Situs Inversus Totalis with Chronic Respiratory Ailment in a Fertile Male
Muneeb Mohammed1, A Sundaramurthy2, KP Ajeesh3, Jereen Varghese4, Venketesh Rathinavel5
1 Postgraduate, Department of Pulmonary Medicine, Shri Sathya Sai Medical College and Research Institue, Chennai, Tamil Nadu, India.
2 Professor and Head, Department of Pulmonary Medicine, Shri Sathya Sai Medical College and Research Institue, Chennai, Tamil Nadu, India.
3 Assistant Professor, Department of Pulmonary Medicine, Shri Sathya Sai Medical College and Research Institue, Chennai, Tamil Nadu, India.
4 Assistant Professor, Department of Pulmonary Medicine, Shri Sathya Sai Medical College and Research Institue, Chennai, Tamil Nadu, India.
5 Postgraduate, Department of Pulmonary Medicine, Shri Sathya Sai Medical College and Research Institue, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. A Sundaramurthy, 7(4) 9th Cross Street, Shasthri Nagar Adyar, Chennai, Tamil Nadu, India.
E-mail: sundaramurthy33@gmail.com
Primary Ciliary Dyskinesia (PCD) is a rare ciliopathic autosomal recessive genetic disorder that causes defect in the action of cilia lining the respiratory tract. In a total of 50% cases of situs inversus totalis fertility is preserved. Here, we report a case of situs inversus totalis with chronic respiratory ailment in a fertile male. A 60-year-old non smoker male, father of four children presented with recurrent episode of infection for past five years. Investigation was done which showed situs inversus totalis (Dextrocardia) with right lower lobe bronchiectasis. He was managed with antibiotics, mucolytics, bronchodilators and chest physiotherapy. Patient status improved well with above mentioned treatment.
Bronchiectasis, Dextrocardia, Primary ciliary dyskinesia
Case Report
A 60-year-old, non smoker male presented with complaints of cough with expectoration and with history of recurrent episode of infections for past five years which were treated symptomatically. Patient had no history of haemoptysis, chronic constitutional symptoms or taking anti-tubercular treatment. He was born out of non-consanguineous marriage, had four children, and is farmer by occupation.
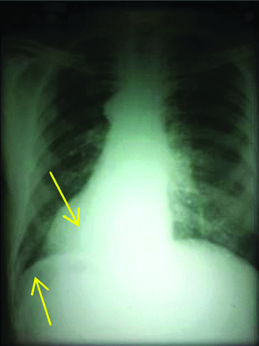
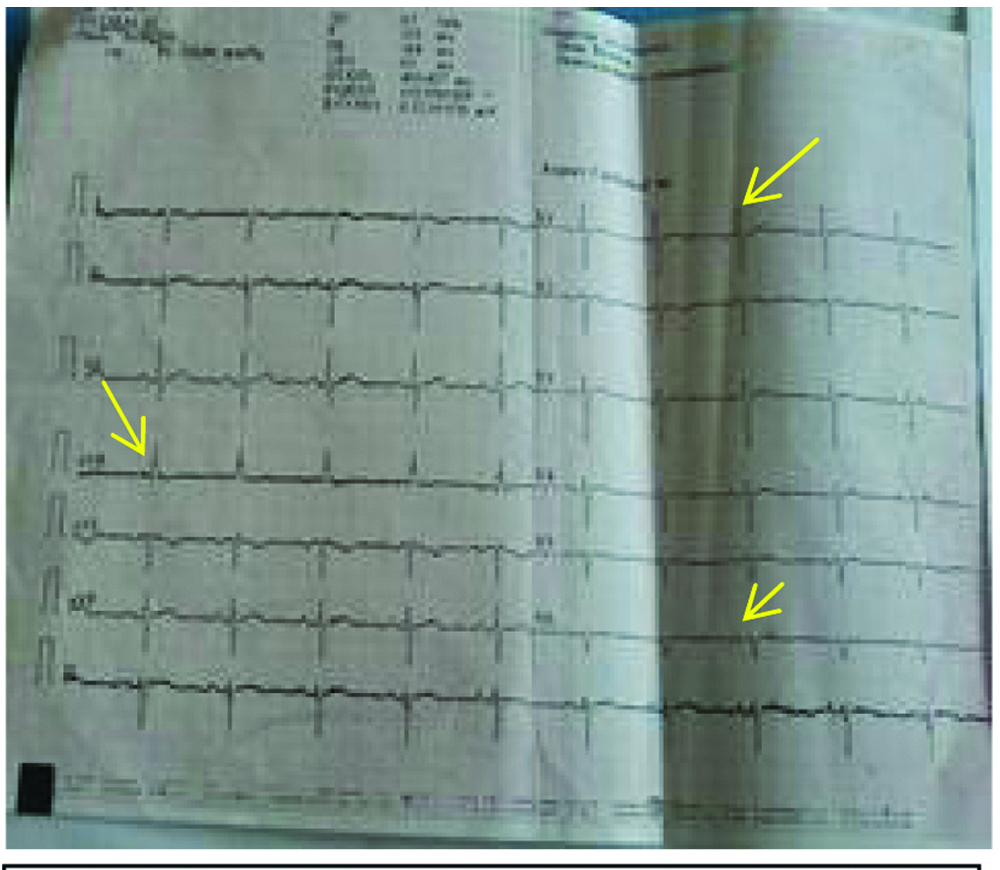
On examination, he had grade II clubbing, vitals were stable, traube’s space was obliterated on left side, liver dullness absent on right side. On auscultation coarse crepitations were heard on right lower hemithorax and heart sounds were best heard on right side of the chest. Blood count was normal and sputum for acid fast bacilli was negative. His chest X-ray [Table/Fig-1] showed dextrocardia and fundus gas was noted on right side. Further, CT scan [Table/Fig-2a,b] was taken which showed dextrocardia, arch of aorta on left, liver on left side with cystic changes appreciated on right lower lobe. X-ray PNS revealed hypoplastic frontal sinus bilaterally [Table/Fig-3]. ECG was taken dextrocardiac features were noted [Table/Fig-4]. For further evaluation USG abdomen and bronchoscopy was done which showed situs inversus totalis with simple renal cyst and inversion of bronchial pattern with mucopurulent secretion noted on right lower lobe respectively. For assessing ciliary function saccharin test was done, test prolonged for one hour twenty minutes. Final diagnosis was primary ciliary dyskinesia, hypoplastic frontal sinus, right lower lobe bronchiectasis, situs inversus totalis (no structural defect).
Dextrocardia, fundus gas was noted on right side (arrow).
CT dextrocardia, arch of aorta on left, liver on left.
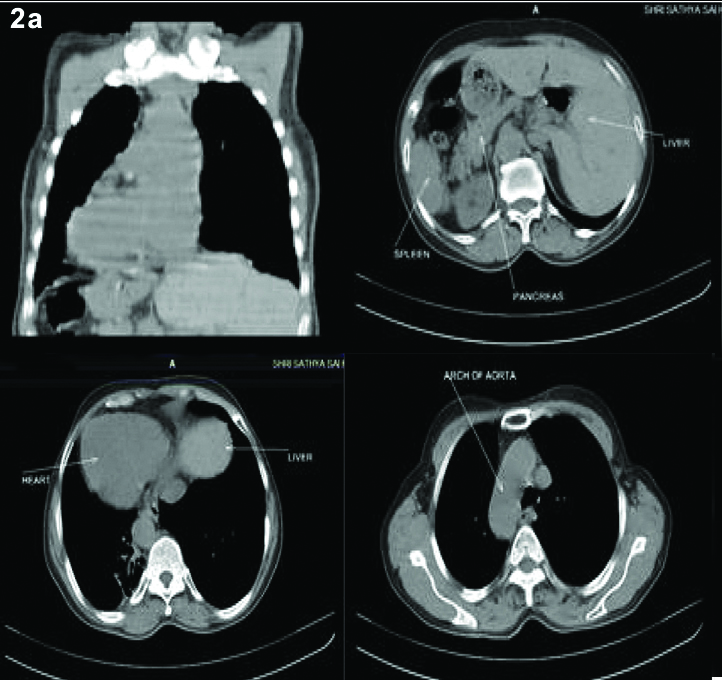
Cystic changes noted on right lower lobe (arrow).
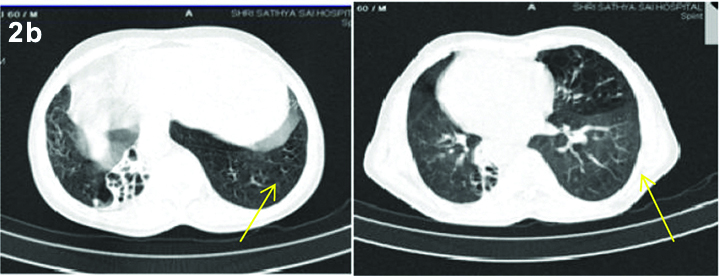
X-ray PNS hypoplastic frontal sinus bilateral.
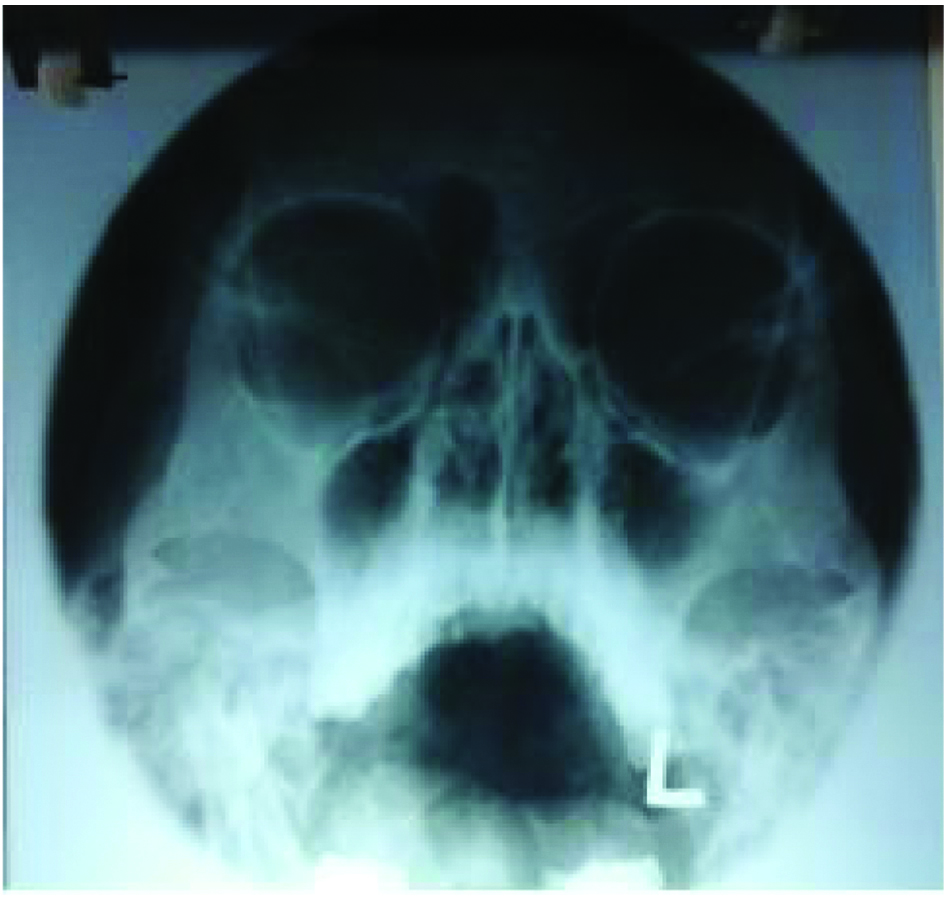
ECG with unreversed leads showing positive wave in aVR and tall R wave in V1 and absent R wave in V6.
Initially he was managed with antibiotics; Inj.Augmentin 1.2 gm IV BD with T.Levofloxacin 500 mg 1OD, Inj.Deriphylline 2 cc IV BD with Nebulisation, chest physiotherapy and postural drainage. He was clinically and symptomatically better after the above treatment and was discharged with oral antibiotics Tab.Ciprofloxacin 500 mg BD, mucolytics, metered dose inhaler combination of LABA and ICS. Patient was advised for follow up after 1 week. He was symptomatically better and had an improved quality of life. Subsequently family screening was done for one of his daughters using saccharin test which turned out to be normal.
Discussion
Bronchiectasis is a pathological description of lung characterized by inflamed and dilated thick walled bronchi from distal to terminal bronchi. Poor ciliary structure or function result in impaired clearance of mucus leading to bronchiectasis, PCD is characterised by chronic rhino sinusitis, chronic bronchial sepsis [1]. Structural or functional changes of cilia end up in poor clearance of mucus which may contribute to nasal polyposis, otitis media and chronic sinusitis, further leading to bronchiectasis [2]. Immotile cilia syndrome is an autosomal recessive disorder characterised by poor motility of cilia in airway and sperms. PCD is a disease characterised by change in ciliary beat pattern, ciliary beat frequency or both and has a heterogenous genetic basis. The prevalence of PCD ranges from 1:2,200 to 1:40,000 [3,4]. Investigations show the congenital defect in the cilia and sperm tail which cause chronic respiratory tract infection and male sterility [5]. In a study conducted on 12 men with PCD, six with dextrocardia, who presented with upper and lower respiratory tract infections; four had normal spermatozoa. The possible mechanism for this paradox could be associated with genetically mediated heterogeneity influencing the phenotypic presentation [1]. Normal respiratory cilia and spermatozoa with Kartagener’s syndrome explain the genetic heterogeneity and unreliable presentation of phenotype [6].
Subgroup of immotile cilia syndrome (Kartagener’s syndrome) is associated with situs inversus, chronic sinusitis, and bronchiectasis. Young’s syndrome, however is characterised by congenital epididymis obstruction with bronchiectasis and differs from immotile cilia syndrome by the absence of ultra structural cilial disorder [7,8]. The lower respiratory tract disease which is seen in young’s syndrome does not worsen without any attributable evidence of microbial culture; they mostly present with testicular dysfunction and normal sweat chloride test value [9]. Male patients with Kartagener’s syndrome invariably present infertility while women present reduced fertility. Most infertile patient with Kartagener’s syndrome have normal spermatozoic count, but with a structural defect and complete lack of motility [10].
PCD is a disease of serious threat for lung function, early diagnosis did not protect against decline in lung function. About 50% of males are sterile [11,12]. PCD/kartagener’s syndrome is usually associated with many complications which affect patient’s quality of life. Medical approach to the disease aims to prevent further progression of infections with an appropriate treatment and timely diagnosis which may help to delay the progression of lesion [13,14]. Mainstay of treatment for PCD involves airway clearance, infection control and different techniques that guarantee airway clearance including chest physiotherapy and postural drainage. More rapid, accurate, effective and economic means of diagnosis will be helpful in low resource settings [15,16].
Conclusion
Kartagener’s syndrome (PCD) is usually reported with infertility, but preserved fertility has been rarely reported. The cause of bronchiectasis must be searched meticulously especially in the setting of recurrent infection. The aim of reporting the case is a crude association between bronchiectasis with preserved fertility which is rarely seen in Kartagener’s syndrome.
[1]. Munro NC, Currie DC, Lindsay KS, Ryder TA, Rutman A, Dewar A, Fertility in men with primary ciliary dyskinesia presenting with respiratory infectionThorax 1994 49(7):684-87.10.1136/thx.49.7.6848066563 [Google Scholar] [CrossRef] [PubMed]
[2]. Madhuvan HS, Ravishankar SN, Kailash MS, Reddy SR T, A case of bronchiectasis with infertility. Primary ciliary DyskinesiaClinical Practice 2014 6(1):5 [Google Scholar]
[3]. Olm MA, Caldini EG, Mauad T, Diagnosis of primary ciliary dyskinesiaJornal Brasileiro de Pneumologia 2015 41(3):251-63.10.1590/S1806-3713201500000444726176524 [Google Scholar] [CrossRef] [PubMed]
[4]. Barthwal MS, Kartagener’s syndrome in a fertile male-An uncommon variantLung India 2006 23(3):12310.4103/0970-2113.44404 [Google Scholar] [CrossRef]
[5]. Eliasson R, Mossberg B, Camner P, Afzelius BA, The immotile-cilia syndrome: a congenital ciliary abnormality as an etiologic factor in chronic airway infections and male sterilityNew England Journal of Medicine 1977 297(1):1-6.10.1056/NEJM197707072970101301245 [Google Scholar] [CrossRef] [PubMed]
[6]. Fraser RS, Müller NL, Colman N, Pare PD, Fraser and Paré’s diagnosis of diseases of the chest 1999 Volumes 1-44th ditionWb Saunders:2281-2283. [Google Scholar]
[7]. Bandyopadhyay D, Bose S, Majumder S, Bandyopadhyay S, Young’s Syndrome: an uncommon cause of bronchiectasisJournal, Indian Academy of Clinical Medicine 2004 5(4):351-53. [Google Scholar]
[8]. Seaton A, Seaton D, Leitch AG, Crofton and Douglas’s Respiratory Diseases: 2 Volume Set 2004 Blackwell science:794-828. [Google Scholar]
[9]. Sangeeta A, Karande S, Limaye C, Dsouza R, Young syndromeBombay Hospital Journal 2011 53(3):672-73. [Google Scholar]
[10]. Mittal V, Shah A, Situs inversus totalis: The association of Kartagener’s syndrome with diffuse bronchiolitis and azoospermiaArchivos de Bronconeumología (English Edition) 2012 48(5):179-82.10.1016/j.arbr.2011.09.006 [Google Scholar] [CrossRef]
[11]. Marthin JK, Petersen N, Skovgaard LT, Nielsen KG, Lung function in patients with primary ciliary dyskinesia: A cross-sectional and 3-decade longitudinal studyAmerican Journal of Respiratory and Critical Care Medicine 2010 181(11):1262-68.10.1164/rccm.200811-1731OC20167855 [Google Scholar] [CrossRef] [PubMed]
[12]. Barbato A, Frischer T, Kuehni CE, Snijders D, Azevedo I, Baktai G, Primary ciliary dyskinesia: A consensus statement on diagnostic and treatment approaches in childrenEuropean Respiratory Journal 2009 34(6):1264-76.10.1183/09031936.0017660819948909 [Google Scholar] [CrossRef] [PubMed]
[13]. Kordus RJ, Price RL, Davis JM, Whitman-Elia GF, Successful twin birth following blastocyst culture of embryos derived from the immotile ejaculated spermatozoa from a patient with primary ciliary dyskinesia: a case reportJournal of Assisted Reproduction and Genetics 2008 25(9-10):437-43.10.1007/s10815-008-9254-x18855132 [Google Scholar] [CrossRef] [PubMed]
[14]. Chodhari R, Mitchison HM, Meeks M, Cilia, primary ciliary dyskinesia and molecular geneticsPaediatric Respiratory Reviews 2004 5(1):69-76.10.1016/j.prrv.2003.09.00515222957 [Google Scholar] [CrossRef] [PubMed]
[15]. Mirra V, Werner C, Santamaria F, Primary ciliary dyskinesia: an update on clinical aspects, genetics, diagnosis, and future treatment strategiesFrontiers in Pediatrics 2017 5:13510.3389/fped.2017.0013528649564 [Google Scholar] [CrossRef] [PubMed]
[16]. Sha YW, Ding L, Li P, Management of primary ciliary dyskinesia/Kartagener’s syndrome in infertile male patients and current progress in defining the underlying genetic mechanismAsian Journal of Andrology 2014 16(1):10110.4103/1008-682X.1949985753545 [Google Scholar] [CrossRef] [PubMed]