In the Western world, bladder cancer has been shown to be the fourth most common cancer in men and the eighth most common cancer in women [1]. Approximately, 70% of the bladder cancer cases are superficial and around 30% occur as MIBC, which may be associated with an increase in morbidity and mortality. Radical cystectomy followed by urinary diversion is known to be the best treatment for MIBC [2]. IC urinary diversion and ONB reconstruction are the two commonly employed treatment procedures for the treatment of patients with invasive bladder cancer.
However, IC urinary diversion and ONB reconstruction may have an effect on the HRQoL of patients. It has been shown that considerable changes occur in urinary, sexual and social functioning, daily living activities, and body image satisfaction [3]. Several studies have shown that patients treated with ONB had a better QoL compared to those treated with IC [2,4,5]. However, a few other studies have also shown that there is no significant difference in the outcome of either of the treatment [6,7]. The aim of this study was to compare the HRQoL of patients with MIBC who underwent IC with those who underwent ONB following radical cystectomy. The secondary objectives were to compare the financial burden of bladder cancer treatment between two types of urinary diversion, to educate patients and clinicians regarding the full spectrum of treatment outcome and facilitate medical decision making, and to assess overall treatment efficacy including subjective morbidity and oncological status.
Materials and Methods
This was a prospective longitudinal study conducted at tertiary care centre (Department of Urology, R.G. Kar Medical College and Hospital, Kolkata) between January 2015 and August 2017. Patients of either sex aged more than 18 years who underwent radical cystectomy followed by IC urinary diversion or ONB reconstruction for invasive bladder cancer were included in this study. Patients admitted in the urosurgery ward were screened and included if eligible. Patients with serum creatinine >2 mg/dL, chronic inflammatory bowel disease, history of previous bowel resection, tumour involvement at the bladder neck or prostatic urethra were excluded from the study. Patients were also excluded if they had any other oncological disorder, alcohol or drug abuse, or psychiatric illness.
Institutional Ethics Committee approved the study protocol. The study was conducted in accordance with the approved protocol and principles that have their origin in the Declaration of Helsinki. Individual written informed consent was obtained before any study-related procedures.
Demographic details, biochemical investigations, histopathology of the cystoprostatectomy (with lymph nodes) specimen, and details of adjuvant therapy and relapse were noted.
This was measured using the FACT-BL (version 4) Questionnaire [8]. The questionnaire contains 40 questions based on different domains (physical well-being, social/family well-being, emotional well-being, functional well-being and additional concerns). The QoL was evaluated preoperatively and at 6 and 12 months after surgery.
No formal sample size calculation was employed for this study. Statistical analysis was performed using SPSS software (Version 17, 2008). The data obtained were tabulated, analysed and presented using descriptive statistics-means (standard deviations) or as number (percentages).
Results
A total of 35 patients underwent radical cystectomy during the study period. An IC was constructed in 20 patients and 15 patients underwent ONB. One patient from the IC group and two patients from ONB group died. All three deaths resulted due to septicaemia.
Overall, the mean age at surgery was 55.63 and 54.46 years in the IC and ONB, respectively [Table/Fig-1]. All patients from ONB group were males; however, 78.95% of patients from the IC group were males. The mean time lag between TURBT and radical cystectomy was slightly higher in patients from the IC group (66.11 days vs. 50.23 days; p=0.314) than ONB group; similarly, the serum creatinine was also slightly higher in IC group (1.11 mg/dL vs 0.98 mg/dL). However, the mean duration of hospital stay after surgery was higher in ONB group than IC group (22.54 days vs. 16.00 days) [Table/Fig-1]. In both the groups, the majority of patients had tumour stage T2 with margin free; however, in IC group, a higher number of patients had a positive margin.
Demographics and clinical characteristics.
| Parameter | Ileal conduit n=19 | Orthotopic neobladder n=13 |
|---|
| Age at surgery (years), mean (SD) | 55.63 (7.49) | 54.46 (6.57) |
| Males n (%) | 15 (78.95) | 13 (100.00) |
| BMI (kg/m2), mean (SD) | 22.54 (1.90) | 22.69 (1.67) |
| Time lag between TURBT and radical cystectomy (days), mean (SD) | 66.11 (50.33) | 50.23 (28.91) |
| Serum creatinine (mg/dL), mean (SD) | 1.11 (0.14) | 0.98 (0.17) |
| Neo-adjuvant chemotherapy, n (%) | 4 (21.05) | 2 (15.38) |
| Comorbidities, n (%) |
| Hypertension | 5 (26.32) | 2 (15.38) |
| Diabetes mellitus | 2 (10.53) | 0 |
| Hospital stay after surgery, mean (SD) | 16.00 (1.67) | 22.54 (10.59) |
| Classification (tumour stage), n (%) |
| T2, Margin free | 14 (73.68) | 10 (76.92) |
| No residual | 1 (5.26) | 3 (23.08) |
| T3 | 3 (15.78) | 0 |
| T4a | 1 (5.26) | 0 |
| Positive lymph node, n (%) | 8 (42.11) | 2 (15.38) |
BMI: Body mass index; SD: Standard deviation; TURBT: Transurethral resection of bladder tumour
Wound infection was the most common complication (ONB group, 46.15%; IC group, 21.05%) followed by paralytic ileus (ONB group, 23.07%; IC group, 10.53%) and urine leakage (ONB group, 23.07%; IC group, 10.53%). Pneumonia occurred in 23.07% of patient in ONB group and 31.57% of patient in IC group. ONB leak was reported in one patient due to the intrusion of the abdominal drain inside the neobladder. It was detected cystoscopically and was removed. Complications based on Clavien-Dindo classification [9] were reported in four patients in IC group (grade 1, n=3; grade 3B, n=1) and in 8 patients in ONB group (grade 1, n=5; grade 3A, n=2; grade 3B, n=1).
A total of 10.53% patient from ONB group and 47.37% of patients from the IC group received adjuvant chemotherapy.
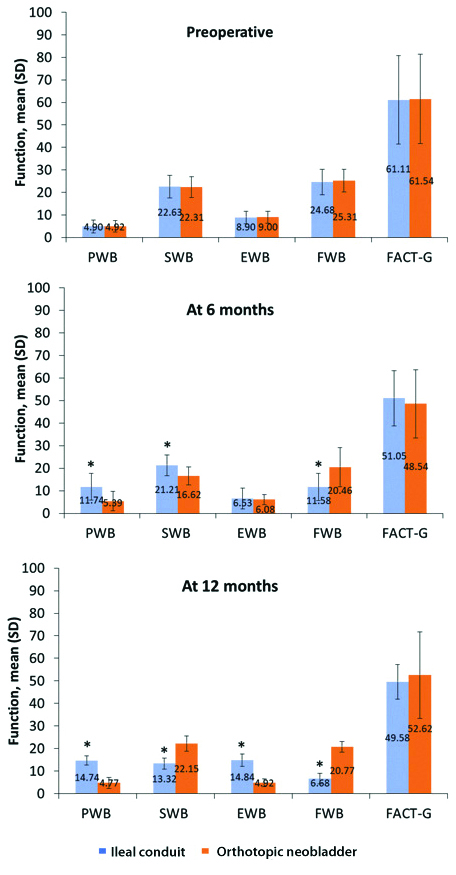
Preoperatively the mean FACT-G score in patients from the IC group and ONB group was 61.11 and 61.54, respectively, showing no significant differences [Table/Fig-2]. The bladder cancer subscale scores were similar in both groups. The patients from the IC group had significantly higher physical well-being score than the ONB group at both 6 and 12 months. The social well-being score was higher at 6 months in the IC group compared to ONB which was reversed at 12 months. At the end of 6 months both the group had similar emotional well-being score but after 12 months ONB group had a lower score in comparison to the IC group. The functional well-being score was higher in the ONB group at both 6 and 12 months compared to IC group. All the differences have been found to be statistically significant except the score of emotional well-being at 6 months [Table/Fig-2].
Difference in FACT-BL between Ileal conduit and orthotopic neobladder groups: a) preoperative; b) at 6 months; and c) at 12 months.
EWB: Emotional well-being; FACT-BL: Functional assessment of cancer therapy-bladder; FACT-G: Functional assessment of Cancer therapy-general; FWB: Functional well-being; PWB: Physical well-being; SD: Standard deviation; SWB: Social/family well-being.
*p<0.0001 between Ileal conduit and orthotopic neobladder groups
Seventeen (89.47%) of 19 patients from IC group answered ‘no trouble at all in controlling urine’, compared to six (46.15%) of 13 patients from ONB group at 12 months whereas at 6 months 16 patients from the IC group did not have any problem compared to 3 patients from ONB group [Table/Fig-3]. However, 10 patients with an IC reported that they did not like the appearance of their bodies at all after 6 months which was reduced to 8 people at 12 months, compared with only one (7.69%) patient at 6 months with an ONB. Patients with an IC had a significantly worse QOL score regarding their body image than those with an ONB. Eleven (57.89%) of IC patients and 8 (61.54%) of ONB patients did not report diarrhea. Sixteen (84.21%) patients from IC group and eight (61.53%) patients from ONB group had no interest in sex at all.
Answer to each bladder-cancer subscale questions (FACT-BL questionnaire).
| Questions | Group | 6 months | 12 months |
|---|
| Not at all | A little bit | Some what | Quite a bit | Very much | Not at all | A little bit | Some what | Quite a bit | Very much |
|---|
| BL1: I have trouble controlling my urine | IC | 16 | 1 | 2 | 0 | 0 | 17 | 2 | 0 | 0 | 0 |
| ONB | 3 | 6 | 4 | 0 | 0 | 6 | 1 | 4 | 2 | 0 |
| C2: I am losing weight | IC | 3 | 5 | 5 | 3 | 3 | 6 | 6 | 5 | 2 | 0 |
| ONB | 6 | 3 | 2 | 2 | 0 | 6 | 3 | 2 | 2 | 0 |
| C3: I have control of my bowels | IC | 11 | 0 | 6 | 2 | 0 | 15 | 2 | 2 | 0 | 0 |
| ONB | 6 | 0 | 5 | 2 | 0 | 6 | 3 | 4 | 0 | 0 |
| BL2: I urinate more frequently than usual | IC | NA | NA |
| ONB | 10 | 1 | 1 | 2 | 0 | 10 | 2 | 1 | 0 | 0 |
| C5: I have diarrhea | IC | 11 | 3 | 5 | 0 | 0 | 11 | 3 | 5 | 0 | 0 |
| ONB | 8 | 2 | 3 | 0 | 0 | 8 | 2 | 3 | 0 | 0 |
| C6: I have a good appetite | IC | 0 | 7 | 4 | 2 | 6 | 3 | 5 | 6 | 4 | 1 |
| ONB | 0 | 1 | 2 | 2 | 8 | 2 | 3 | 5 | 2 | 1 |
| C7: I like the appearance of my body | IC | 10 | 2 | 4 | 3 | 0 | 8 | 4 | 4 | 1 | 2 |
| ONB | 1 | 1 | 1 | 2 | 8 | 0 | 0 | 2 | 3 | 8 |
| BL3: It burns when I urinate | IC | NA | NA |
| ONB | 8 | 2 | 2 | 1 | 0 | 8 | 3 | 2 | 0 | 0 |
| BL4: I am interested in sex | IC | 16 | 1 | 2 | 0 | 0 | 16 | 1 | 2 | 0 | 0 |
| ONB | 8 | 2 | 2 | 1 | | 8 | 2 | 2 | 1 | 0 |
| BL5: (For men only) I am able to have and maintain an erection | IC | 13 | 2 | 0 | 0 | 0 | 13 | 2 | 0 | 0 | 0 |
| ONB | 10 | 1 | 2 | 0 | 0 | 10 | 1 | 2 | 0 | 0 |
| C8: I am embarrassed by my ostomy appliance | IC | 1 | 2 | 2 | 7 | 7 | 1 | 2 | 2 | 7 | 7 |
| ONB | - | - | - | - | - | - | - | - | - | - |
| C9: Caring for my ostomy appliance is difficult | IC | 5 | 5 | 1 | 2 | 6 | 5 | 5 | 1 | 2 | 6 |
| ONB | - | - | - | - | - | - | - | - | - | - |
IC: Ileal conduit; ONB: Orthotopic neobladder
The financial difficulty was found to be immense in the IC group. The IC group patients had to incur about Rs 450 per week on the urostomy bag extra which found to be absent in the ONB group (patients of IC group had to pay as it is not supplied by the authority).
At 6 months, the average bladder capacity was 350 mL, Peak Flow Rate (Qmax) was 14.5 mL/s and Post Void Residual (PVR) was 70 mL. At 12 months the average bladder capacity was 360 mL, Qmax 15.2 mL/s and PVR decreased by 10 mL. Intermittent self-catheterization was needed in six patients (46.15%). None of the patient’s urine cytology was positive on follow-up. One patient in the IC group had a recurrence at 13 months of follow-up which presented with bleeding per meatus confirmed by urethroscopy. The radiological tests on scheduled did not show any recurrence. Among late compilations, incisional hernia (n=2), renal deterioration (n=2) and pyelonephritis (n=1) were reported in patients from IC group; and incisional hernia (n=1) and urinary retention (n=2) in patients from ONB group at 12 months.
Discussion
Radical cystectomy and urinary diversion are among the commonly used treatment modalities for patients with MIBC. In this study, we compared the HRQoL of patients with MIBC who underwent IC with those who underwent ONB after radical cystectomy. In contrast to most of the previous studies that were retrospective and cross-sectional, in the present study, the FACT-BL questionnaire was filled by the patients preoperatively (baseline) and then at 6 and 12 months after surgery. One of the limitations of retrospective studies lies in selection bias, where the patient’s preoperative health status may have been different before cystectomy, and this may have affected the choice of diversion. Another limitation of these studies is that the QoL was measured only once after the procedure; however, few measured them longitudinally [10-14]. In the present study, the QoL was evaluated before and at regular timepoints after the procedure. Overall, the patient groups in this study were similar to that in previous studies. Since only four women survived in the IC group, a separate analysis was not done for this cohort because the results would not have been clinically meaningful and significant. In a study by Gacci M et al., comparable outcomes were observed in women between IC and ONB [15].
The FACT-BL questionnaire is a common questionnaire used to assess QoL in patients with bladder cancer who have undergone urinary diversion. In the present study, we used the English version of FACT-BL questionnaire. The total FACT-G score did not show significant differences between the two groups preoperatively. In contrast, patients of the IC group had a higher physical well-being score than those in the ONB group at both 6 and 12 months after surgery. All the differences were statistically significant except the score for emotional well-being at 6 months. Kikuchi E et al., did not report differences in the four categories of FACT-G between the groups [16]. However, Fujisawa M et al., who used the Short-Form-36 questionnaire, also report better physical functioning in patients who underwent ONB reconstruction than those who underwent IC diversion [17]. In a prospective study by Singh V et al., who used the QLQ-C30 questionnaire, significantly better physical, role, social functioning and global health status/QoL was observed in patients with ONB throughout the first 18 months postoperatively compared with those who had IC formation [2].
We found that our patients with an IC had significantly less trouble controlling urine than those with an ONB, which is in agreement with previous studies [18,19]. Better stoma appliances and postoperative care by a skilled stoma therapist could have reduced the stoma-related problems. One of the common findings in patients with ONB is some degree of urinary leakage, especially at night [20].
In the present study, nearly all patients agreed to being embarrassed by the ostomy and the majority of the patients had difficulty in taking care of the appliance. It has been reported earlier that patients with IC may have concerns related to body image and owing to this around half of the patients feel uncomfortable with such change [21].
Generally, Studer neobladder initially has a capacity of 150 mL and later it increases up to 360 mL at around 12 months [22]. In our study, we did not observe significant metabolic acidosis since the patients were given sodium bicarbonate powder in the early postoperative period and also because the shorter ileal segment was taken. Wound infection, followed by paralytic ileus, were the most common complications encountered in both the groups in our study. The complication rate in both the groups was comparable. Urine leak was significantly less due to early bladder wash by the diluted sodium bicarbonate solution. Daytime continence was 55%-65% at 12 months, which was increased by kegel exercise. Night-time continence was significantly enhanced to 40%-50% by advising the patient to pass urine once at midnight.
In our study, the stoma complication was not appreciable due to meticulous technique, whereas the incidence of complications like incisional hernia was comparable in both groups. Pyelonephritis and renal deterioration were observed in the IC group and urinary retention was observed in the ONB group. Disease recurrence during follow-up is known to affect QoL. In the present study, one patient from the IC group reported disease recurrence. However, this single finding might not have an impact on the comparison of QoL in IC and ONB groups.
Limitation
Authors acknowledge the few limitations of the study including small sample size and that the study was non-randomized. It was possible to perform this comparative study on the QoL of patients with IC and ONB using the FACT items, which is more specific to cystectomy and different urinary diversions.
Conclusion
Results from this study demonstrated that ONB had a better QoL than the IC group. This study will facilitate the clinicians to educate the patients about the choice of diversion on the background of the data available in the study.
BMI: Body mass index; SD: Standard deviation; TURBT: Transurethral resection of bladder tumour
IC: Ileal conduit; ONB: Orthotopic neobladder