Recurrent Stroke in a Young Adult due to Antiphospholipid Antibody Syndrome-A Case Report
Siraveni Thirupathi1, Dinesh Ragav2, Nasreen Begum3
1 Postgraduate, Department of General Medicine, Shri Sathya Sai Medical College and Research Institute, Kancheepuram, Tamil Nadu, India.
2 Assistant Professor, Department of General Medicine, Shri Sathya Sai Medical College and Research Institute, Kancheepuram, Tamil Nadu, India.
3 Professor, Department of General Medicine, Shri Sathya Sai Medical College and Research Institute, Kancheepuram, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dinesh Ragav, Assistant Professor, Shri Sathya Sai Medical College and Research Institute, Ammapetti, Nellikuppam, Sembakkam (Taluka), Kancheepuram, Tamil Nadu, India.
E-mail: drthiruyadav@gmail.com
Antiphospholipid Syndrome (APS) is an autoimmune disease characterised by arterial thrombosis, venous thromboembolic complications, mild to moderate thrombocytopenia and/or pregnancy morbidities in the presence of persistently positive levels of antiphospholipid antibodies (aPL) such as Lupus Anticoagulant (LA), anticardiolipin (aCL), and anti-β2-glycoprotein-I (aβ2GPI) antibodies. Many mechanisms create a prothrombotic state, it is prone to complication like abortions, preterm deliveries, foetal loss, cerebral stroke, acute coronary syndrome, venous thromboembolic and peripheral vascular occlusive disorders, intracerebral haemorrhage, encephalopathy and infections. Here, the case of a 42-year-old female is being reported, who was diagnosed with APS, treated with warfarin. The available knowledge about this disease and its relevance to the symptoms of the patient is also summarised.
Lupus anticoagulant, Procoagulable state, Thromboembolic events
Case Report
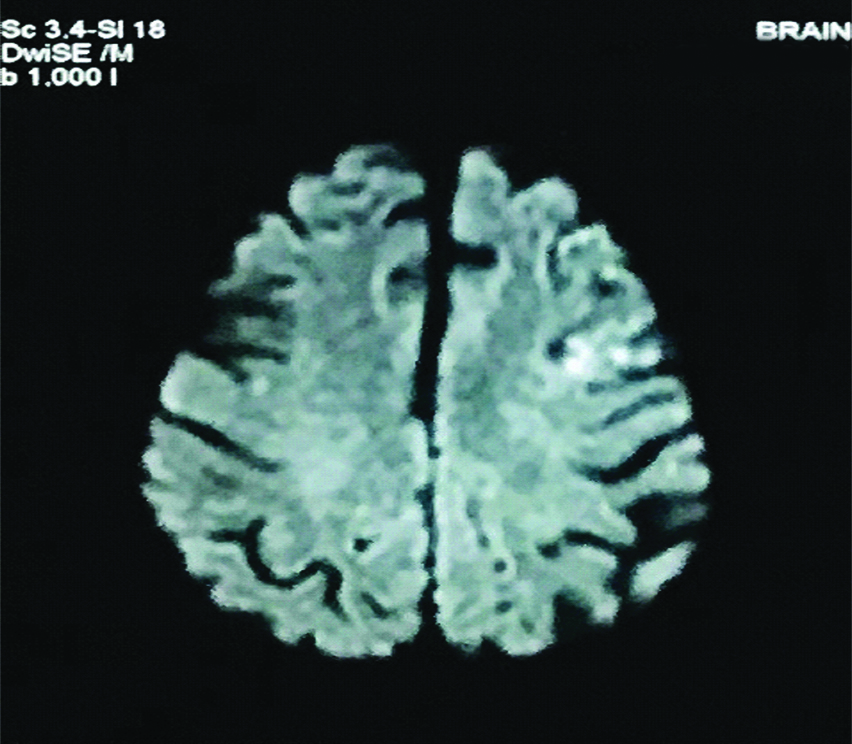
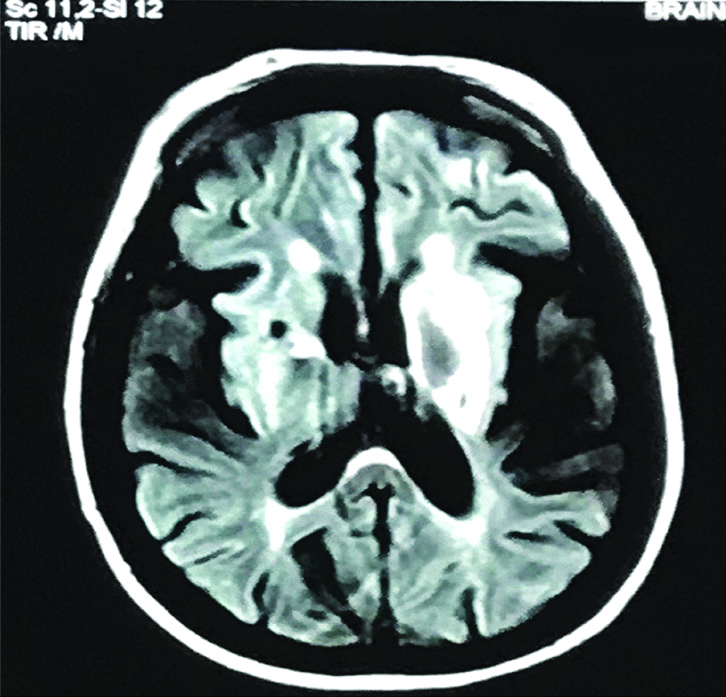
A 42-year-old married female was brought to our emergency department with a history of difficulty in speech and one episode of involuntary micturition since one day. She had a history of Cardio Vascular Accident (CVA) with right hemiparesis at the age of 37 years. She was on tab aspirin 75 mg OD, but took medicine irregularly. Mother of two healthy children, there was no history of abortions, preterm deliveries and foetal deaths. On examination, patient was conscious, obeying oral commands but aphasic, Central Nervous System (CNS) examination revealed spastic contraction with power 3/5 and exaggerated deep tendon reflexes on right upper and lower limbs. Babinski sign was positive on right plantar. She had circumduction gait. Other systems were normal. Vitals were normal. We suspected a recurrent CVA and did emergency CT scan. It showed sub acute infarct in the left middle and inferior frontal gyrus, and left parietal lobe, chronic infarct in the left corona radiata, centrum semiovale and left lentiform nucleus, chronic infarct in the right caudate nucleus, internal capsule and lentiform nucleus with ex vacuo dilatation of lateral ventricle, lacunar infarct in left thalamus and atrophic changes in cerebral brain parenchyma. MRI brain showed sub acute infarct in left parietal [Table/Fig-1] and chronic infarct in left occipital lobes, b/l basal ganglia [Table/Fig-2] and left thalamus, small vessel ischaemic disease in the bilateral corona radiata, hypo plastic left transverse and sigmoid sinuses. These findings suggested that she had a recurrent episode of CVA. Hence we screened her for procoagulable state. Patient was admitted and started on tab aspirin 75 mg along with supportive management. Echocardiography was normal. Carotid doppler showed bilateral media thickness and normal intima without hemodynamic abnormalities. Doppler of bilateral vertebral arteries was normal. Venereal Disease Research Laboratory (VDRL) test, serological tests were negative, Anti ds DNA-negative, Anti nuclear antibody-negative, ESR-60 mm/hr, Platelet count-2.7 l, PT-13.6 sec, INR-1.01, APTT-58 sec. Pro coagulation results revealed lupus anticoagulant LA1 (59.6 sec), LA2 (45.1 sec) and LA1/LA2 (1.32) ratio elevated, anti cardiolipins antibodies (against cardiolipins substance) IgM and IgG, aPL (against β2-glycoprotein I) IgM and IgG were normal and antithrombin was elevated, protein C and protein S and homocystein were normal. Above investigations when repeated after three months, derived same results.
Diffusion-weighted imaging-Subacute infarct in left parietal lobe.
FLAIR-Chronic infarct in b/l basal ganglia.
Discussion
Antiphospholipid Syndrome (APS) [1] was first coined in 1980s. It is an autoimmune disorder identified by the presence of venous thromboembolism, arterial thrombotic complications, and/or pregnancy morbidities with the persistent presence of antiphospholipid antibodies (aPL) [2] such as lupus anticoagulant, anticardiolipin, and anti-β2-glycoprotein-I antibodies as per revised Sapporo criteria [3]. Among several types of aPL [4], lupus anticoagulant [5] has been shown to be the strongest risk factor for thrombosis. Repeat test 12-week apart is important, because transient aPL test is positive in some infections and medications [6]. APS Patients, compared to normal individuals are at high risk for atherosclerosis, myocardial infarction, valvular heart disease and stroke. Vascular endothelial cell dysfunction and subsequent complement proteins activation by aPL plays a major role in the pathogenesis of APS [7]. New research studies on APS found the pathogenesis of APS at molecular level. It is very helpful to know risk stratification and provide new therapeutic targets at molecular level. Pyo JY, et al., studied 99 ischaemic stroke patients with minimum one of the antiphospholipid or more antiphospholipid antibodies positivity. They divided the patients into two groups by the laboratory diagnostic criteria for APS, who did not fulfill the criteria as “definite APS” and who not fulfilled the criteria as “indefinite APS”. In these two groups, they compared the risk of subsequent thrombotic events. They used, Cox proportional hazards model and Kaplan Meier survival curves for the analyses. There was no much difference of increased risk for subsequent episodes of strokes or other thromboembolic events with definite APS, compared with indefinite APS group [8]. Delgado MG et al., reported a case of 77-year-old female who presented with language difficulties and history of multiple ischaemic stroke events in the last three years and the incidents of these stroke events were accredited to the cardiac emboli aetiology (atrial fibrillation). On subsequent stroke, the pro-coagulation profile test revealed lupus anticoagulant, anti-β2-glycoprotein and anticardiolipin antibodies positivity and diagnosed as APS [9]. APS is mainly seen in the younger patient population. There are few studies in literature documenting APS in elderly. A cohort study by Euro Phospholipid project group was conducted on 1000 patients, 12.7% of patients reported as older onset (onset after the age of 50) APS [10,11]. Management of APS and prevention of further complications is a challenge for clinicians. During the 14th International Congress the Trends Task Force recommended that vitamin K antagonists (VKAs-warfarin) should be the drug of choice in thrombotic APS, unless there are specific contraindications such as allergy, intolerance, or documented poor efficacy [12]. The use of Newer Oral-Anticoagulants (NOACs) safety and efficacy in the management of APS may need more clinical trials to get additional clarity [13,14]. A case reported by Joshi et al., on recurrent thrombosis in patients with APS receiving newer oral anticoagulants conclude that treatment strategies for APS should be tailored cautiously when using NOACs [15].
This is a documented case of recurrent strokes in young age, the presence of lupus anticoagulant antibodies without pregnancy morbidities. As per Revised Sapporo classification criteria for diagnosis of antiphospholpid antibody syndrome, the presence of at least one of the clinical criteria (vascular thrombosis and/or pregnancy morbidity) and at least one of the laboratory criteria (detection of lupus anticoagulant, anticardiolipins, or anti-β2-glycoprotein-I antibodies) is required. This case was diagnosed as recurrent stroke in young adult due to antiphospholipid antibody syndrome. Tablet warfarin was started at 2 mg per day and titrated to 3 mg/day to a target INR of 2-3. On admission her aphasia has recovered completely. She was counselled for lifelong anticoagulation and the risk of bleeding and need regular follow-up with PT and INR report.
Conclusion
In conclusion, when there are clinical symptoms such as recurrent arterial and venous occlusive events and/or recurrent foetal loss, without any underlying known clinical conditions causing thrombosis, the clinicians should suspect APS and investigate for aPL, as early diagnosis may influence the course of the disease. Finally, management of APS that involves prevention of thrombosis together with close monitoring of the patient on an anticoagulant could be quite challenging. Therefore, patient should get educated about the drug compliance, periodic monitoring, and prevention of thrombosis is indispensable.
[1]. Hughes GR, The antiphospholipid syndrome: ten years onLancet 1993 342:341-44.10.1016/0140-6736(93)91477-4 [Google Scholar] [CrossRef]
[2]. Vila P, Hernández MC, López-Fernández MF, Batlle J, Prevalence, follow-up and clinical significance of the anticardiolipin antibodies in normal subjectsThromb Haemost 1994 72:209-13.10.1055/s-0038-16488407831653 [Google Scholar] [CrossRef] [PubMed]
[3]. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS)J Thromb Haemost 2006 4:295-306.10.1111/j.1538-7836.2006.01753.x16420554 [Google Scholar] [CrossRef] [PubMed]
[4]. Htet A, Hayes L, Leung T, Strong lupus anticoagulant (LA) as a cause for prolonged prothrombin time (PT), activated partial thromboplastin time (APTT) and abnormally low intrinsic factor (IF) levelsPathology 2015 47:S9010.1097/01.PAT.0000461585.89264.ae [Google Scholar] [CrossRef]
[5]. Pengo V, Tripodi A, Reber G, Rand JH, Ortel TL, Galli M, Update of the guidelines for lupus anticoagulant detectionJournal of Thrombosis and Haemostasis 2009 7(10):1737-40.10.1111/j.1538-7836.2009.03555.x19624461 [Google Scholar] [CrossRef] [PubMed]
[6]. Lim W, Antiphospholipid syndromeHematology Am Soc Hematol Educ Program 2013 2013:675-80.10.1182/asheducation-2013.1.67524319251 [Google Scholar] [CrossRef] [PubMed]
[7]. Corban MT, Duarte-Garcia A, McBane RD, Matteson EL, Lerman LO, Lerman A, Antiphospholipid syndrome: role of vascular endothelial cells and implications for risk stratification and targeted therapeuticsJournal of the American College of Cardiology 2017 69(18):2317-30.10.1016/j.jacc.2017.02.05828473138 [Google Scholar] [CrossRef] [PubMed]
[8]. Pyo JY, Jung SM, Lee SW, Song JJ, Lee SK, Park YB, Subsequent Thrombotic Outcomes in Patients with Ischemic Stroke with Antiphospholipid Antibody PositivityYonsei Medical Journal 2017 58(6):1128-34.10.3349/ymj.2017.58.6.112829047236 [Google Scholar] [CrossRef] [PubMed]
[9]. Delgado MG, Rodríguez S, García R, Sánchez P, Sáiz A, Calleja S, Antiphospholipid syndrome of late onset: a difficult diagnosis of a recurrent embolic strokeJournal of Stroke and Cerebrovascular Diseases 2015 24(8):e209-11.10.1016/j.jstrokecerebrovasdis.2015.04.01625979425 [Google Scholar] [CrossRef] [PubMed]
[10]. Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, Brey R, Crowther M, Derksen R, Evidence based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International congress on antiphospholipid antibodiesLupus 2011 20(2):206-18.10.1177/096120331039580321303837 [Google Scholar] [CrossRef] [PubMed]
[11]. Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA, Antiphospholipid syndromeLancet 2010 376(9751):1498-509.10.1016/S0140-6736(10)60709-X [Google Scholar] [CrossRef]
[12]. Erkan D, Aguiar CL, Andrade D, Cohen H, Cuadrado MJ, Danowski A, 14th International Congress on Antiphospholipid Antibodies: task force report on antiphospholipid syndrome treatment trendsAutoimmun Rev 2014 13:685-96.10.1016/j.autrev.2014.01.05324468415 [Google Scholar] [CrossRef] [PubMed]
[13]. Cohen H, Hunt BJ, Efthymiou M, Arachchillage DRJ, Mackie IJ, Clawson S, RAPS trial investigators. Rivaroxaban versus warfarin to treat patients with thrombotic antiphospholipid syndrome, with or without systemic lupus erythematosus (RAPS): a randomised, controlled, open-label, phase 2/3, noninferiority trialLancet Haematol 2016 3:e426-36.10.1016/S2352-3026(16)30079-5 [Google Scholar] [CrossRef]
[14]. Pengo V, Banzato A, Bison E, Zoppellaro G, Padayattil Jose S, Denas G, Efficacy and safety of rivaroxaban vs warfarin in high-risk patients with antiphospholipid syndrome: Rationale and design of the Trial on Rivaroxaban in AntiPhospholipid Syndrome (TRAPS) trialLupus 2016 25:301-06.10.1177/096120331561149526466613 [Google Scholar] [CrossRef] [PubMed]
[15]. Joshi A, Hong J, Siva C, Recurrent thrombosis in patients with antiphospholipid syndrome receiving newer oral anticoagulants: A case report and review of literatureClinical Medicine & Research 2017 15(1-2):41-44.10.3121/cmr.2017.134928751467 [Google Scholar] [CrossRef] [PubMed]