radiation protocol may be optimally induced in the study.
Conclusion
The establishment of a quick diagnosis and the essentiality of ruling out alternate diagnosis which are common despite high clinical suspicion of FB aspiration in children, are both accurately and comprehensively addressed by MDCT. The major contribution of our study is in realising the excellent capability of MDCT in correctly preventing unnecessary interventions (85%), thereby enforcing the essentiality of MDCT Thorax to precede Bronchoscopy.